A 48-Year-Old Woman with Pain in the Back and Thigh
April 17, 2019
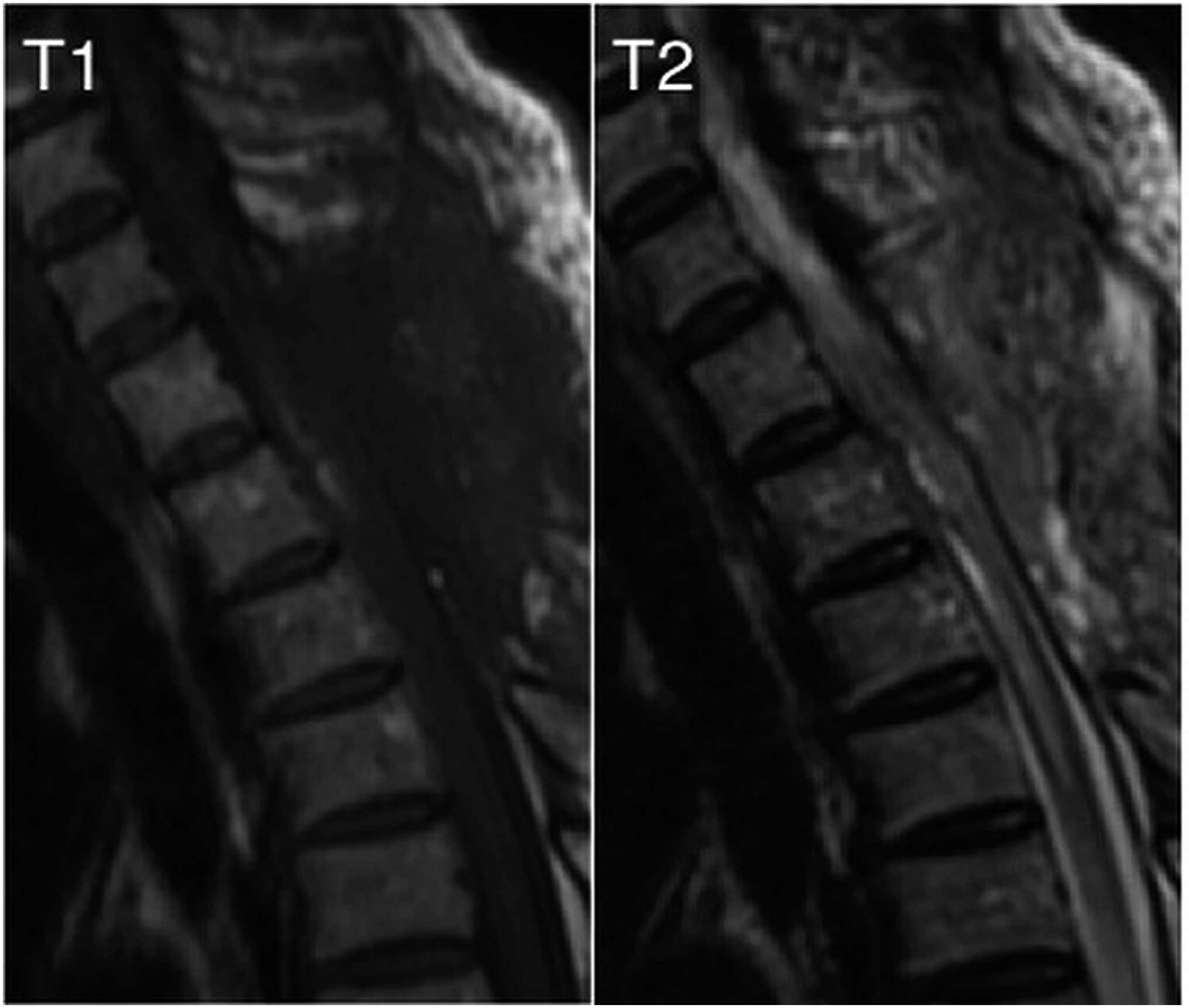
A 48-year-old woman, with no noteworthy medical history, presented to an outpatient clinic in March 2012 with back pain and pain around the lateral aspect of the left thigh. She first had noticed the back pain in December 2011; the thigh pain had started 1 week prior to the visit. Magnetic resonance imaging (MRI) revealed an intramedullary lesion at the level of the second thoracic (T2) vertebra, 8 mm in size, with heterogeneous hyperintense and hypointense regions on T1 and T2-weighted imaging and an area of hypointense signal surrounding the lesion on T2-weighted imaging (Fig. 1-A). There was no contrast enhancement (Fig. 1-B). Computed tomography (CT) and MRI with fat suppression were not performed. The patient was admitted for surgical resection.
