A 38-Year-Old Woman with Long-Term Shoulder Pain
March 7, 2018
A 38-year-old woman presented to the orthopaedic team with a 3-year history of left shoulder pain, with no history of trauma. She had no other comorbidities. On physical examination, she had painful shoulder range of motion. Radiographs (Figs. 1 and 2) revealed an osteolytic expansile lesion in the spine of the left scapula, which was confirmed with computed tomography (CT) (Fig. 3) and magnetic resonance imaging (MRI) (Figs. 4 and 5). Technetium-99m scintigraphy showed no other bone lesions.
A core biopsy of the left scapular lesion was performed 1 month later; it showed a well-differentiated follicular neoplasm (Fig. 6-A). Immunohistochemical stains were positive for cytokeratin CAM 5.2 (Fig. 6-B), thyroglobulin (Fig. 6-C), and thyroid transcription factor-1 (TTF-1) (Fig. 6-D).
The head and neck team also evaluated the patient. Thyroid ultrasonography demonstrated a well-delimited hypoechoic nodule in the thyroid, and the serum thyroglobulin level was 177 ng/mL (normal, 1.5 to 35 ng/mL). Abdominal and pelvic CT was done for staging and surveillance, and an adnexal mass was found in the right ovary.
Three months after the initial evaluation by the orthopaedic team, the patient underwent a total thyroidectomy and a salpingo-oophorectomy on the right side. The thyroid gland weighed 17.5 g, showed no lesions on macroscopic analysis, and was submitted en bloc for histopathologic examination, which revealed only a colloid goiter (Fig. 7-A) and lymphocytic thyroiditis (Fig. 7-B).
The right ovary had an increased size; it weighed 75.5 g and measured 5.2 cm in the major axis. Macroscopically, the whole ovary was occupied by a brownish and gelatinous lesion, without rupture of the capsule. The histology of the ovarian tissue is shown in Fig. 7-C.
The thyroid tissue was found to contain only a colloid goiter, so even though tissue in the scapula and ovary seemed to contain thyroid follicles, they could not represent metastatic follicular carcinoma from the thyroid. The ovary contained histologically mature thyroid tissue, diagnostic of a monodermal teratoma (struma ovarii). Therefore, the scapular lesion represented metastatic struma ovarii from the ovary.
After surgery, the patient began thyroid replacement therapy. The serum thyroglobulin level was 356.21 ng/mL. She underwent radioactive iodine (RAI) therapy; however, the serum thyroglobulin level remained elevated (2,662.98 ng/mL). Positron emission tomography (PET)-CT showed intense activity in the left scapula, with standardized uptake values between 2.7 and 3.6.
A tridimensional partial scapulectomy was performed 9 months after the first 2 surgeries (Fig. 8); it was followed by a new dose of RAI therapy. The specimen showed an ill-defined whitish lesion measuring 0.7 × 0.3 cm. The microscopic findings were of a well-differentiated follicular carcinoma of thyroid-tissue origin invading bone, with focal cortical rupture and adjacent soft-tissue extension (Fig. 7-D). All margins were free of neoplasm.
Another PET-CT was obtained 6 months later, and there was no metabolic fluorodeoxyglucose activity. Nearly 1 year after the partial scapulectomy, the patient was well and asymptomatic, and had full range of motion of the shoulder. Follow-up radiographs showed no evidence of residual disease or recurrence. The patient remained on thyroid replacement therapy, and the serum thyroglobulin level was 1.23 ng/mL at this time.
Proceed to Discussion >>Reference: Comunello J, Eloi Pinto FF, Nakagawa SA, Tu Chung W, D’Almeida Costa F, Brilhante AD. Isolated scapular metastasis in a patient with malignant struma ovarii: a case report. JBJS Case Connect. 2017 Oct-Dec;7(4):e82.
