A 28-year-old Caucasian woman presented to an outside hospital in May 2011 with a 1-year history of right hip and pelvic pain. Radiographs, computed tomography (CT), and magnetic resonance imaging (MRI) showed a lytic, expansile lesion involving the posteroinferior pelvis, measuring 9 × 9 × 10 cm (Figs. 1 and 2). In June 2011 a CT-guided, percutaneous needle biopsy was performed (Fig. 3). The patient began denosumab therapy at 120 mg/month for 9 months and then continued with 120 mg every 2 months for another 11 months. MRI performed biannually throughout this period showed that the lesion was stable or resolving.
The patient subsequently developed right groin and ischial pain. On examination, she had excellent hip range of motion, with tenderness over the ischium and superior pubic ramus. Radiographs demonstrated a mixed lytic and sclerotic lesion (Fig. 4). In comparison with the original imaging studies, the previous purely lytic lesion had become sclerotic and smaller (6 × 6 × 7 cm). In September 2013, the lesion was removed by complete excision of the inferior mass, curettage, and high-speed burring of the superior pubic ramus and posterior column, thereby preserving the hip joint. The specimen was found to be heavily ossified throughout. Histologic examination showed small nests of mononuclear cells embedded in densely hyalinized fibrous tissue, as well as embolization spherules (Fig. 5).
Three months later, she had minimal discomfort and excellent hip function, with no radiographic evidence of recurrence (Fig. 6). After 7 months, however, she developed worsening hip pain and weight loss. Radiographs showed interval development of a lytic lesion in the superolateral acetabulum with a mineralized soft-tissue mass (Fig. 7). CT studies showed a destructive lesion measuring 7 × 11 × 12 cm, as well as multiple lung nodules.
The patient began methotrexate, cisplatin, and doxorubicin therapy. After 2 months of this regimen, she reported no substantial pain relief; both the pelvic and lung disease had progressed. A palliative right hemipelvectomy was performed. The specimen consisted of a soft-tissue mass associated with diffuse intraosseous tumor (Fig. 8). Postoperatively, a regimen consisting of gemcitabine and docetaxel was initiated, but the treatment failed and the patient died 3 months later.
The patient was diagnosed with malignant transformation (osteosarcoma) of denosumab-treated giant cell tumor of bone.
Proceed to Discussion >>Reference: Park A, Cipriano CA, Hill K, Kyriakos M, McDonald DJ. Malignant transformation of a giant cell tumor of bone treated with denosumab: A case report. JBJS Case Connect. 2016 Sep 28;6(3):e78.
Malignant transformation develops in <5% of giant cell tumors (GCTs) of bone and almost always occurs in response to radiation therapy. To the best of our knowledge, <30 cases of malignant transformation in the absence of radiation have been reported in the literature. These “evolutionary” malignancies typically developed after several local recurrences and symptom-free periods averaging 9.9 years. These are distinct from “primary” malignant GCTs of bone in which malignant stromal cells are juxtaposed or intermixed with an otherwise benign GCT of bone at initial presentation. Our patient received 20 months of denosumab therapy for a benign GCT of bone, stopped taking denosumab for 7 months, and then underwent surgical resection, at which time there was no histologic evidence of malignancy. In the 7 months following resection, she developed osteosarcoma at the site of the original tumor as well as in the lungs.
Denosumab has shown promise as a treatment for GCT of bone. In a Phase-2 prospective trial, denosumab was found to halt disease progression in 162 (96%) of 169 patients with unresectable GCT of bone at a median follow-up of 13 months. However, 2 patients in this trial developed sarcomatous transformation; the authors suggested that one was actually present at baseline and the other was unrelated to denosumab, but gave no additional explanation of their reasoning. Aponte-Tinao et al. reported the case of a patient with a proximal tibial GCT that repeatedly recurred despite intralesional and then en bloc resections over 3.8 years. They initiated denosumab therapy at that point to limit future recurrences, but 13 months later the mass was found to have transformed into a high-grade pleomorphic sarcoma. Additionally, Broehm et al. described 2 cases of benign GCTs of bone that recurred soon after surgical resection. Denosumab was initiated 6 and 9 years after the resections because of the progression of the recurrent disease, and the patients initially responded well; however, they were diagnosed with metastatic osteosarcoma 8 and 30 months later, respectively.
