A 78-year-old man with multiple cardiovascular comorbidities presented to a musculoskeletal oncology clinic for acute right hip pain with a known right proximal femoral lesion. In 2006, he underwent lumbar and pelvic radiographs at our institution for chronic low back pain. The radiographs showed a radiolucent lesion in the right proximal part of the femur with a sclerotic rim and areas of internal septation and calcification (Figs. 1-A and 1-B). The lesion was believed to represent fibrous dysplasia or a liposclerosing myxofibrous tumor, and he was monitored with serial radiographs until he was lost to follow-up.
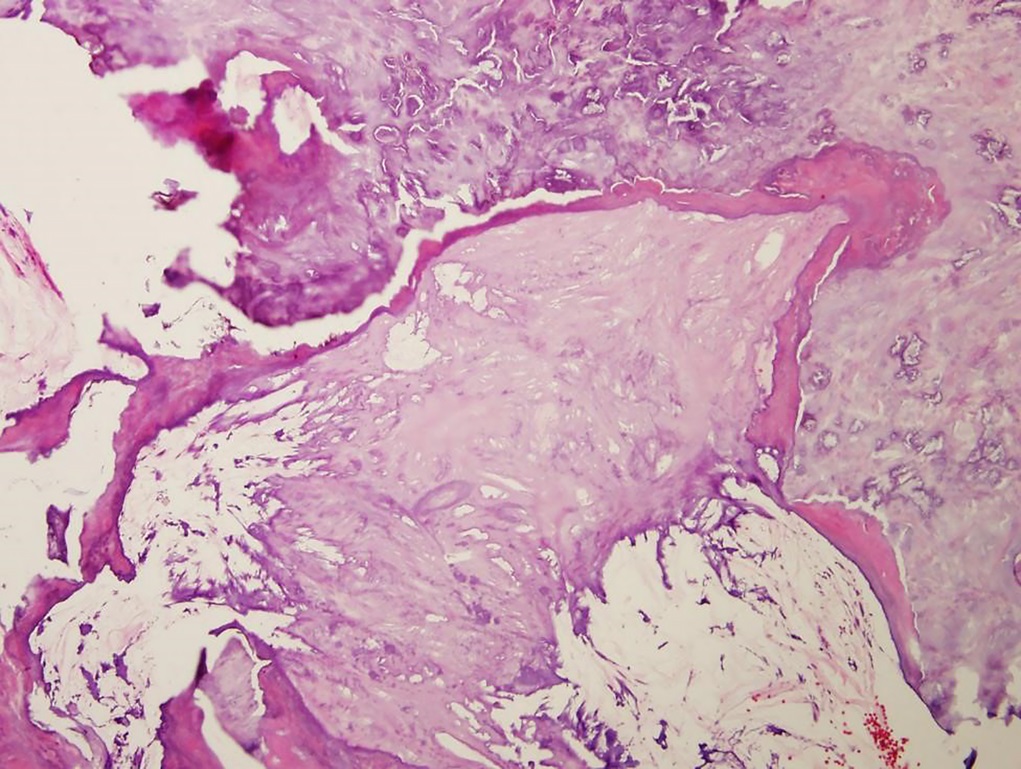
Eleven years later, the patient presented with a 2-month history of right proximal anterior thigh pain without inciting trauma. Radiographs of the right hip showed the proximal femoral lesion (Fig. 2-A). The lateral view (Fig. 2-B) showed loss of the posterior cortex at the level of the inferior lesser trochanter, representing a change in appearance since 11 years earlier. Magnetic resonance imaging (MRI) was obtained using a 0.2-T open magnet. (The MRI was of poor quality and could not be repeated because of insurance restrictions.) An intramedullary marrow-replacing lesion involving the proximal part of the femur and the heterogeneous signal was observed. The coronal T1-weighted image (Fig. 3-A) showed areas of high signal, isointense to subcutaneous fat. Fluid-sensitive sequences showed areas of high signal throughout the lesion, although fat-containing areas were hypointense, as expected. Linear areas of low signal consistent with mineralization were appreciated, corresponding to the radiographic appearance. On the sagittal short tau inversion recovery (STIR) image (Fig. 3-B), posterior perilesional soft-tissue extension was identified. A bone scan showed mild radiotracer uptake in the proximal part of the femur, with an area of moderately increased uptake along the medial proximal femoral cortex (Fig. 4). Histology from an open biopsy is shown in Figure 5.