Struma ovarii is a monodermal ovarian teratoma that is composed of >50% thyroid tissue. Only 20% of ovarian neoplasms are teratomas, and only 2% of ovarian teratomas are considered struma ovarii. They are usually benign neoplasms; malignant struma ovarii occur in <1% of these patients. Bone metastasis of struma ovarii is even rarer; to our knowledge, only a few cases have been described in the literature. Because of its rarity, the diagnosis is challenging, and the optimal treatment is unclear.
The clinical presentation of struma ovarii is variable. An asymptomatic ovarian mass is usually present (in 58% of patients) and may cause ascites and hydrothorax (Meigs syndrome). Laboratory evidence of hyperthyroidism also may be present. Acute abdominal pain occurs in 12% of patients. Bone pain as the first sign of disease is unusual.
If struma ovarii induces hyperthyroidism, it is not unusual to suspect a thyroid neoplasm, which explains why most patients initially are treated with a thyroidectomy. Abnormal levels of thyroglobulin as well as abdominal and pelvic CT showing an ovarian mass may lead to the diagnosis. The majority of cases, however, are diagnosed only after salpingo-oophorectomy or total hysterectomy.
Distant metastasis of struma ovarii occurs in <5% of cases. The most common sites are the pelvic and paraaortic lymph nodes (via the lymphatic system); the omentum, the peritoneal cavity, the mesentery, and the contralateral ovary (via direct spread); and the liver, the lungs, the bones, and the brain (via hematologic dissemination). Patients who present with distant metastatic disease undergo a biopsy of the metastatic site and pathologic examination to confirm the diagnosis.
Some authors suggest that pelvic surgery alone may be sufficient for the treatment of struma ovarii, whereas total thyroidectomy is reserved for patients with a distant metastasis and extraovarian spread. Many studies discuss iodine-131 radioablation after struma ovarii resection and after resection of metastases. In our case, the patient seemed to have a single skeletal metastasis and a high serum thyroglobulin level after the pelvic surgery and the total thyroidectomy had been performed. The optimal treatment of bone metastasis is controversial. Surgery was our treatment of choice, with the intention to decrease pain without there being any loss of function.
A few cases of struma ovarii with thoracic and lumbar spine metastasis have been described in the literature. Surgery followed by RAI therapy was performed in 1 patient with paraparesis, with good results and remission of the symptoms. Pelvic bone metastases also have been described. Nuclear medicine imaging using radioiodine can be performed to demonstrate metastatic carcinoma. Extrathyroidal iodine uptake in pelvic bone after total thyroidectomy allowed the diagnosis of bone metastasis. In 1 case, RAI therapy resolved the bone lesion. The second case was an extensive left hip metastasis that was successfully treated with surgery.
The metastatic potential of struma ovarii is difficult to predict. Even some histologically benign struma ovarii are associated with recurrence and extraovarian metastasis. Some authors analyzed the biologic behavior of malignant struma ovarii; the factors predictive of a potentially more aggressive clinical course are large tumor size (>10 cm), >80% stromal tissue, extensive papillary carcinoma histology, >5 mitoses per 10 high-power fields, and marked cytologic atypia. Our case showed none of these criteria.
Some patients had early distant metastasis, and others did not have metastasis until 10 years after the struma ovarii resection. Therefore, long-term follow-up is imperative. The serum thyroglobulin measurement appears to be useful not only to identify local recurrence, but also for early metastatic detection. In most cases, elevated levels were found only postoperatively, although it is possible that the levels were elevated preoperatively as well, mainly in patients affected with hyperthyroidism.
The case described herein has several strengths. Wide resection of the metastatic site associated with salpingo-oophorectomy seems to be the ideal treatment for metastatic struma ovarii. We also attempted to confirm the value of the thyroglobulin measurements preoperatively and postoperatively. However, the results may be limited by the short follow-up because we know that the disease can recur at 10 years following the initial treatment. Another limitation is the lack of consensus in the literature about the treatment of choice for the metastatic site, mainly when the metastasis occurs in the bone, which makes it difficult for a physician to choose between surgery and RAI therapy.
Reference: Comunello J, Eloi Pinto FF, Nakagawa SA, Tu Chung W, D’Almeida Costa F, Brilhante AD. Isolated scapular metastasis in a patient with malignant struma ovarii: a case report. JBJS Case Connect. 2017 Oct-Dec;7(4):e82.