The cellular effects of denosumab on GCT of bone are currently under investigation. Mak et al. examined specimens from 2 patients with GCTs of bone treated with denosumab for 6 months, and reported that the stromal cell population persisted despite complete elimination of the giant cells. However, based on histologic analysis of specimens from 20 patients with GCTs of bone treated with denosumab from 3 to 7 months, Branstetter et al. suggested that denosumab decreases the giant cell and stromal cell populations and induces differentiation of the latter into woven bone. Similarly, Hakozaki et al. examined a specimen from a patient with GCT of bone treated with denosumab for 6 months and found reactive bone but no giant cells or stromal cells. Wojcik et al. reported that denosumab induced atypia and bone deposition that resembled osteosarcoma in 9 patients with benign GCT of bone, but none of these patients had a clinical course consistent with malignancy. Histologic analysis of our patient’s pelvic specimen after treatment with denosumab for 20 months showed reactive changes, bone, and rare foci of residual degenerated GCT. While we do not know what findings might be attributed to the single attempt at embolization that our patient underwent, Emori et al. reported that serial embolization of GCT of bone induces peripheral tumor ossification, but residual viable GCT remains. Because we found no viable GCT of bone, we feel that denosumab, not embolization, played a major role in inducing the changes we observed.
To our knowledge, this is the first case of a patient with GCT of bone that underwent malignant transformation after being treated initially with denosumab therapy and subsequently