The neurological evaluation prior to admission demonstrated a slight hyperreflexia of the lower limb and a mild sensory deficit on the lateral aspect of the left thigh. There was no motor weakness of the lower extremities or bladder/bowel dysfunction.
A midline spinous process-splitting approach was employed to expose the dura mater. With use of a microscope, the dura mater and arachnoid membrane were split, and the lesion was exposed via the posterior median sulcus. It was 8 mm in size (Fig. 2-A). We totally resected the lesion (Fig. 2-B).
The histology of the resected lesion is shown in Figure 3.
The patient was diagnosed with a lipoma variant (osteolipoma).
Histology revealed the lesion to be largely composed of mature lobulated adipose tissue (S100-positive) surrounded by glial scar tissue (S100 and glial fibrillary acidic protein [GFAP]-positive) with ectopic bone that contained marrow cells within the adipose tissue (Figs. 3-A, 3-B, and 3-C). The histological diagnosis was an intramedullary osteolipoma without evidence of malignancy.
At 2 weeks postoperatively, the patient was able to walk unaided, and she was discharged 6 weeks postoperatively. At the 3-year follow-up, she displayed mild dysesthesia of the lower limbs, but no recurrence of the osteolipoma was observed on MRI (Fig. 4).
Proceed to Discussion >>Reference: Kojima K, Iwanami A, Mikami S, Ishii K, Matsumoto M, Nakamura M. An intramedullary osteolipoma of the upper thoracic spinal cord: a case report. JBJS Case Connect. 2016;6(3):e80
The histogenesis of osteolipoma is still not understood, and various theories, including metaplastic response of fibroblasts to osteogenic factors, microtrauma, mechanical stress, and differentiation by mesenchymomas, have been suggested. Chromosomal abnormalities have also been reported, with almost 75% of lipomas displaying a form of aberration. Two-thirds of lipomas are thought to involve chromosome location 12q13-15; the most common rearrangement is translocation t(3;12)(q27-28;q13-q15).
Variants of lipomas, which generally lack the homogeneous fat signal that is observed on MRI of standard lipomas, can provide a more heterogeneous picture, which makes diagnosis difficult. Therefore, CT and MRI can both play an important role in diagnosing osteolipomas. CT will reveal a hypodense area of adipose tissue surrounding a hyperdense region of osseous tissue. MRI will reveal a heterogeneous picture on both T1 and T2-weighted imaging, and fat suppression will aid in identifying adipose tissue within the tumor. MRI with fat suppression could have helped differentiate a hemangiomatous tumor from a lipoma in our patient. Definitive diagnosis, however, requires a histological examination.
Osteolipomas behave in the same way as standard lipomas, and, to the best of our knowledge, no postoperative recurrences have been reported in the literature. Clinical symptoms of an intramedullary lipoma depend on the mass effect, and surgery is recommended only in those with progressive neurological symptoms. Postoperative prognosis of intramedullary lipomas with regard to neurological function is generally poor, and the acceptable goal of surgery is decompression of the adjacent neural structures. In the case of an intramedullary osteolipoma within the spinal cord, we believe that the location and clinical picture determine the surgical indication.
In summary, an intramedullary osteolipoma without any extramedullary connections or coexisting spinal dysraphism is rarely encountered in clinical practice and, if unsuspected, its diagnosis is extremely difficult. MRI with fat suppression and CT would be useful in diagnosing this type of tumor, but definitive diagnosis requires histological examination. Definitive treatment is complete surgical resection, but it is not indicated in all patients.
Reference: Kojima K, Iwanami A, Mikami S, Ishii K, Matsumoto M, Nakamura M. An intramedullary osteolipoma of the upper thoracic spinal cord: a case report. JBJS Case Connect. 2016;6(3):e80
What is the diagnosis?