What is the diagnosis?
Metastatic follicular carcinoma of the thyroid gland to the ovary and scapula
Metastatic follicular carcinoma of the thyroid gland to the scapula, and a monodermal teratoma (struma ovarii) of the ovary
Metastatic struma ovarii to the scapula and thyroid gland
Colloid goiter of the thyroid gland, and struma ovarii of the ovary with metastasis to the scapula
Metastatic papillary carcinoma of the thyroid to both the ovary and scapula

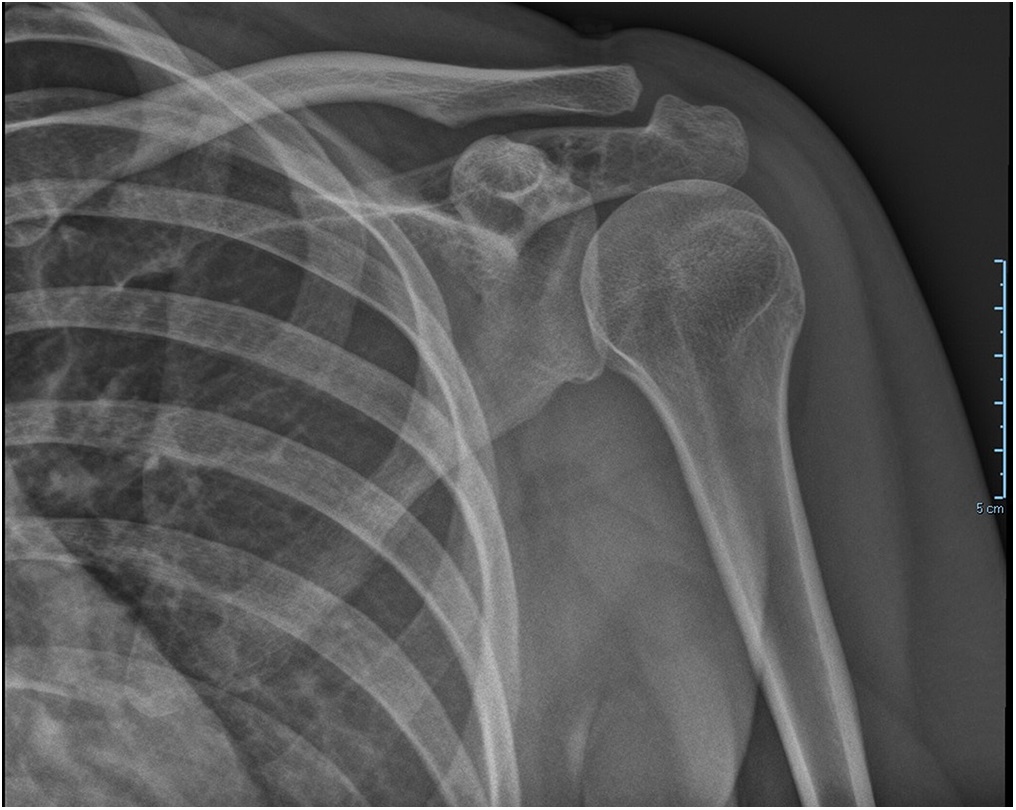

