This patient first presented in 1972 at age 14 because of a mass in the anterior aspect of the right knee. Evaluation showed a cystic mass lateral to the patellar tendon; aspiration yielded gelatinous fluid with no evidence of infection, apparently interpreted as a ganglion cyst. The patellar tendon was substantially widened, measuring 4 cm at its attachment site to the tibial tubercle. At the level of the joint, the tendon was found near the edge of the lateral femoral condyle. Physical examination of the patient’s older brother at that time revealed full knee extension and active flexion to 135° bilaterally, while the younger brother had full extension and was able to flex the knees so that the heels reached the buttocks.
Over the next 40 years, both brothers visited 4 orthopaedic surgeons who performed several bilateral knee arthroscopies for meniscal pathology, synovitis, chondromalacia, and patellar tendon fraying. We were unable to determine the total number of surgeries because the records were not attainable and the patients were uncertain. However, it was evident that the younger brother had undergone an open procedure at the age of 13 years, which had required staple fixation of the left tibial tubercle. Furthermore, the older brother had developed diabetes mellitus and hypertension, while the younger brother had undergone coronary artery bypass graft surgery after sustaining a myocardial infarction.
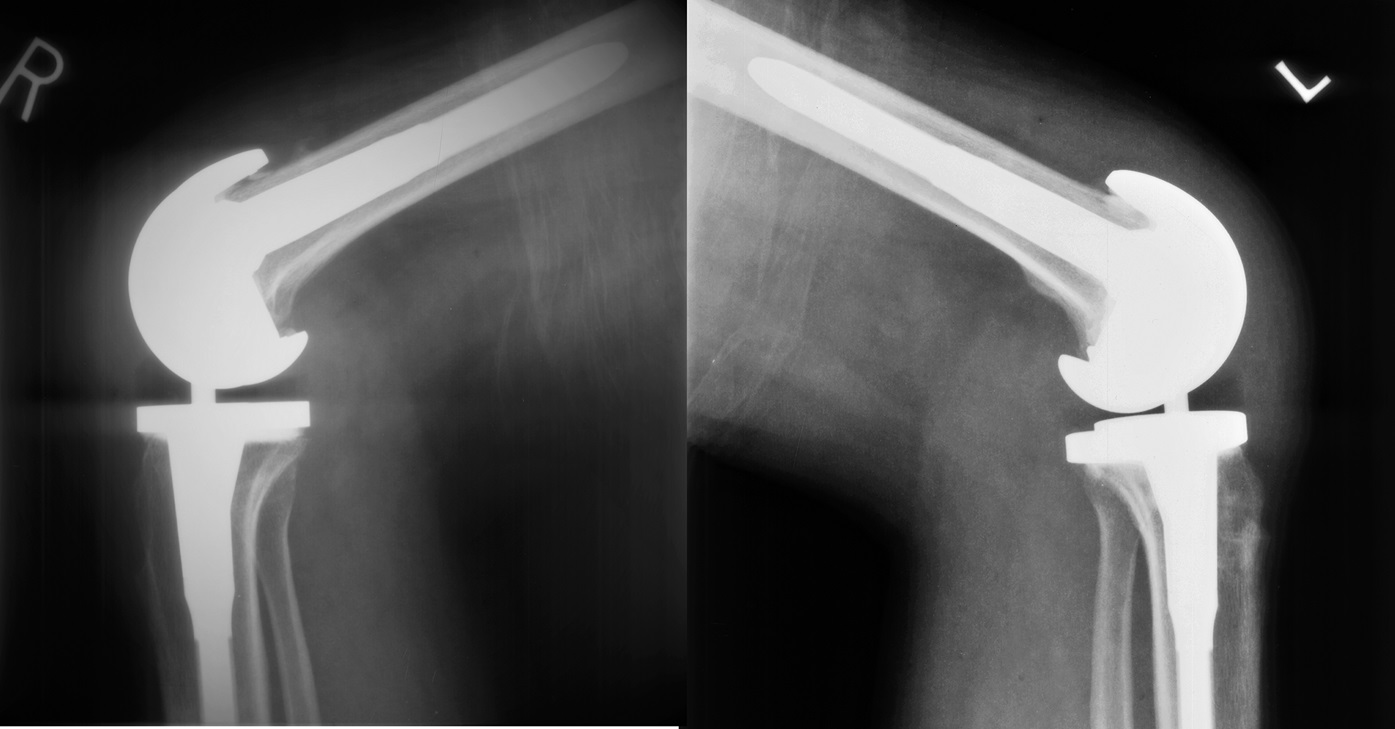
After several procedures, both individuals were found to have severe degenerative osteoarthritis, which may have been directly related to the number of prior procedures that had been performed and/or secondary to the possibility of altered knee biomechanics. In 2010, the younger brother was the first to present for joint replacement at the age of 45 years. On initial presentation, he noted right-sided knee pain and difficulty when walking for long distances, and especially when ascending and descending stairs. He had performed physical therapy and received numerous injections of hyaluronic acid without any relief. On examination, he had range of motion from 0° to 135° bilaterally, right-sided medial joint line pain, and bilateral grade-2 to 3 varus and valgus instability at both 0° and 30°. The Lachman examination, the anterior and posterior drawer tests, the pivot-shift test, and the posterolateral rotatory stress test at 30° and 90° were all negative. Radiographs are shown in Figures 1 and 2.
