A Fifty-seven-Year-Old Man with Worsening Neck Pain
February 3, 2016
A fifty-seven-year-old African-American male was seen in the orthopaedic spine clinic with a one-month history of worsening neck pain. The patient noted that the onset of pain had been insidious, waking him from sleep four weeks prior to presentation without an antecedent traumatic event. He reported intermittent paresthesias in both upper extremities, with the symptoms being greater on the right side than on the left side and becoming worse during neck extension and coughing. He denied fevers, night sweats, or accelerated weight loss. He had had a 34-kg (75-lb) weight loss over six months following the treatment of stage-V chronic kidney disease secondary to type-II diabetes mellitus. The medical history was additionally positive for hypertension, obesity, gout, and obstructive sleep apnea. The patient had previously undergone the creation of an arteriovenous fistula in the right forearm, right adrenalectomy, and right knee arthroscopy. On physical examination, the patient was able to walk on the toes and heels with normal tandem gait. Cervical range of motion was near full in rotation but decreased in flexion and extension because of discomfort. The results of the Romberg and Spurling tests were negative. Motor strength was full in all major muscle groups in both upper extremities except for the deltoids, which had grade-4 of 5 strength bilaterally. Sensation was intact to light touch, with 2+ reflexes at the biceps, triceps, and brachioradialis. There was a positive inverted radial reflex and Hoffmann reflex on the right side, and both were negative on the left side. No intrinsic wasting was present. There was no clonus, and toes were downgoing on Babinski testing. Radiographs of the cervical spine demonstrated focal kyphosis at the C5 and C6 vertebral levels, with destruction of the disc space and erosion through the inferior end plate of C5 and the superior end plate of C6 (Fig. 1). Flexion and extension radiographs did not demonstrate instability. Computed tomography (CT) scans of the cervical spine demonstrated destruction of the vertebral bodies at C5 and C6, with focal canal stenosis secondary to vertebral body collapse and osteolysis. Magnetic resonance imaging (MRI) with contrast medium revealed osseous destruction of the inferior end plate of C5 and the superior end plate of C6, with collapse and retropulsion of the vertebral bodies into the spinal cord canal resulting in cervical stenosis at C5-C6 (Fig. 2). Laboratory studies demonstrated an elevated erythrocyte sedimentation rate (ESR) (91 mm/hr; normal, 0 to 15 mm/hr); an elevated, highly sensitive C-reactive protein (CRP) level (184.2 mg/L; normal 0.2 to 8 mg/L); and an elevated white blood-cell count (12.3 × 10/mL; normal, 4 to 10.3 × 10/mL). Other notable laboratory findings included a creatinine level of 7.0 mg/dL, a blood urea nitrogen level of 33 mg/dL, and a glomerular filtration rate of 9.2 mL/min/1.73 m. Blood specimens were obtained for culture, and antibiotics were withheld until the results of culture of surgical specimens were available.
On imaging, abnormal signal was noted within the intervertebral disc and bodies, consistent with discitis and vertebral osteomyelitis of C5 and C6. As the patient had also undergone hemodialysis to treat chronic kidney disease, he was diagnosed with hemodialysis-associated spondylodiscitis. Given the radiographic findings, planned staged procedures were performed, beginning with anterior incision and debridement, corpectomies of C5 and C6, and placement of a titanium interbody cage and an anterior plate spanning C4 to C7. Following the anterior procedure, the patient was maintained in a rigid cervical collar and was managed with the initiation of organism-specific intravenous (IV) antibiotic therapy (daptomycin; 6 mg/kg, three times weekly) for the treatment of Staphylococcus epidermidis, which had grown on culture of blood and wound specimens. Staged posterior cervical arthrodesis of C4 to C7 was performed seventeen days after the initial anterior procedure (Fig. 3). The patient completed a six-week course of IV daptomycin and was subsequently managed with oral amoxicillin/clavulanic acid (Augmentin; 500 mg, administered twice a day) for an anticipated one-year course of suppressive antibiotic therapy. At one year of follow-up, the patient had no residual neck pain and had returned to all previous activities, including golf. He was subsequently placed on the kidney transplant waiting list and continued to receive indefinite suppressive oral Augmentin therapy. Physical examination demonstrated decreased cervical range of motion, unchanged from the initial postoperative examination, with full motor strength and no sensation deficit. Radiographs demonstrated solid fusion, with stable implants and no subsidence.