Cavernous hemangioma
Lipoma variant (osteolipoma)
Malignant triton tumor (malignant peripheral nerve sheath tumor with rhabdomyoblastic differentiation)
Meningioma
Benign schwannoma with heterologous elements

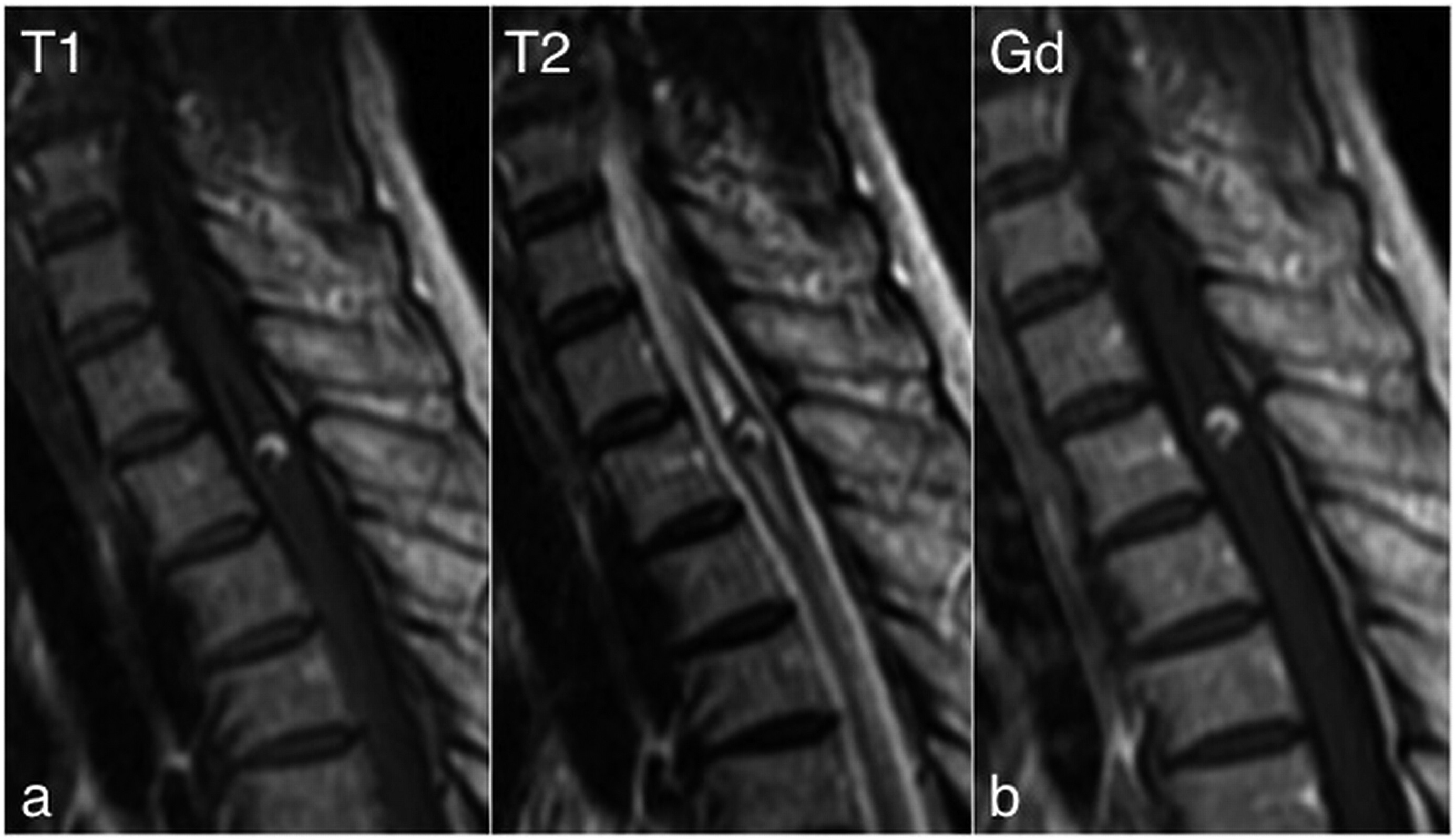
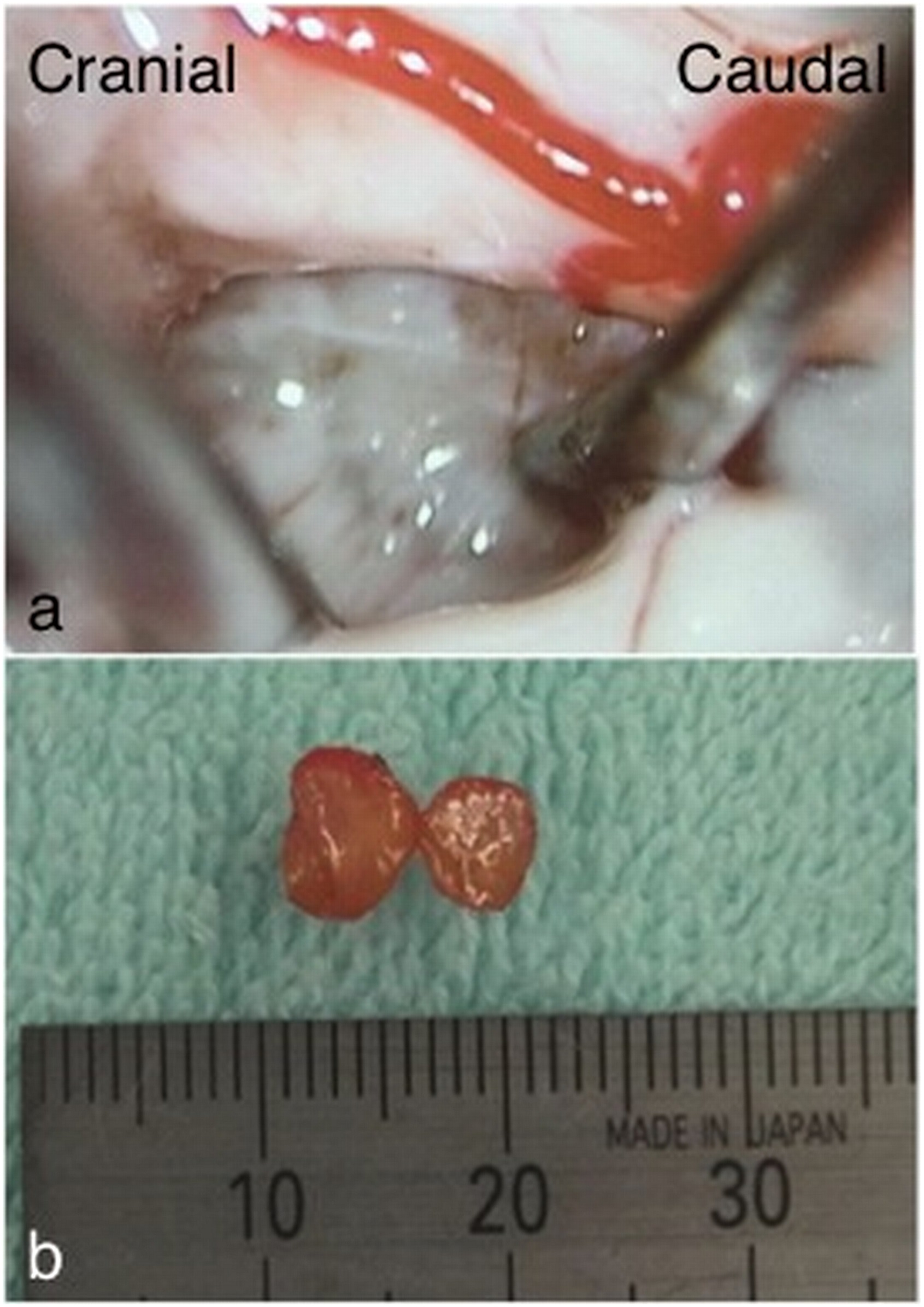
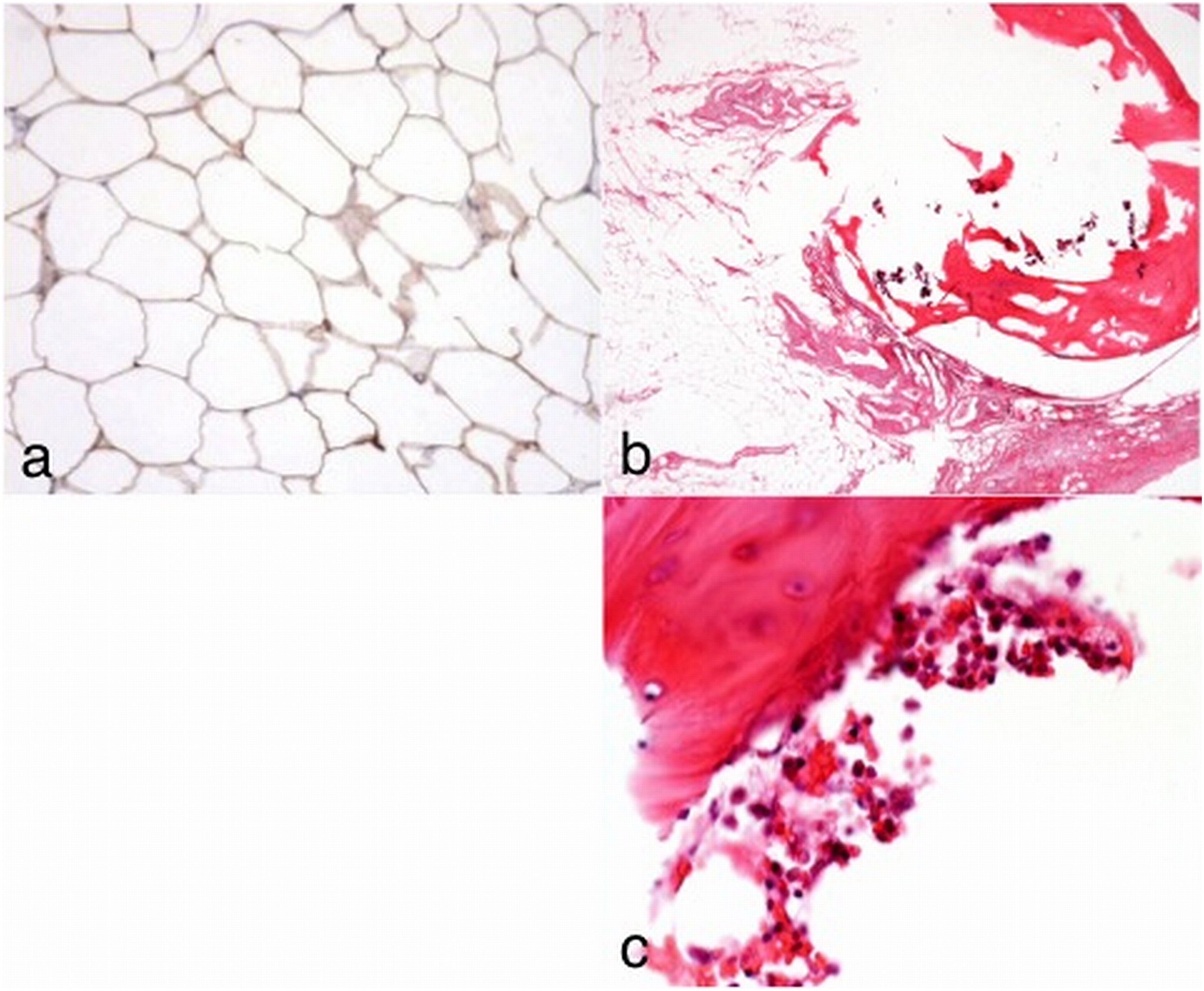
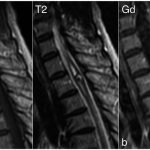 Fig. 1
Fig. 1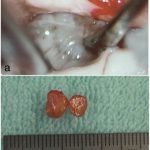 Fig. 2
Fig. 2 Fig. 3
Fig. 3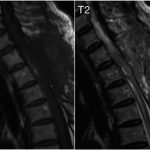 Fig. 4
Fig. 4