These brothers, originally described in 1973, represent examples of familial patella absentia syndrome.
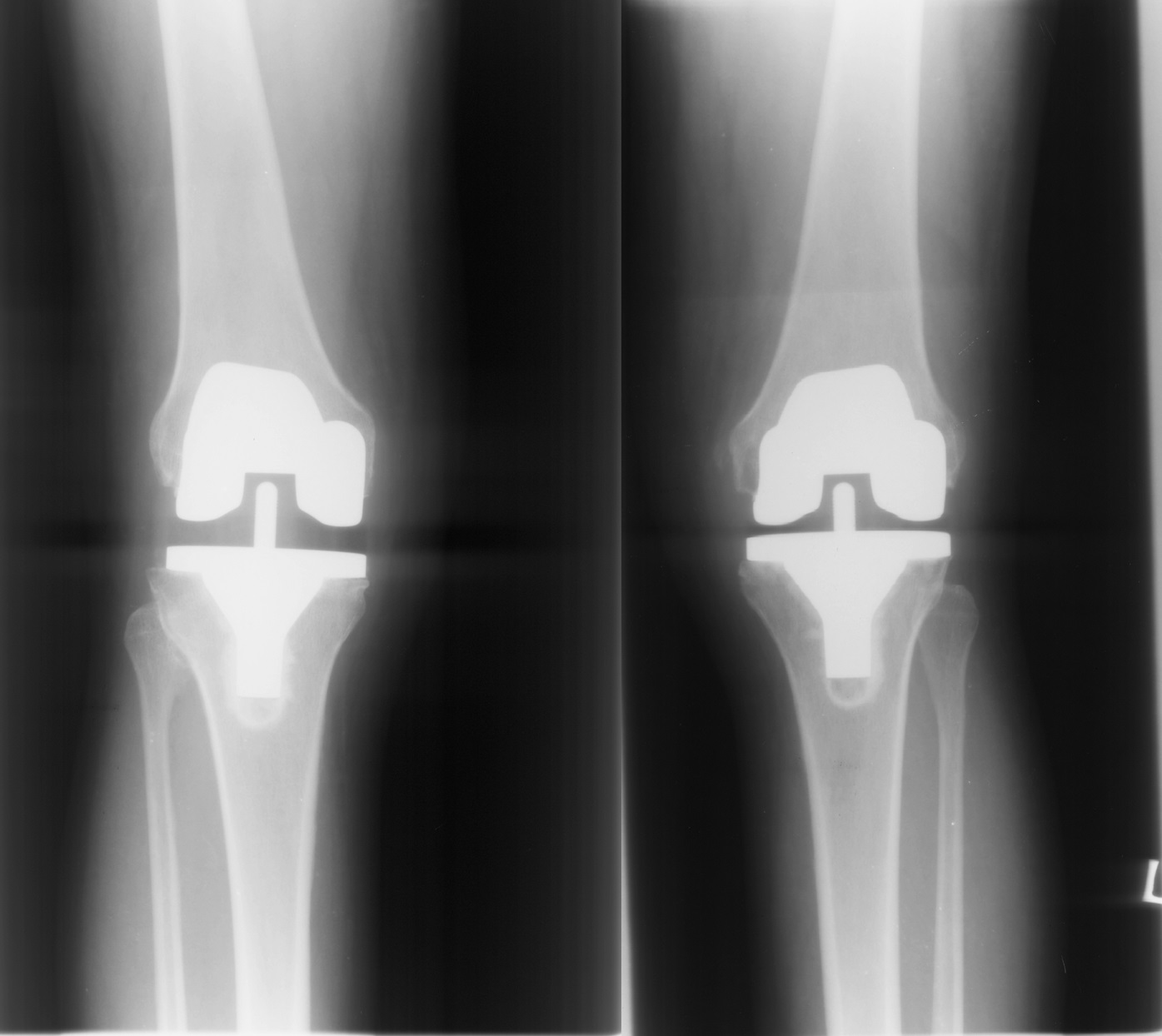
The younger brother underwent a right total knee arthroplasty with use of a semiconstrained prosthesis because of the varus and valgus laxity. Of note, at the time of the arthroplasty, striations that were visible in the quadriceps-patellar junction were sutured at the end of the surgery to allow for smooth gliding over the prosthesis (Figs. 3 and 4).