The biopsy was interpreted as a high-grade pleomorphic sarcoma.
The planned procedure of placing an intramedullary nail was aborted, and the patient was staged. A computed tomographic (CT) scan of the chest showed no evidence of metastatic disease. The patient underwent proximal femoral resection and reconstruction with a megaprosthesis. Gross pathology demonstrated an invasion of the tumor into the medial cortex, which corresponded with preoperative imaging (Fig. 6). Histopathology demonstrated that most of the lesion was consistent with an old intraosseous lipoma. Cancellous bone in the intertrochanteric region had been replaced extensively by adipose tissue, much of which had undergone cystic change. Other portions had undergone fibrosis with myxomatous degeneration. There was extensive dystrophic calcification in the necrotic fat, no evidence of cartilage, and no osteonecrosis. In the medial portion of the distal segment of the lesion was a well-demarcated zone of high-grade pleomorphic sarcoma. This sarcoma was associated with endosteal erosion, which was absent on previous imaging. Stains for MDM2 were negative in the fatty portion of the lesion and in the sarcomatous area (Fig. 7).
The patient had an uneventful postoperative course and regained independent ambulatory function. Two years after the surgery, he developed pulmonary metastases. At the time of this writing, the patient was alive with disease, which was managed by systemic therapy.
Proceed to Discussion >>Reference: Kreulen RT, Mawn JG, Fayad LM, McCarthy EF, Morris CD. High-grade sarcoma arising in association with an intraosseous lipoma: a case report. JBJS Case Connect. 2020 Jul-Sep;10(3):e19.00577.
Intraosseous lipomas are rare tumors that are typically indolent in presentation. They can be diagnosed safely on radiographs and MRI, meaning that biopsy is not required for diagnosis and is not routinely obtained. Lesions can expand and become symptomatic without undergoing malignant transformation. In such instances, the lesion can be treated with curettage and bone graft. Although rare, malignant transformation associated with these lesions has been described. Such cases, as well as our case, highlight the importance of maintaining a high index of suspicion when the clinical presentation changes over time.
Mixed fibrous and osseous lesions were characterized by Ragsdale, who noted that these tumors appeared almost exclusively in the proximal part of the femur. Ragsdale described the lesions as “liposclerosing myxofibrous tumor” (LSMFT), which had been noted in case reports. LSMFTs were further characterized by Kransdorf et al., who presented a series of 33 patients. Lesions showed a mixed histology consistent with entities including lipoma, fibroxanthoma, myxoma, myxofibrosarcoma, fibrous dysplasia, cysts, fat necrosis, ischemic ossification, and cartilage. All patients in their series were adults (age range, 18 to 65 years), and lesions were discovered incidentally or secondary to pain. Radiographs showed well-defined lytic lesions with variable density, sclerotic border, and variable amounts of expansile remodeling. A mineralized matrix was also commonly seen, although in variable patterns. CT features mimicked those seen on radiography. No internal lipid density was noted. MRI revealed patterns that paralleled the histology. Lesions were well defined and had a peripheral low-signal rind. They were isointense to muscle on T1 and heterogenous on T2, with no internal lipid signal. Bone scan showed variable radiotracer uptake that was not correlated with malignant transformation. Kransdorf et al. proposed that the origin of this tumor was an intraosseous lipoma of bone with proliferative changes. Four patients (12%) in their series had evidence of associated malignancy. Kransdorf et al. concluded that there was a high prevalence of associated malignancy and that these lesions warranted close follow-up. However, considering LSMFT as a distinct diagnostic entity remains controversial. Datillo et al. examined 33 patients with LSMFT, 18 of whom had histology slides. The authors concluded that the disease represented degenerative changes in other well-characterized bone lesions, and they recommended against defining LSMFT as a distinct entity.