Proceed to Discussion >>Reference: Shaw A, Boomsma SE, Johnson PC, Gloystein DM. Hemodialysis-associated spondylodiscitis of the cervical spine: A case report. JBJS Case Connect. 2015 Oct 28;5(4):e90.
Infection is a common complication in patients undergoing chronic hemodialysis, accounting for 40% of all complications. Infections present in the form of bacteremia, tunnel-site infections, catheter-site infections, endocarditis, osteomyelitis, and epidural abscesses; bacteremia is the most common complication, with an average prevalence of 29%. These complications are seen less frequently in association with permanent forms of vascular access, such as arteriovenous fistulas, which remain the standard treatment for long-term hemodialysis. Vertebral infections are infrequently encountered in patients undergoing hemodialysis (prevalence, 2.5%). The pathogenesis is hematogenous spread resulting in spinal epidural abscess or spondylodiscitis, with a predilection for the lumbar and thoracic segments. These infections are notoriously catastrophic because of rapid progression. The initial stage is characterized by severe pain; the second stage consists of spinal irritation presenting with classic physical examination findings such as the Lasègue, Kernig, and Lhermitte signs as well as neck stiffness; the third stage is marked by the appearance of neurological deficits; and the terminal stage is characterized by paralysis and paresis, particularly when there is thoracic level involvement. Radiographic evaluation remains the mainstay of diagnosis. However, the classic radiographic findings of alterations in the radiodensity of the underlying osseous structure appear only after several weeks of disease progression. For this reason, the inclusion of advanced imaging modalities offers the capability of earlier diagnosis, with MRI with contrast medium being the study of choice. After diagnosis, treatment varies largely on the basis of the pathogenesis and character of the infection. Hadjipavlou et al. reviewed the surgical treatment of spinal infections of mixed etiology and presented an algorithm of treatment based on the type of infection. According to this algorithm, epidural abscesses require surgical treatment. Primary infections can be treated with emergency laminectomy, followed by posterior instrumented arthrodeses if the spine is unstable. Secondary epidural abscesses require more extensive treatment, typically with combined anterior and posterior procedures designed to correct the spinal deformity and stabilize the spine, the order of which is determined by the location of the abscess with regard to the spinal cord. Patients presenting with early spondylodiscitis without substantial bone destruction can be managed with immobilization and long-term antibiotic therapy. However, in the setting of extensive bone loss and structural deformity, anterior and posterior decompression and arthrodeses with instrumentation are recommended. The goals of surgical treatment include drainage of the abscess with debridement of necrotic tissue, decompression of neural components, stabilization of the spine, and appropriate antibiotic therapy. Following debridement, reconstructive procedures to restore vertebral height are often indicated. Depending on the amount of correction needed, autogenous tricortical iliac crest bone graft can be used, whereas larger corrections may require vascularized rib or fibular strut grafts. In addition, expandable titanium interbody cages have been utilized increasingly because of the customizability of height and deformity correction without the added morbidity of autograft harvest. Recent data have supported the ability of interbody cages to maintain alignment without progressive collapse. Specifically, the use of titanium has been shown to result in decreased biofilm adherence compared with stainless steel implants, resulting in decreased infection rates. Following surgery, continued treatment with IV antibiotics is recommended for a minimum of six weeks but for as long as twelve weeks, depending on the type of infection as well as on various patient-related considerations. Following completion of the course of IV antibiotics, long-term oral antibiotic therapy has been recommended secondary to persistent bacterial colonization of implants.
Reference: Shaw A, Boomsma SE, Johnson PC, Gloystein DM. Hemodialysis-associated spondylodiscitis of the cervical spine: A case report. JBJS Case Connect. 2015 Oct 28;5(4):e90.
