A 23-year-old right-hand-dominant man was referred after 6 months of unrelenting left elbow pain, which had begun after he pulled himself onto a boat while scuba diving. He described the pain as sharp and throbbing, most noticeable in the morning and at night, and localized to the radial side of the proximal aspect of the left forearm. The pain was aggravated by activity, relieved with rest, and managed with acetaminophen. The medical and family histories were noncontributory. He reported loss of strength and decreased range of motion of the elbow. He had no constitutional symptoms.
Physical examination of the left upper extremity showed normal sensation and decreased strength (4 of 5) in wrist flexion and extension, elbow flexion and extension, and supination and pronation, likely because of discomfort. Left-sided supination was 40° less than the right side. There was no loss of pronation. Tenderness was noted over a palpable mass at the lateral aspect of the arm overlying the proximal aspect of the radius.
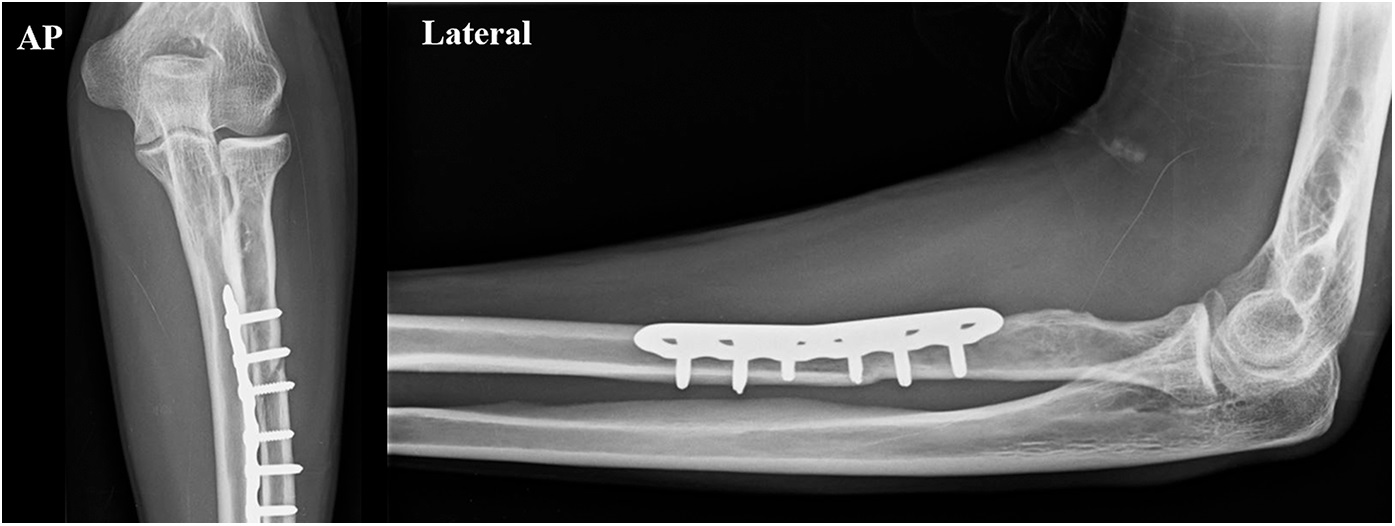
Anteroposterior and lateral radiographs showed an expansile lytic metadiaphyseal lesion involving the proximal aspect of the left radius and the radial head (Fig. 1). Magnetic resonance imaging (MRI) depicted a lobulated and expansile solid lesion involving the proximal aspect of the radius (Fig. 2). A core needle biopsy is shown in Figure 3.
The combination of radiographic findings and histology was interpreted as a giant cell tumor (GCT) of bone. Because of the marked destruction and expansion of the radius, we believed that intralesional curettage would provide less effective local tumor control than resection. The decision was made to perform resection and reconstruction with an osteoarticular allograft and internal fixation.