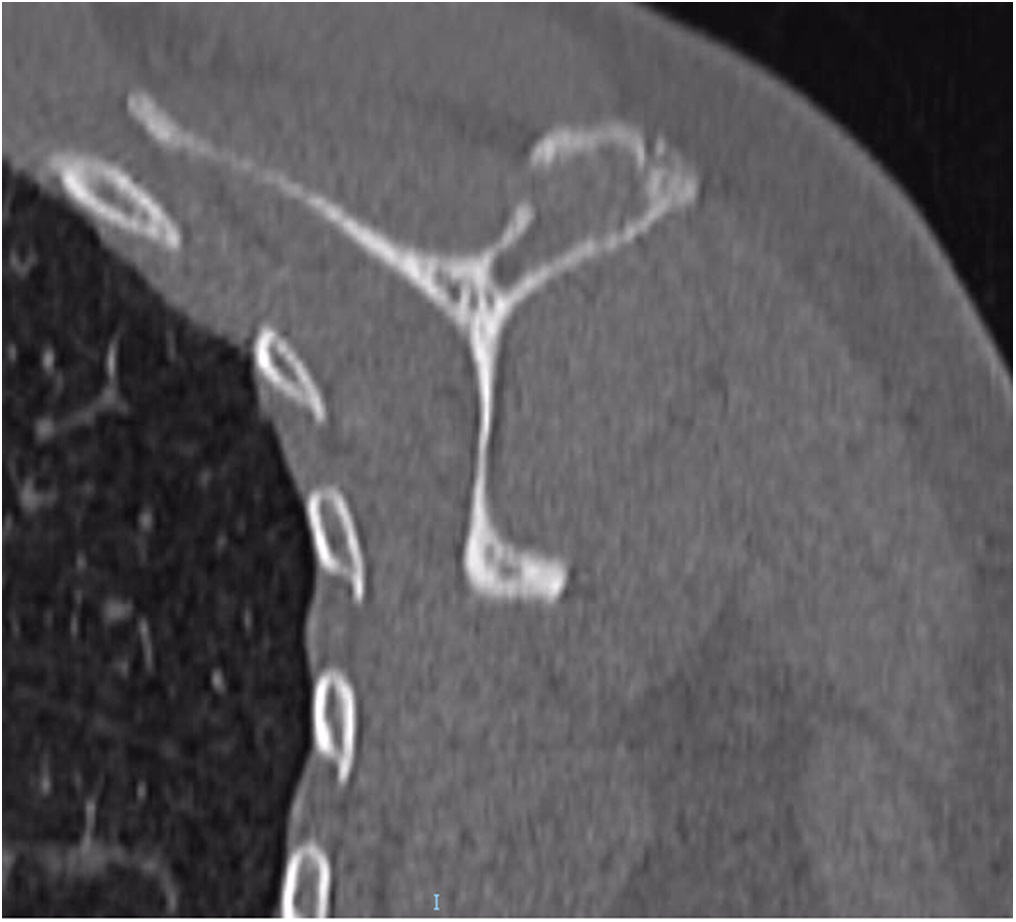
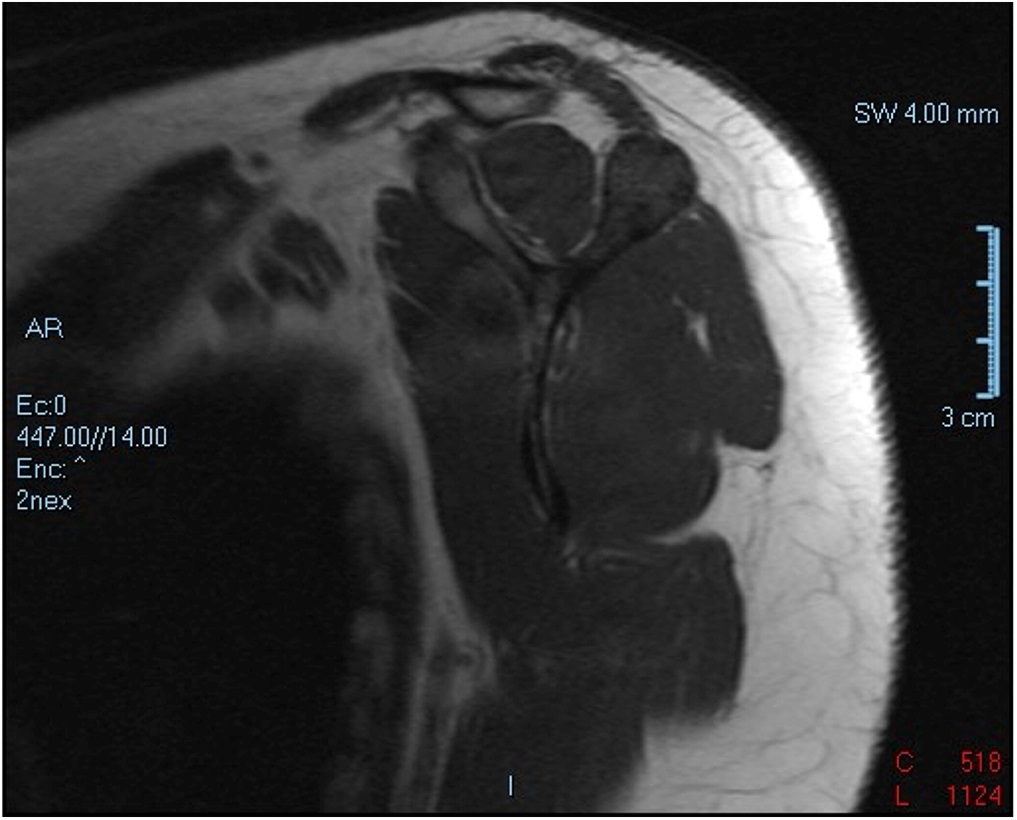
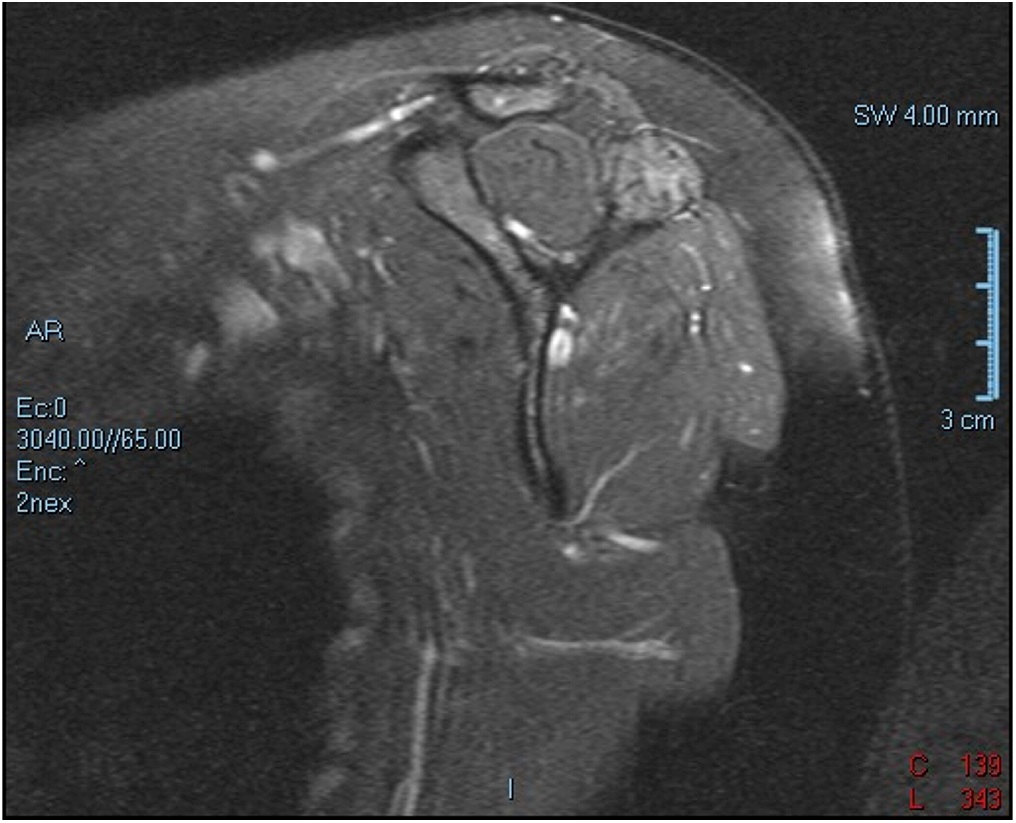
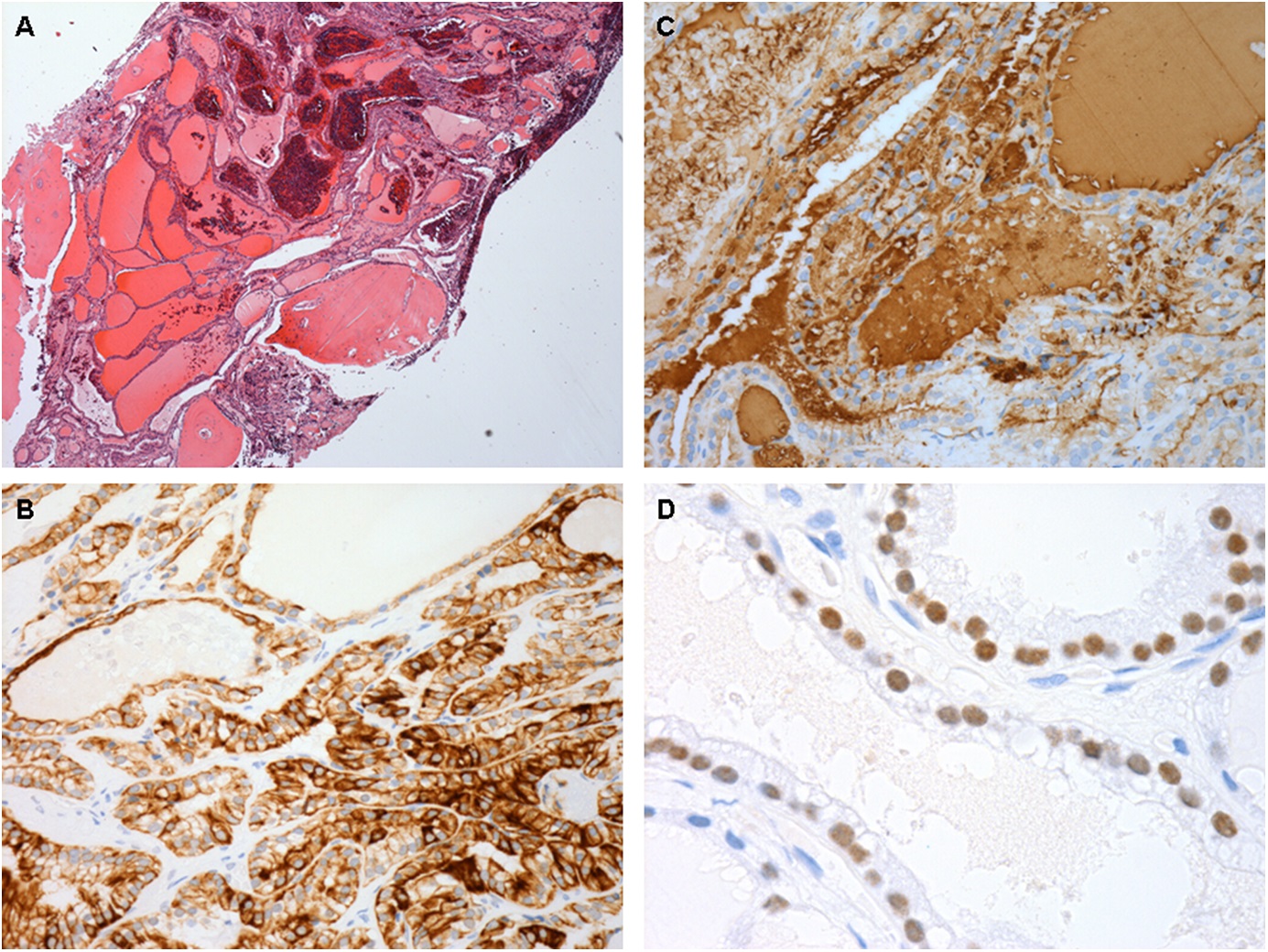