with surgical resection. There was no evidence of osteosarcoma either on the initial biopsy or after extensive examination of the initially resected specimen. Furthermore, the initial tumor was pretreated with only embolization and denosumab, and a high-grade osteosarcoma would not respond to this regimen. Speculation regarding the mechanism of such a transformation is beyond the scope of this case report, and it is not possible to imply a direct cause-and-effect relationship between denosumab and malignant transformation in our patient. Nevertheless, this phenomenon has now been reported several times, particularly in patients with multiple recurrences and prolonged disease courses. We believe that this critically adverse outcome warrants close follow-up if denosumab is used in the treatment of GCT of bone.
Reference: Park A, Cipriano CA, Hill K, Kyriakos M, McDonald DJ. Malignant transformation of a giant cell tumor of bone treated with denosumab: A case report. JBJS Case Connect. 2016 Sep 28;6(3):e78.
What is the diagnosis?
Malignant giant cell tumor of bone
Malignant transformation (osteosarcoma) of denosumab-treated giant cell tumor of bone
Dedifferentiated chondrosarcoma
Diffuse, tenosynovial giant cell tumor
Synovial sarcoma

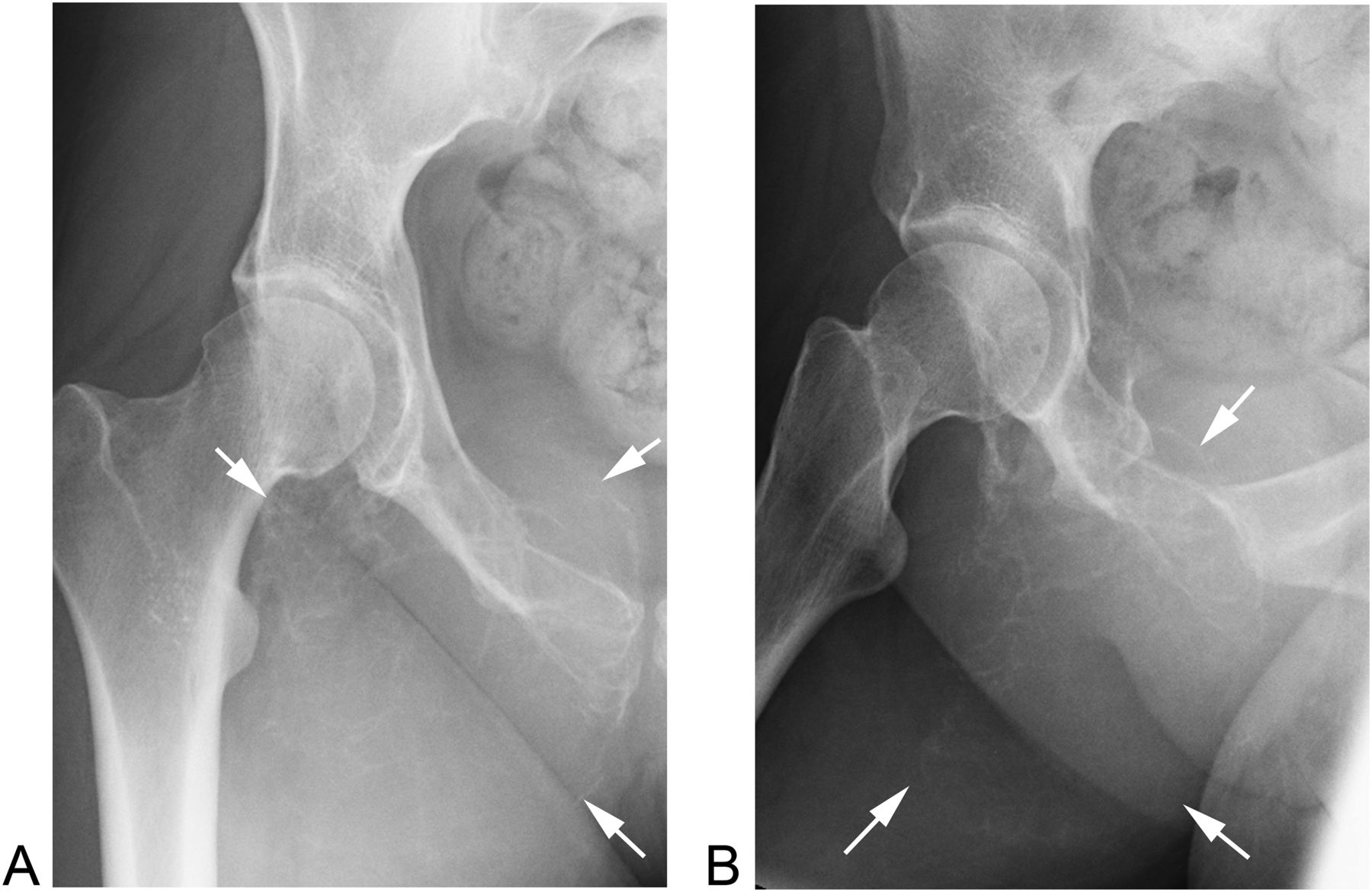
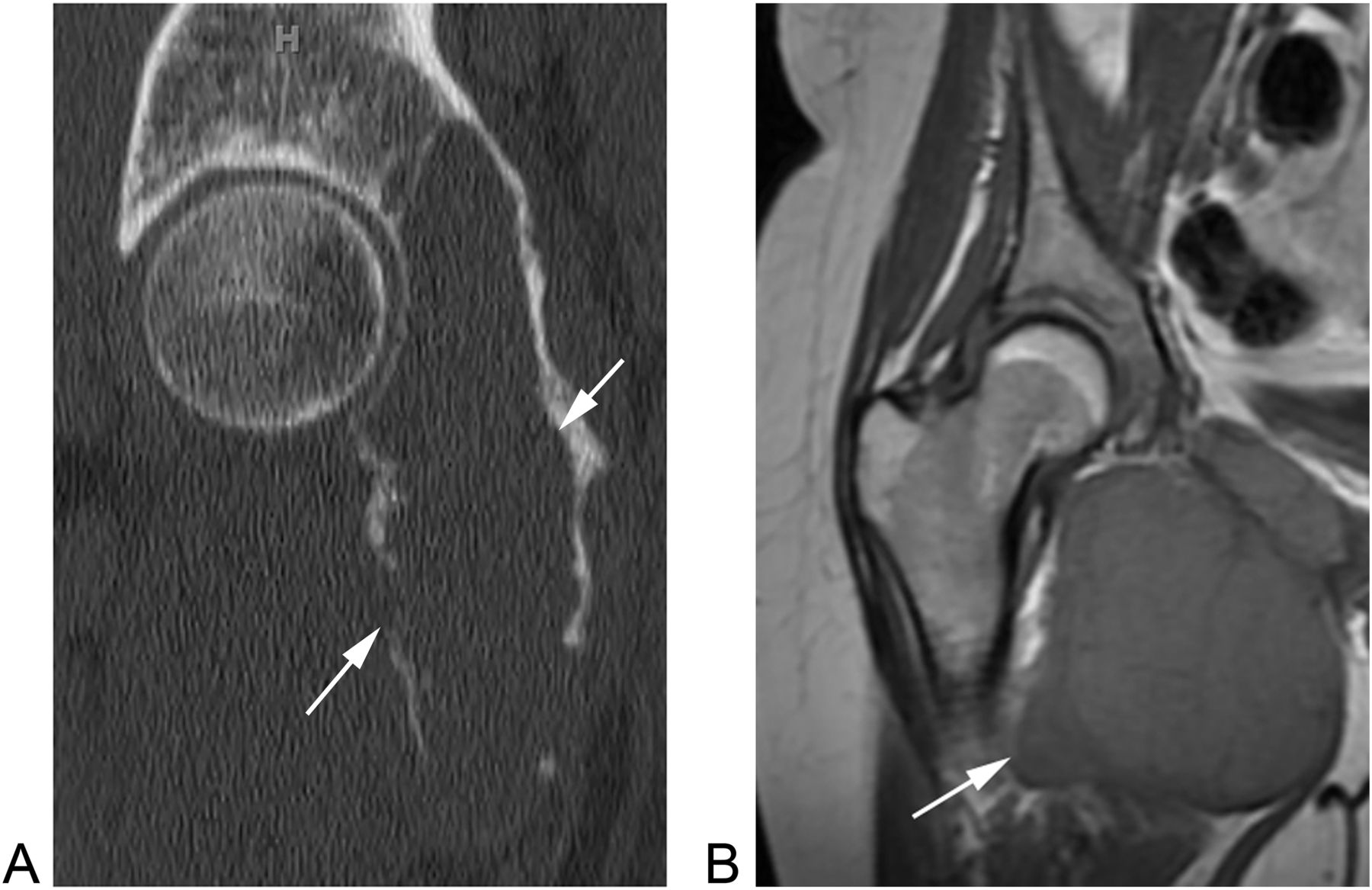




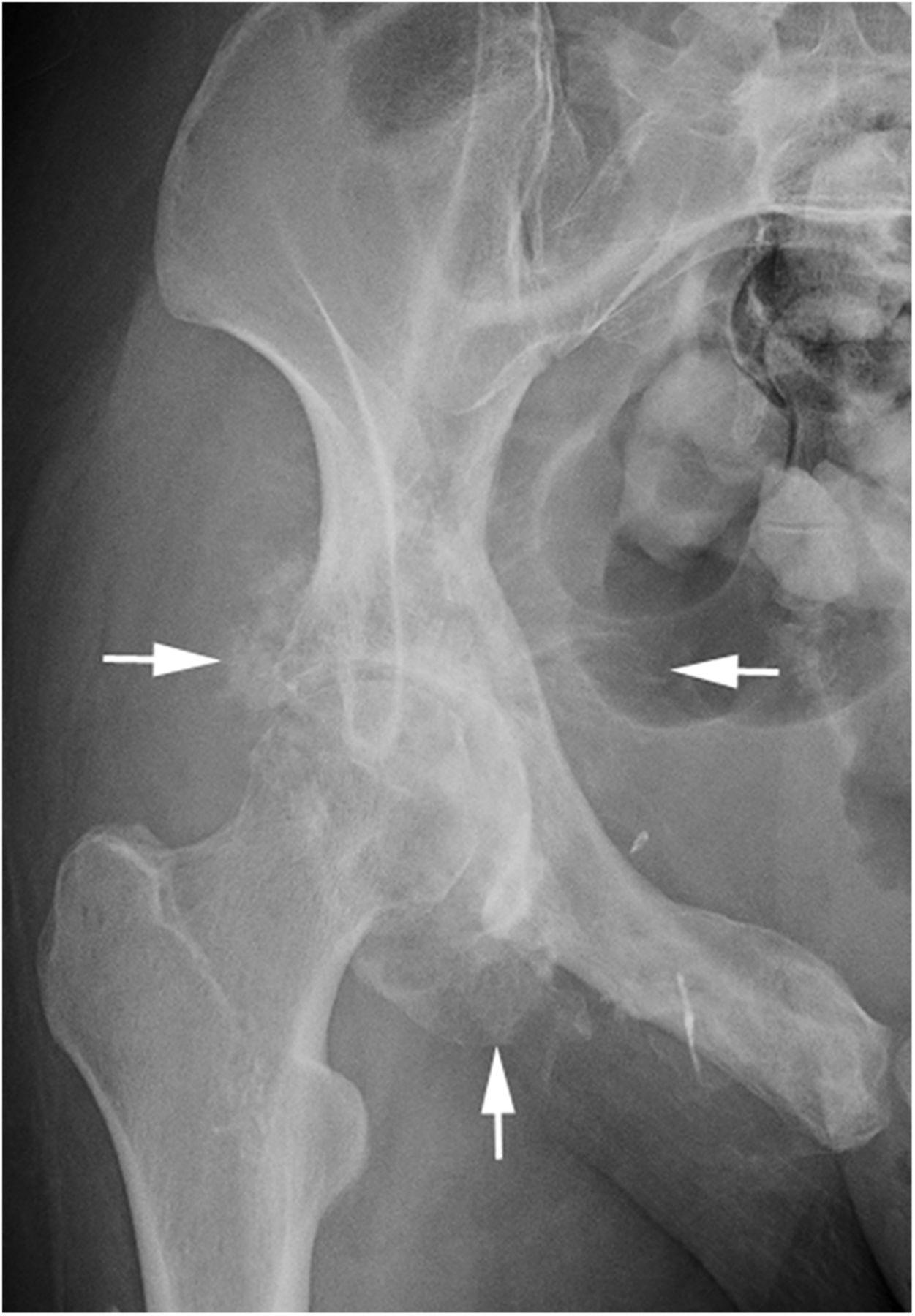
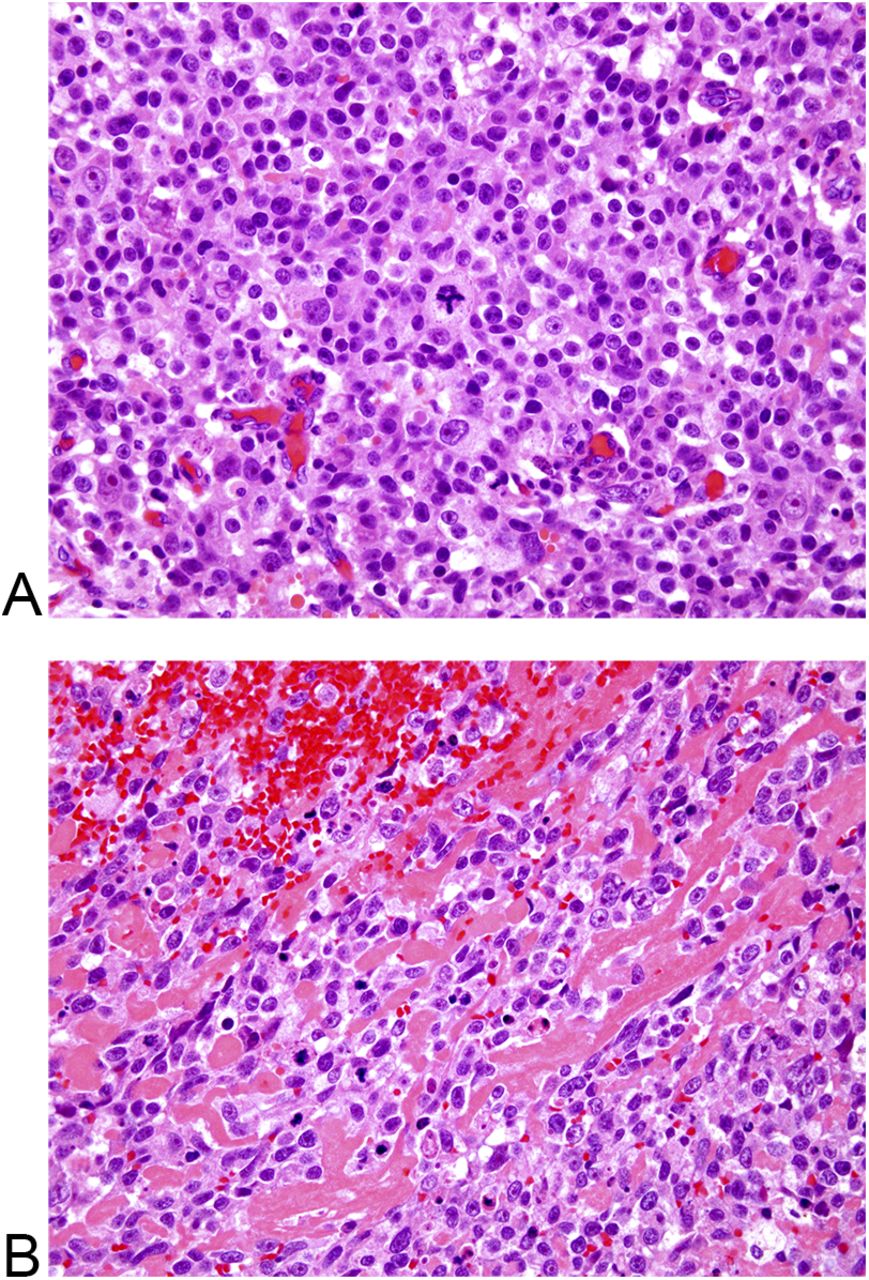
 Fig. 1
Fig. 1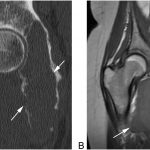 Fig. 2
Fig. 2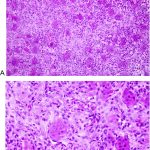 Fig. 3
Fig. 3 Fig. 4
Fig. 4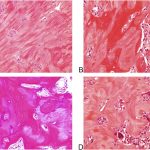 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7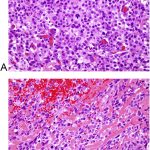 Fig. 8
Fig. 8