Pain in the younger brother’s left knee worsened, and he was unable to perform certain activities of daily living. A total knee arthroplasty was performed on the left knee 7 months after the arthroplasty on the right, with use of the same prosthesis system. The tibial tubercle staple was removed without any complications.
The younger brother tolerated both procedures well and had no immediate postoperative complications. He was evaluated at 2 and 4 months after the right knee arthroplasty, and range of motion remained limited from 0° to 100°. He continued physical therapy and returned for follow-up in July 2011; at that time, there was improved range of motion from 0° to 125° in both knees (Figs. 3 and 4).
Following his younger brother, the older brother presented for evaluation of knee pain. In June 2013, he noted worsening pain in the left knee, which occurred at rest as well as with stair-climbing. Examination of both knees revealed range of motion measurements from 5° to 115°, with a minor extension lag present in the left knee, bilateral grade-1 to 2 varus and valgus instability at both 0° and 30° (evidently more stability than his brother). The Lachman examination, the anterior and posterior drawer tests, the pivot-shift test, and the posterolateral rotatory stress test at 30° and 90° were all negative. Well-healed scars, including healed arthrotomy incisions (possibly from removal of a ganglion cyst) over the medial aspect of the right knee and arthroscopy scars, were present. Additional radiographic findings revealed bilateral joint space narrowing, as well as lateral translation of the tibia on the femur. In August 2013, the patient elected to proceed with a total knee arthroplasty for the left knee with use of a standard posterior stabilized prosthesis. Intraoperatively, the quadriceps mechanism was tracking well, and the rest of the ligaments appeared well-balanced. Postoperatively, the range of motion was from 0° to 125°, and the pain had improved (Fig. 5).
Shortly thereafter, the patient returned with symptoms in the right knee; in October 2013, he underwent a total knee arthroplasty with the same prosthesis system that had been used in the contralateral leg. Postoperatively, the range of motion was from 0° to 125°; no lag in motion was noted in flexion or extension (Fig. 5).
Proceed to Discussion >>Reference: Khaimov M, Fakhoury J, Karim F, Bitterman A, Alpert S. Total knee arthroplasty in patients with familial patellar absentia syndrome: a 40-year update: a case report. JBJS Case Connect. 2018 Oct-Dec;8(4):e100.
Isolated absence of the patella is a very rare phenomenon, and most of the documented cases have a syndromic presentation. With regard to our patients, the rarity is further compounded by the fact that the disorder appeared in only 2 of 5 non-twin children in a single family. Additionally, it is rare for an absent patella to be the sole cause of disability. These 2 brothers, who do not have any additional pathology, may fall under the diagnosis of patella aplasia-hypoplasia (PTLAH).
These 2 patients are similar to those described in prior case reports. They had complete congenital absence of the patella with comparable clinical characteristics, including prominent femoral condyles and a widened extensor mechanism. These adaptations provide the extensor mechanism with increased relative stability and a stronger fulcrum for extension. Degenerative changes and instability requiring total knee arthroplasty appeared in our patients at an earlier age than is average for severe osteoarthritis.
According to Jerome et al., for many with this abnormality, the lack of a patella may be deemed unimportant and necessitates no specific treatment. In 1944, Kiil-Nielsen believed that if the only defect in a patient was absent patellae, the function of the knee was normal. About half of the cases he presented were observed in children, many in whom the patellae developed later in patients who received nonoperative management, including massage and bracing. He also stated that if the quadriceps are functional, the absence of the patella should not cause an inconvenience.
Patients with absent patellae also may have additional knee pathology that requires operative intervention, as with these 2 brothers early on. These pathologies include, but are not limited to, severe flexion contractures in addition to extensor mechanism maltracking. Depending on a patient’s clinical findings, surgical procedures can include hamstring lengthening, proximal and distal realignment procedures, and lateral retinacular release. Guidera et al. noted that approximately 50% of children with nail-patella syndrome underwent knee surgery to treat instability. The main goal of these operations is to restore adequate alignment and maintain knee functionality. It is important to implement aggressive physical therapy after any such procedure to ensure that contractures do not return.
There is limited published information regarding total knee arthroplasty in patients without patellae. Most reports generally have focused on patients with hypoplastic patellae or on those who have undergone patellectomy as opposed to those with congenital absence of the patellae. In studies of patients receiving total knee arthroplasty for degenerative joint disease, patella absentia is not a limiting factor.