A classification system to describe intraosseous lipomas was proposed by Milgram and is based on the way in which intraosseous lipomas display different degrees of involution and necrosis. Stage-1 tumors consist of viable fat cells. Stage-2 tumors are transitional cases, partially composed fat cells but also containing fat necrosis and calcification. Stage-3 tumors contain necrotic fat that is often calcified, cysts, and reactive woven bone. This staging system describes the natural course for these lesions. Deviations from this course may be subtle. Sentinel events, such as the pain in our patient, can indicate that malignant transformation has occurred. In these cases, establishing a tissue diagnosis is important so that malignancy is not missed.
Previous examples of bone lipomas associated with surrounding malignancy were compiled in 1990 by Milgram. The 4 cases occurred in patients who were 19 to 60 years of age. All presented because of pain in the affected limb, which included the proximal part of the femur, the distal part of the femur, the proximal part of the tibia, and the proximal part of the fibula. Three patients were treated with amputation, and 1 patient was treated with a limb-sparing procedure. Of the 3 patients who returned for follow-up, 2 died from metastatic disease.
The surgical implications of this case are notable. Unfortunately, inadvertent nailing of sarcomas is not uncommon. Adams et al. and Spence et al. published series of sarcomas that had inappropriately undergone fixation, leading to widespread tumor contamination. Common themes in these series include incomplete preoperative imaging, improper biopsy and/or surgical technique, and insufficient collection of patient history. Fortunately, a frozen section specimen was sent at the time of our procedure, leading us to abort the planned prophylactic nailing procedure.