The left upper extremity was prepared and draped in the usual sterile fashion. A tourniquet was inflated to 250 mm Hg. A volar (Henry) approach to the radius was performed. Multiple small vessels of the tumor were ligated or cauterized. The pronator teres and biceps tendons were released and tagged. The annular ligament was incised along with the joint capsule, but the interosseous ligament was preserved because the attachment was distal to the planned resection. The posterior interosseous nerve was visualized within the supinator, and it was protected. An osteotomy of the radius was performed 7.5 cm from the capitellum with a small oscillating saw that cut on a sharp, oblique angle along the flat surface of the radius to allow plate fixation with compression screws. The specimen, which measured 25 mm anteroposteriorly and 22 mm mediolaterally, was removed and sent to pathology. The tourniquet was released for >30 minutes before reconstruction, during which time the wound was irrigated and hemostasis was obtained.
Reconstruction was performed using a fresh-frozen allograft from the proximal aspect of the radius without articular cartilage cryopreservation. The graft was cut obliquely to match the osteotomy site of the native radial surface. A 6-hole 3.5-mm plate was placed along the ulnar aspect of the radius, with the proximal end distal to the bicipital tuberosity. Two proximal screws were placed, and the allograft was inserted in the radius with a well-aligned radiocapitellar joint, allowing anterior subluxation of 2 to 3 mm of the proximal aspect of the radius in supination. The plate was compressed proximally with a screw and fixed distally with 1 nonlocking and 2 locking screws. This was considered by the surgical team to be adequate fixation. The annular ligament was reconstructed. After trimming the biceps allograft tendon, the biceps was reattached with #2 FiberWire suture (Arthrex) and a Krackow stitch. The pronator teres was reattached to the allograft. The supinator was reattached to the plate because there was no remaining attachment on the allograft. A deep drain was inserted, and the elbow was placed in 90° of flexion with a posterior splint that extended to the wrist with the forearm in a neutral position. The patient was discharged home the next day.
The resection specimen measured 8.5 × 4.2 × 3.5 cm, with the GCT beginning 2 cm from the proximal aspect of the cartilage surface. The intraosseous lesion measured 5.1 × 3.5 cm. Routine histologic testing confirmed the diagnosis of GCT and negative margins.
The patient had an uncomplicated recovery and pursued occupational therapy for strengthening and range-of-motion exercises, including warm compresses in a supination stretch, weighted pronation and supination stretching, and brachioradialis/biceps/triceps/grip weighted exercises. Five months after surgery, the baseline strength had improved (5 of 5) in all forearm, wrist, and hand muscles, as had elbow, forearm, and wrist range of motion. Physical examination showed a healed incision, no tenderness to palpation on either epicondyle, and no joint subluxation of the radial head with pronation and supination. The elbow joint was stable to varus and valgus stress. Active left elbow extension and flexion were 0° and 145°, respectively, without pain. Pronation was full, and supination had improved from 55° preoperatively to 70° postoperatively. Radiographs at 5 months after surgery showed a healing fracture with no signs of allograft or instrumentation failure (Fig. 4). Full union had been achieved at the 17-month follow-up (Fig. 5), and there were preserved strength and range of motion and a stable joint at 54 months.
Proceed to Discussion >>Reference: Nayar SK, Dein EJ, Spiker AM, Bernard JA, Zikria BA, Weber KL. Resection of a giant-cell tumor of the proximal aspect of the radius with osteoarticular allograft reconstruction: a case report. JBJS Case Connect. 2018 Jan-Mar;8(1):e7.
We have described a case of osteoarticular allograft reconstruction of the proximal aspect of the radius after resection of an aggressive GCT. This approach allows maintenance of elbow and wrist stability and a lower incidence of recurrence compared with intralesional curettage without reconstruction.