For most individuals, congenital absence of the patella may pose no problem. Based on our literature search, the etiology and clinical importance of this anatomic abnormality require additional long-term studies. In some patients, early treatment options may not be successful, and biomechanical ramifications may involve alteration of how the joint functions, resulting in early-onset osteoarthritis. If nonoperative measures are unsuccessful, total knee arthroplasty is a viable option that can provide pain relief and restoration of adequate joint biomechanics.
Reference: Khaimov M, Fakhoury J, Karim F, Bitterman A, Alpert S. Total knee arthroplasty in patients with familial patellar absentia syndrome: a 40-year update: a case report. JBJS Case Connect. 2018 Oct-Dec;8(4):e100.
What is the diagnosis?
Gorham disease (massive osteolysis, disappearing bone disease)
Reiter syndrome
Chronic osteomyelitis of the patella
Familial patella absentia syndrome
Psoriatic arthritis


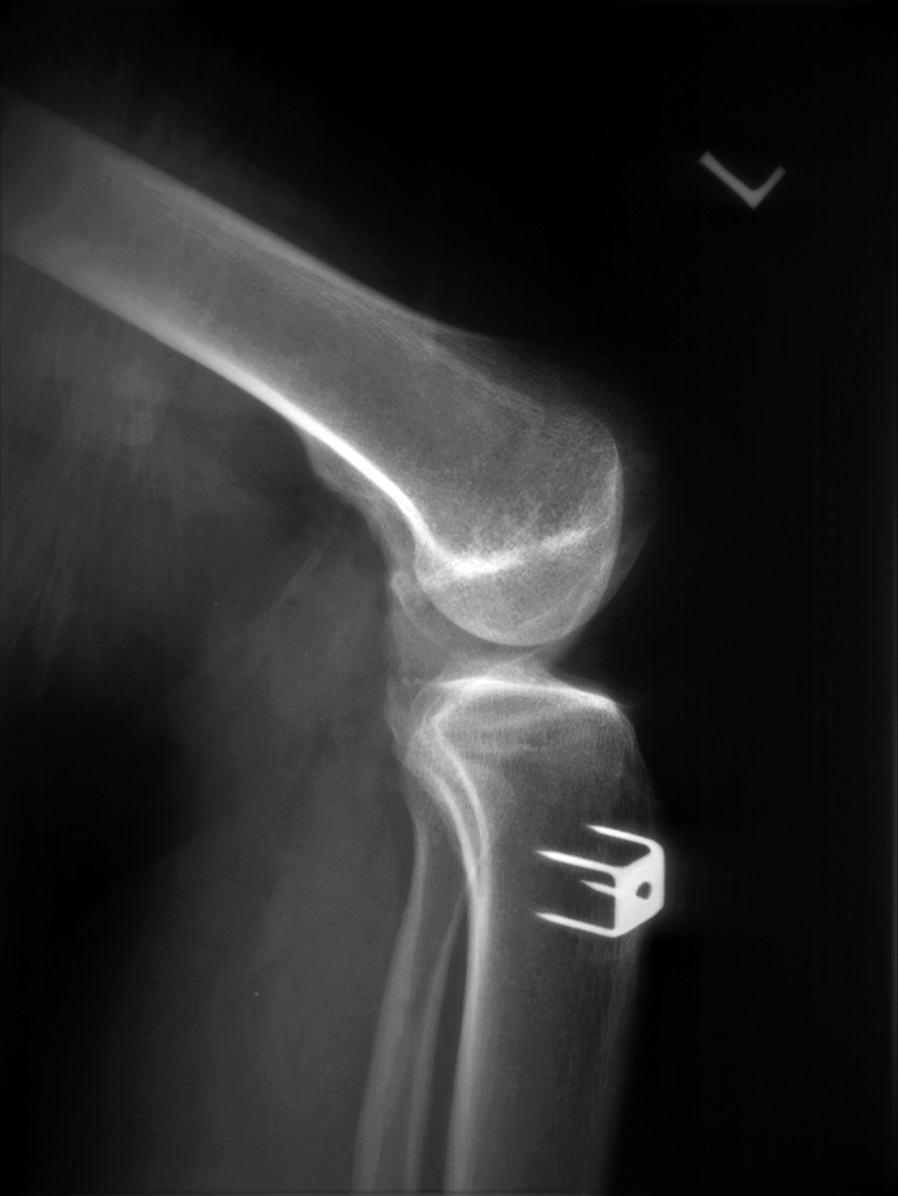
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5