It is important to note that the neoplasm seen in this case and in others is likely not the transformation of the lipoma itself to a sarcoma. Rather, the pathogenesis is believed to be related to the reparative reaction that occurs around the lipoma as it undergoes necrosis and calcification. Sarcomatous transformation associated with other benign lesions of bone, such as bone infarcts and enchondromas, has been well described. It is believed that these processes likely occur by the same malignant transformation of the reactive zone as the tumor presented here.
We report a case of malignant transformation of an intraosseous lipoma of the proximal part of the femur. This case emphasizes the importance of maintaining a high level of suspicion for malignancy, even in the setting of a known benign bone lesion. Tissue diagnosis is crucial in understanding histologic changes that may explain the progression of symptoms and dictate the need for additional treatment.
Reference: Kreulen RT, Mawn JG, Fayad LM, McCarthy EF, Morris CD. High-grade sarcoma arising in association with an intraosseous lipoma: a case report. JBJS Case Connect. 2020 Jul-Sep;10(3):e19.00577.
What is the diagnosis?
Fibrous dysplasia
Intraosseous tenosynovial giant cell tumor (formerly called pigmented villonodular synovitis [PVNS])
De-differentiated giant cell tumor of bone
High-grade pleomorphic sarcoma
Telangiectatic osteosarcoma

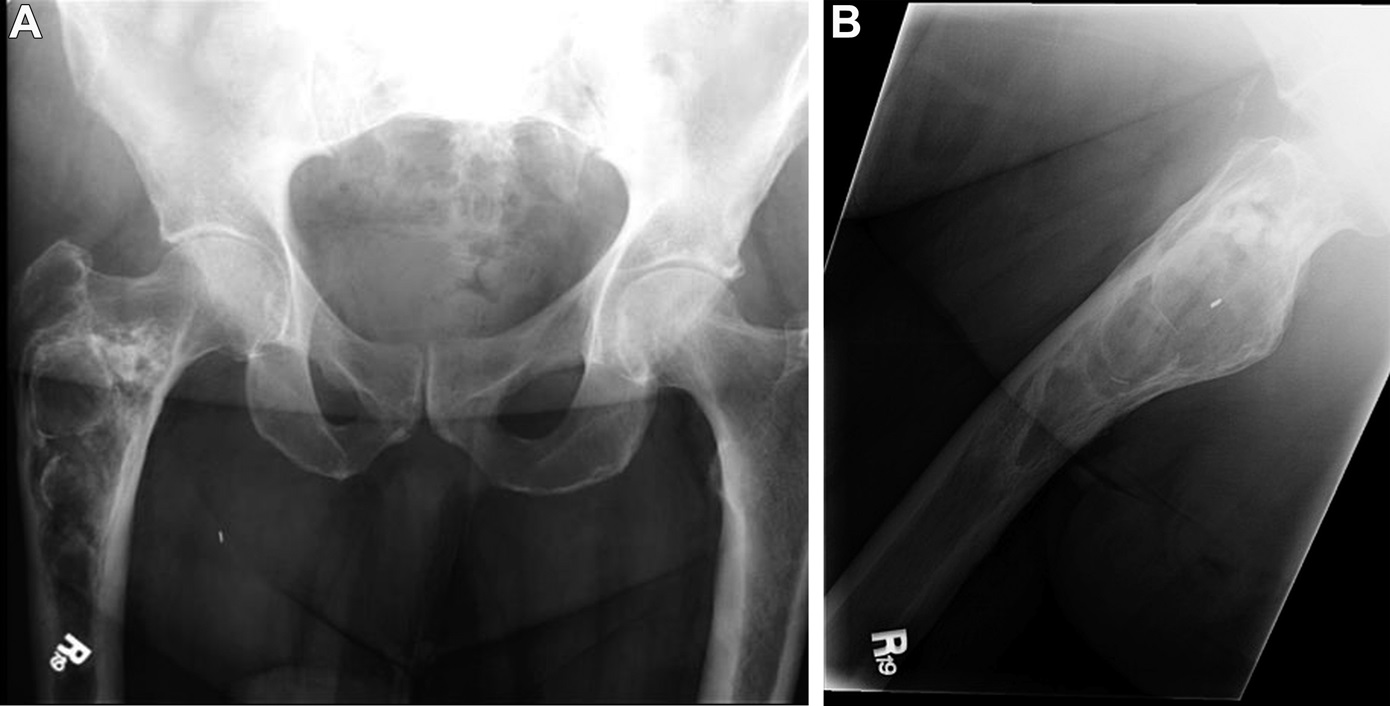
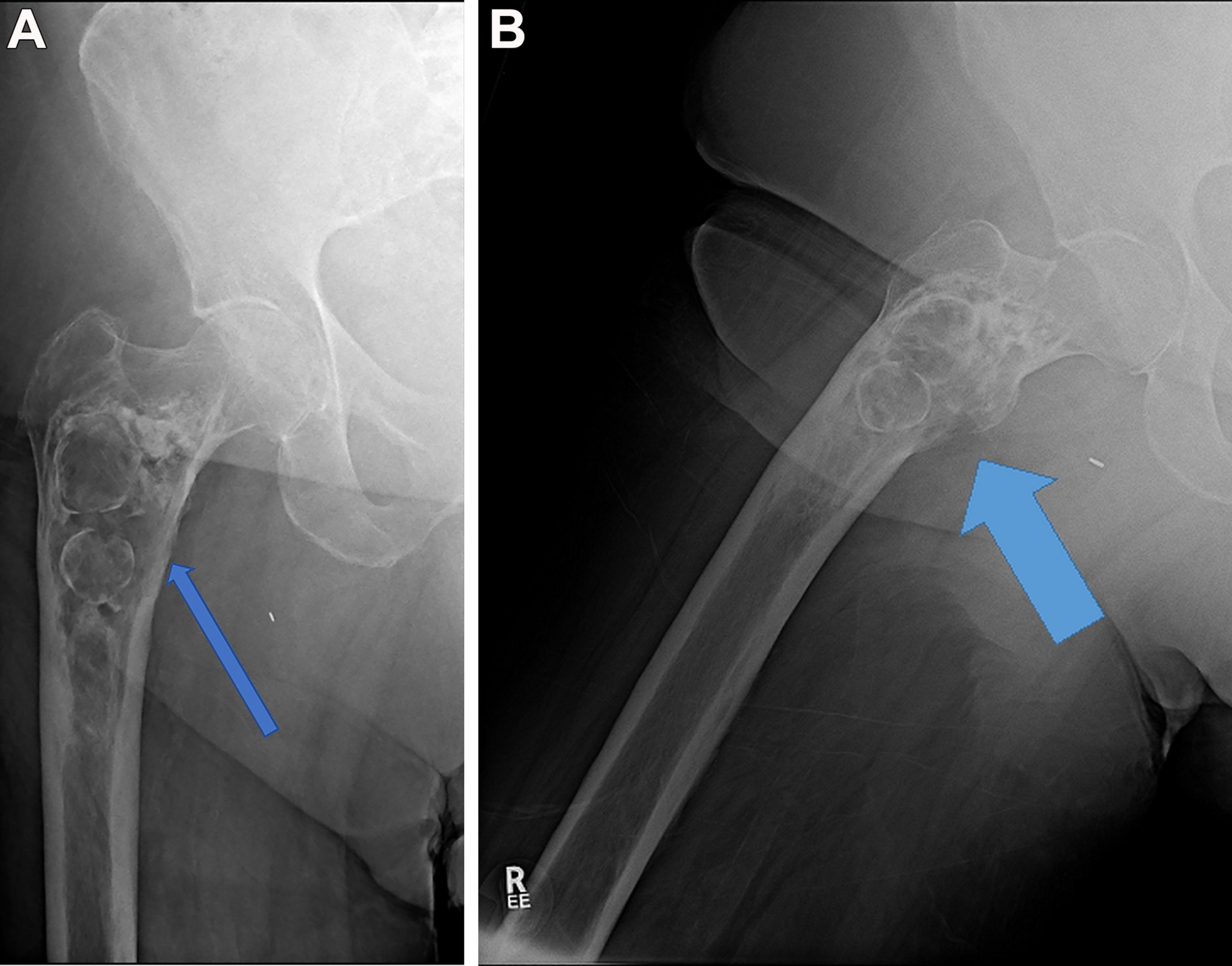
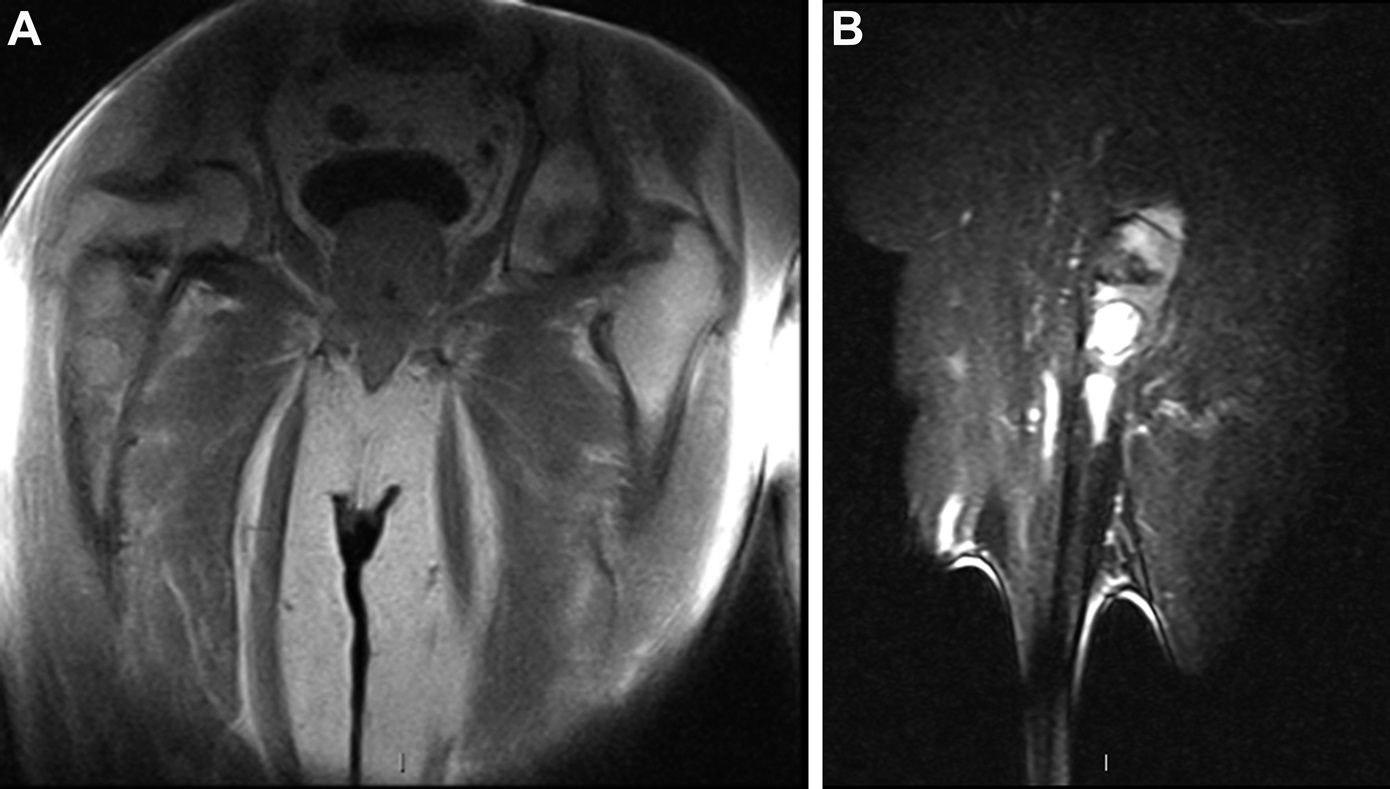

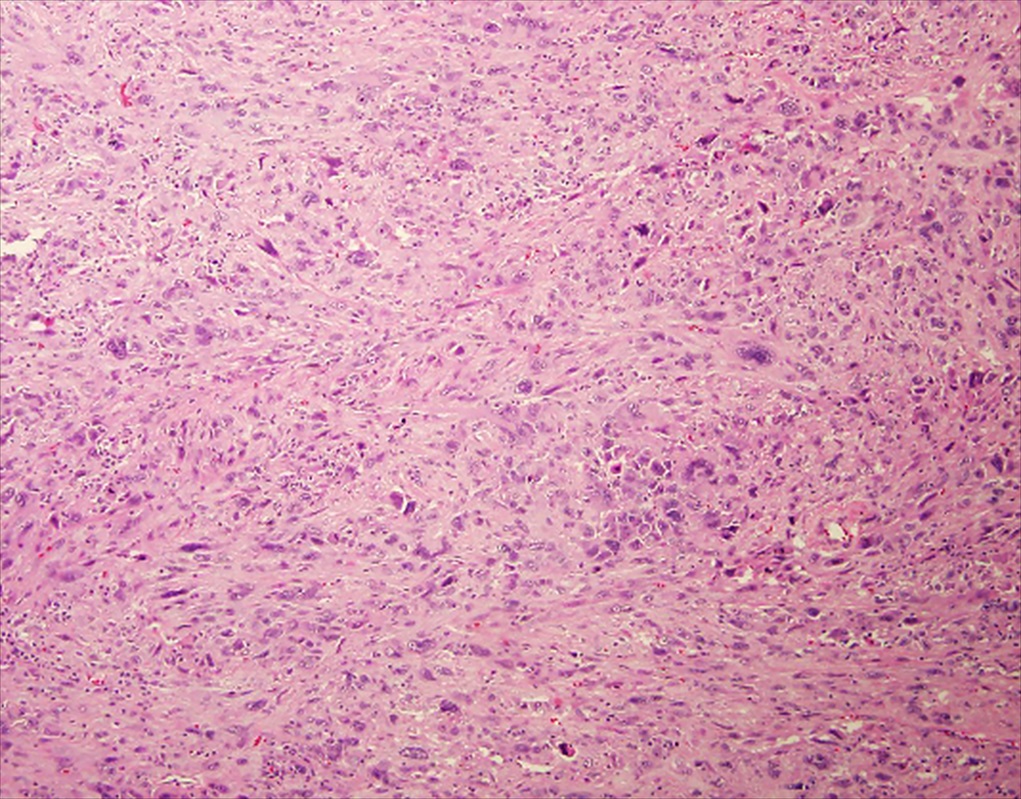
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4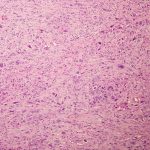 Fig. 5
Fig. 5 Fig. 6
Fig. 6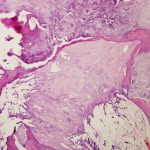 Fig. 7
Fig. 7