We found no other reports in the literature of allograft reconstruction in the proximal aspect of the radius after resection of GCT, likely because of the low incidence of GCTs in this location. These grafts, however, have been used to treat other impairments of the proximal aspect of the radius, including those seen in an Essex-Lopresti injury, symptomatic radial head translation, and posttraumatic osteoarticular loss. Alternatives to osteoarticular allografts for radial reconstruction include vascularized and nonvascularized grafts for aneurysmal cysts, allograft prosthesis composites for osteosarcoma, and endoprostheses for GCT. To our knowledge, the results of these alternative methods have not been compared with those of osteoarticular allografts.
Osteoarticular allografts have been used widely at other anatomic sites, including the proximal aspect of the tibia, the proximal and distal aspects of the femur, and the proximal aspect of the humerus. Although the benefits of allografts include bone stock restoration, biologic bone union, and soft-tissue attachment, there are many drawbacks, including healing times of 1 to 4 years, fracture rates as high as 45%, risk of disease transmission, and perioperative infection rates of ≤10%. Reconstruction with osteoarticular allografts is technically challenging, and there is a 16% rate of required resurfacing arthroplasty for allografts placed in weight-bearing joints. Graft survival rates are low but comparable with alternative treatments for patients who require resection and reconstruction of the proximal aspect of the femur (77% to 86% at 10 years), the distal aspect of the femur (65% at 10 years), the proximal aspect of the tibia (65% at 10 years), and the proximal aspect of the humerus (55% at 10 years). Considering that the radiocapitellar joint is non-weight-bearing, is less prone to arthritic degeneration, is easier to reconstruct technically, and has adequate soft-tissue coverage compared with other joints, use of an allograft may be a better reconstructive option for the proximal aspect of the radius in the setting of resection.
An important technical point for allograft reconstruction of the proximal aspect of the radius involves understanding the anatomy of the interosseous membrane, which is vital for forearm stability. The interosseous membrane arises approximately 7.7 cm distal to the radial head and inserts approximately 13.7 cm from the olecranon tip. If resection of the proximal aspect of the radius is >7.5 cm from the radial head, forearm stability should be checked. If the forearm is unstable, one should consider repairing or reconstructing the interosseous membrane during allograft reconstruction.
The histologic differential diagnosis of GCT includes other conditions that feature giant cells, such as giant-cell reparative granuloma, brown tumor, osteoblastoma, chondroblastoma, nonossifying fibroma, and osteosarcoma. Radiographic features consistent with GCT include low-to-intermediate signal intensity on T2-weighted MRI (Fig. 2), metaphyseal and epiphyseal involvement at a closed growth plate, shared borders with articular cartilage, well-defined margins, and a noncentral origin. When treating patients with GCT, clinicians should be aware that pulmonary metastasis, although rare, has been reported, as well as ossification of surrounding tissue, which occurs in approximately 1.5% of cases and may predispose to local relapse.
In summary, at 5 months after osteoarticular allograft reconstruction following GCT resection, our patient had improved strength and range of motion and good joint stability. There were no signs of instrumentation failure or malunion, and the radiocapitellar joint remained intact. At 17 months, there was full union of the graft to native bone; at 54 months, there was preserved function and a stable radiohumeral joint. We have described an acceptable alternative to current methods of reconstruction of the proximal aspect of the radius. We believe that this method combines the strengths of other approaches to minimize the risk of tumor recurrence and restore joint function.
Reference: Nayar SK, Dein EJ, Spiker AM, Bernard JA, Zikria BA, Weber KL. Resection of a giant-cell tumor of the proximal aspect of the radius with osteoarticular allograft reconstruction: a case report. JBJS Case Connect. 2018 Jan-Mar;8(1):e7.
What is the diagnosis?
