In September 2009, a seventy-seven-year-old woman presented with the primary symptom of a clicking sound in the right hip. In 1990, she had undergone metal-on-polyethylene (MOP) arthroplasty of the right hip for osteoarthritis with an anatomic medullary locking femoral stem (10 mm in size, cobalt-chromium alloy), a tri-lock cup (52 mm in diameter, titanium alloy), a manufacturer-designed acetabular cup system liner (conventional type of polyethylene), and a femoral head (28 mm in diameter, cobalt-chromium alloy) (DePuy Orthopaedics). The postoperative course had been uneventful. She did not notice any gait disturbance but used a T cane for balance. She did not have a history of any neoplasm, and no suspicious pigmented skin lesions were evident. Physical findings showed a good range of motion (flexion, 120°; abduction, 40°) in the operated hip, but a clicking sound was present with passive motion. Radiographs revealed bone-ingrown fixation of both the acetabular and femoral metal implants; however, direct contact of the metal head to the metal cup caused by eccentric wear of the polyethylene liner was suspected (Fig. 1).
We recommended revision surgery; a large mass was detected in the right pelvis during the preoperative assessment. Computed tomography (CT) and magnetic resonance imaging (MRI) (Figs. 2-A and 2-B) revealed the presence of an intrapelvic mass measuring 110 × 140 mm in diameter on the right side, which appeared to elongate anteriorly to the right hip joint (Fig. 2-C). Although the mass was palpable in the right lower abdomen, there were no abdominal or genitourinary symptoms.
The patient reported that this abdominal mass had been examined by internists at another hospital in 2001, and they had assured her that the mass was not malignant even though its origin was unclear.
Revision arthroplasty was performed via a posterolateral surgical approach in January 2010. The intraoperative findings included catastrophic breakage of the polyethylene liner and partial breakage of the rim of the metal cup, which indicated failure of the locking mechanism of the cup for the liner. The acetabular cup and femoral stem were well fixed to bone, and limited osteolysis was observed around the stem insertion. We did not explore the anterior aspects of the joint, but we performed curettage within the joint and replaced the polyethylene liner (with the same type of polyethylene that had been used at the primary operation) with use of bone cement. The laboratory culture results were negative. The patient had an uneventful recovery and was discharged when she was able to walk with the aid of a T cane.
One month after surgery, the patient returned to our hospital because of a posterior dislocation of the hip. We repositioned the joint under fluoroscopic guidance. However, one week later, fluctuance developed around the greater trochanter at the operative site. We aspirated 90 mL of dark red fluid from this swollen area. Twice-monthly aspiration was required over the next six months. Multiple cultures were negative. There was no increase in white blood-cell count or in C-reactive protein level.
MRI indicated that the trochanteric cystic lesion connected to the hip joint space and also allowed visualization of the development of a similar horizontal demarcation line in both the trochanteric cystic lesion and the intrapelvic mass (Figs. 3-A and 3-B), suggesting that the content within the mass was flowing back from the mass to the joint space.
In September 2010, we again performed curettage within the hip via the same approach and placed an indwelling catheter in the intrapelvic mass. Initial results following mass volume reduction were fair, but fluid accumulation recurred after removal of the drainage tube. In November 2010, the mass was resected via an iliopectineal surgical approach. A black mass with a diameter of approximately 140 mm was excised from under the iliopsoas fascia (Fig. 4). The mass connected to the hip joint at the anterior acetabular edge along the iliopsoas tendon underneath the inguinal ligament. After excision of the mass, the joint space was irrigated with use of jet lavage. Macroscopically, the excised mass had a thick, black wall of connective tissue (Fig. 5).
Histology of the mass is seen in Figure 6.
The histology revealed black deposits suggestive of metal debris, in addition to foam cells and multinucleated giant cells in the connective tissue, consistent with the appearance of a pseudotumor. We did not find any perivascular lymphocytic aggregates. Metal analysis of fluid previously aspirated showed a high concentration of titanium-6aluminum-4vanadium (Ti6Al4V) alloy (titanium, 500 mg/g; aluminum, 26 mg/g; vanadium, 18 mg/g; cobalt, <0.5 mg/g; chromium, <0.5 mg/g, likely from the acetabular component).