Metastatic renal cell carcinoma
Metastatic lung carcinoma
Osteoblastoma
Chordoma
Hemodialysis-associated spondylodisctis


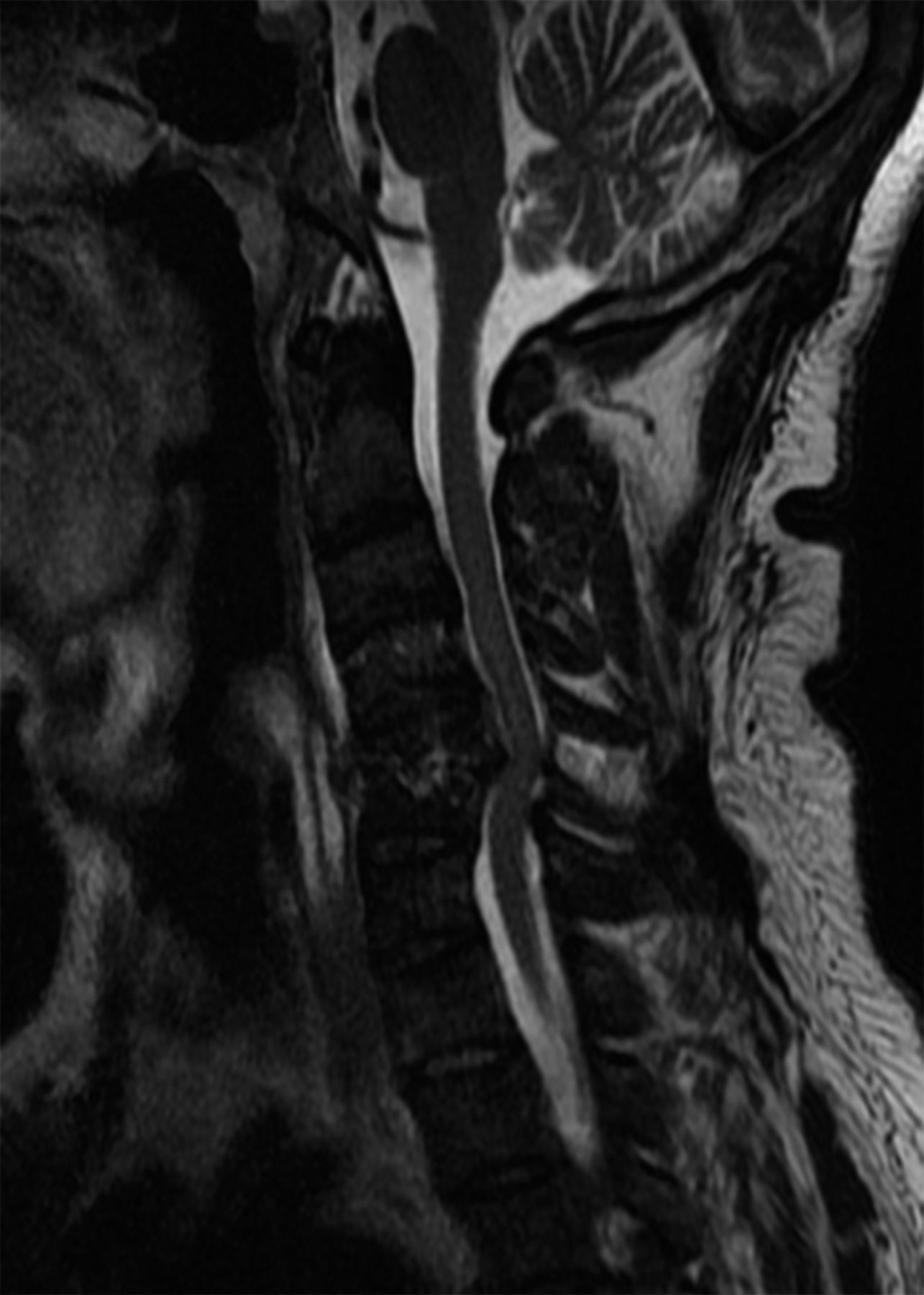
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3