Aneurysmal bone cyst
Langerhans cell histiocytosis
Tenosynovial giant cell tumor
Giant cell tumor of bone
Granulomatous inflammation consistent with Mycobacterium marinum infection

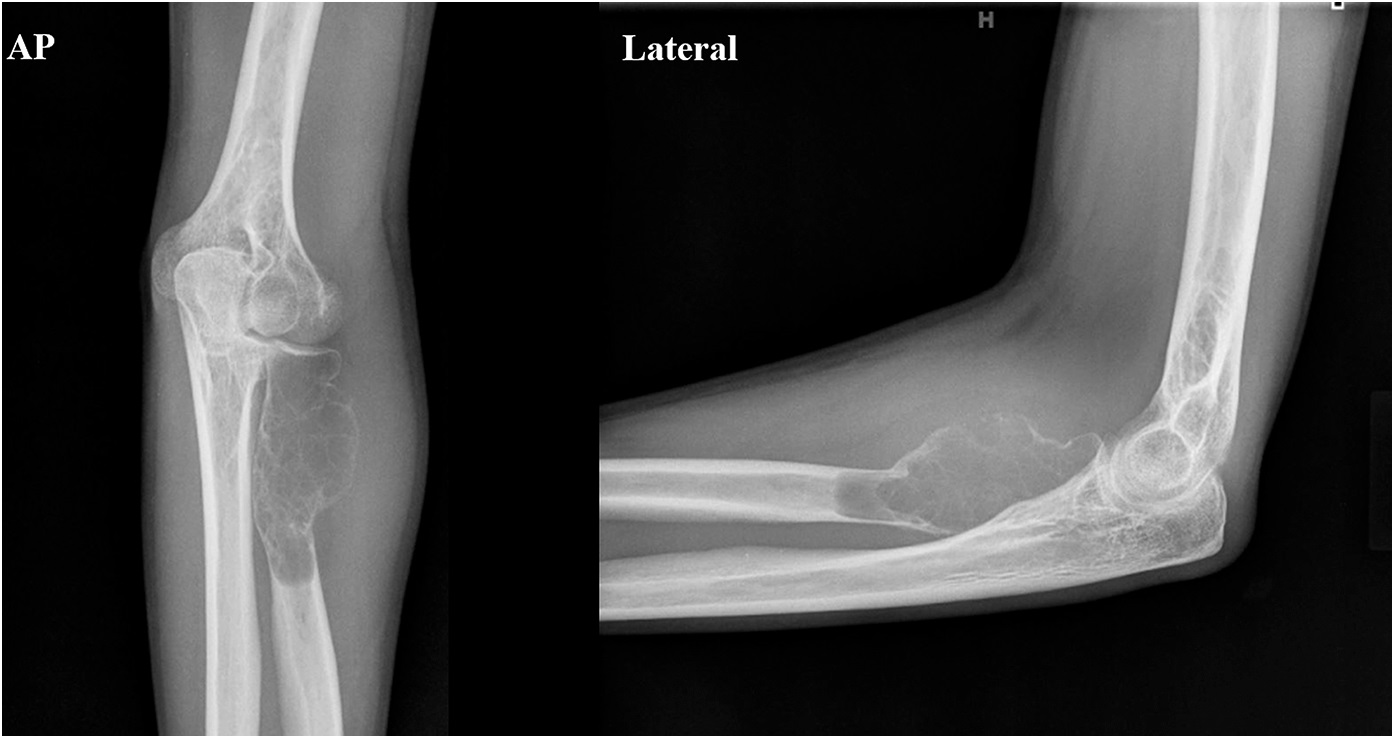