At the most recent follow-up, the patient was walking with a T cane; she had had no symptoms of joint pain in the right hip or from the right lower abdominal mass for the two years following surgery.
Proceed to Discussion >>Reference: Yoshihara Y, Shiromoto Y, Tatsumi M, Hirano M, Kawano T, Arino H, Osako M, Nemoto K. Backflow from a metallosis-induced intrapelvic mass into a revision hip arthroplasty: a case report. JBJS Case Connect. 2013 Jul 10;3(3):e66.
There have been several reports of patients with intrapelvic masses associated with total hip arthroplasty. Only two reports have described masses due to metallosis following polyethylene liner breakage. Mak et al. reported a case quite similar to ours: the patient developed an intrapelvic mass after MOP total hip arthroplasty. Radiographs revealed eccentric polyethylene liner wear; however, the excision of the mass was primarily performed by gynecologists, who believed it to be an ovarian tumor. During complete excision, the mass, which contained black metal debris, was observed to have a pedicle underneath the inguinal ligament that led to the anterior joint capsule. Additional revision hip arthroplasty was not done because the patient refused. Murgatroyd also reported a case of an intrapelvic cystic mass. Radiographs revealed a polyethylene liner with eccentric wear following MOP total hip arthroplasty. At the revision surgery, substantial metallosis was present, and a large bone defect connecting to the cystic cavity was also observed behind the delaminated cup. A partial excision of the cystic wall and irrigation of the cavity were performed to remove the contents, followed by an acetabular component revision. Good clinical results without a recurrence were demonstrated.
In our patient, the intrapelvic mass was present eleven years after the primary total hip arthroplasty, even though radiographs did not demonstrate a broken polyethylene liner. This suggests that the development of the mass was initially caused by a reaction to polyethylene wear and then followed by the accumulation of black metallic debris. The histologic studies revealed metal depositions, as well as foam cells and multinucleated giant cells, as foreign body reactions without the perivascular aggregates of lymphocytes seen in ALVALs (Fig. 6). These findings also suggest that the etiology of the mass was related to a granulomatous reaction to wear particles rather than an immunological response to metal debris.
Complete resection of asymptomatic intrapelvic masses may not always be necessary. Leigh et al. successfully reduced the size of an intrapelvic mass without metallosis by simply revising the polyethylene liner and curetting its contents. They also suggested that removal of the source of the wear debris by revision arthroplasty should result in resolution of the granuloma. Certainly, revision surgery itself may be successful for a solid ALVAL or a granuloma caused by stimulation of metal ions or high amounts of polyethylene debris, but not for a case such as ours, with high amounts of metallic fluid in the cavity. We believe that, in addition to sufficiently removing the metallic contents of the mass, it might be advantageous to perform revision of the polyethylene liner. Complete mass excision and sufficient mass cavity irrigation might demonstrate favorable results. We chose the former procedure because the mass was a bilocular cyst and it would have been difficult to sufficiently remove the metallic contents with a small exploration. This morphologic feature may also be one of the reasons why catheter drainage of the mass contents did not work effectively.
In conclusion, we propose that revision of the components combined with mass excision may be the best approach in cases of intrapelvic masses resulting from macroscopic metallosis. At a minimum, sufficient elimination of the metallic content is necessary. Because our patient was followed for only two years, the treatment results cannot be considered definitive; observation is ongoing in this patient.
Reference: Yoshihara Y, Shiromoto Y, Tatsumi M, Hirano M, Kawano T, Arino H, Osako M, Nemoto K. Backflow from a metallosis-induced intrapelvic mass into a revision hip arthroplasty: a case report. JBJS Case Connect. 2013 Jul 10;3(3):e66.
What is the diagnosis?