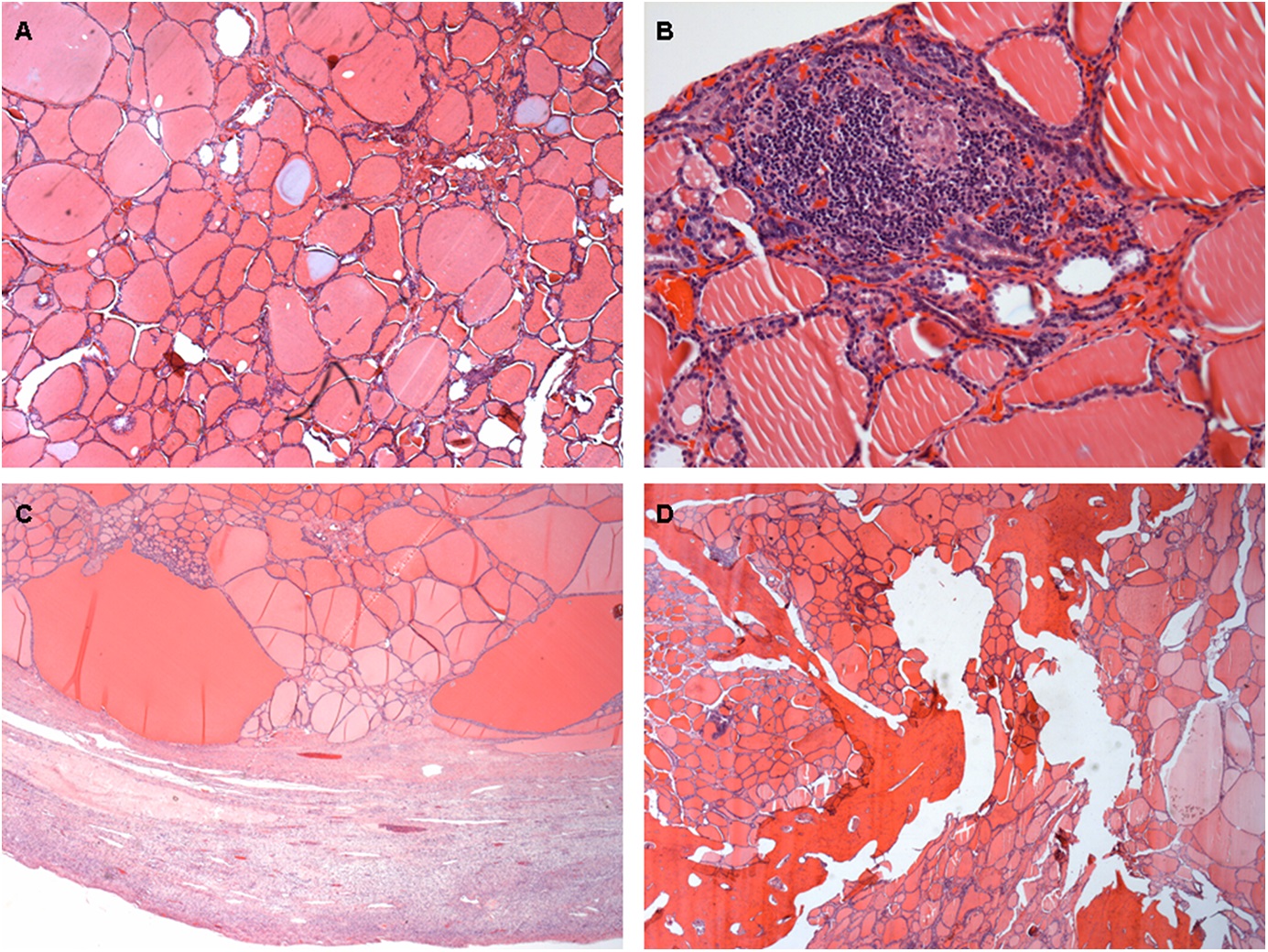
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6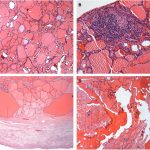 Fig. 7
Fig. 7 Fig. 8
Fig. 8