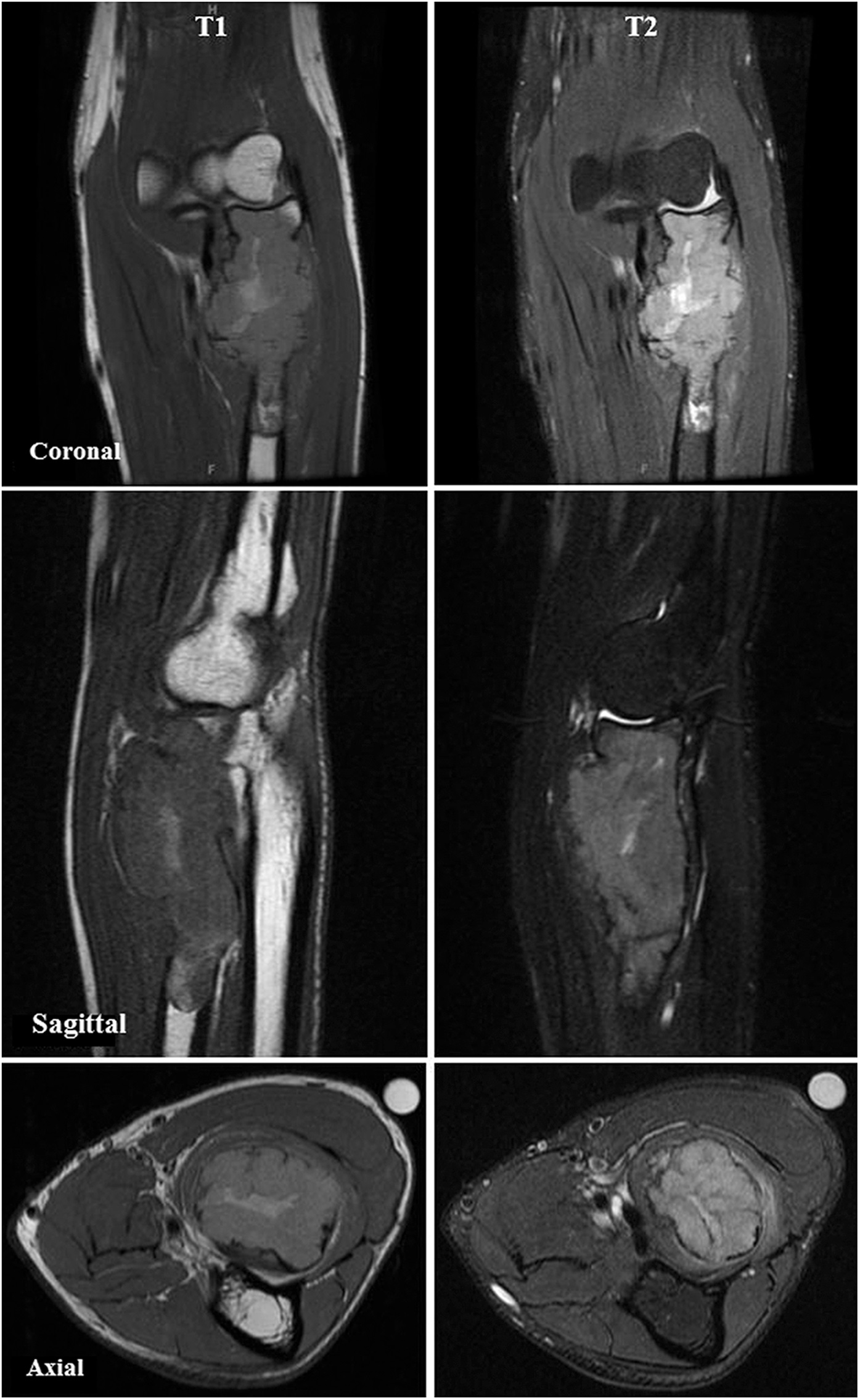

 Fig. 1
Fig. 1 Fig. 2
Fig. 2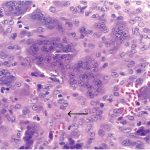 Fig. 3
Fig. 3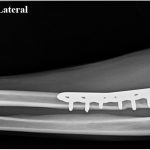 Fig. 4
Fig. 4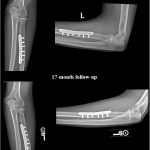 Fig. 5
Fig. 5