Metastatic malignant melanoma
Pigmented (melanotic) schwannoma (neurilemmoma)
Pseudotumor related to metal debris
Aseptic lymphocyte dominant vasculitis-associated lesion (ALVAL)
Gossypiboma (surgical sponge from previous operation)

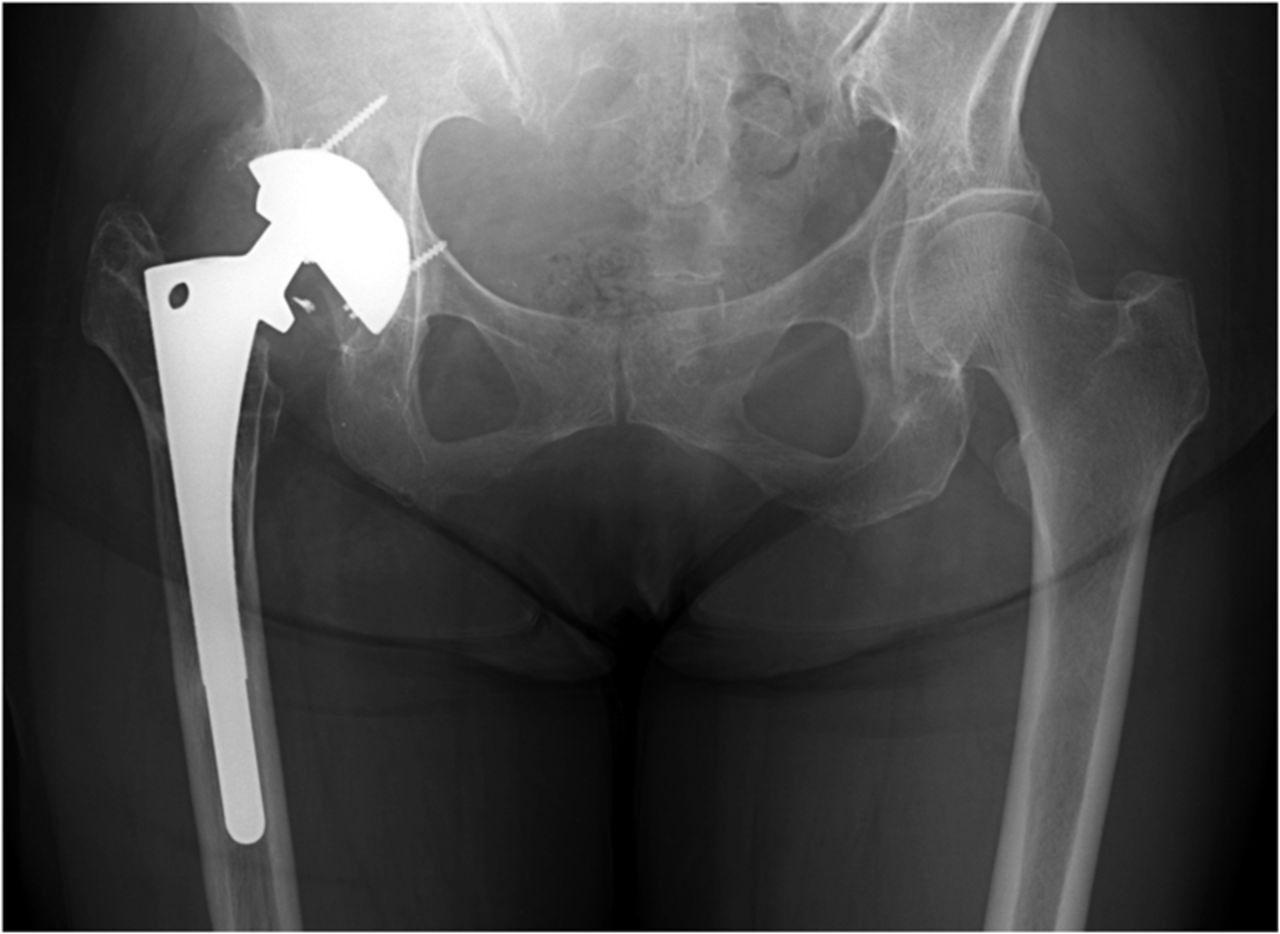
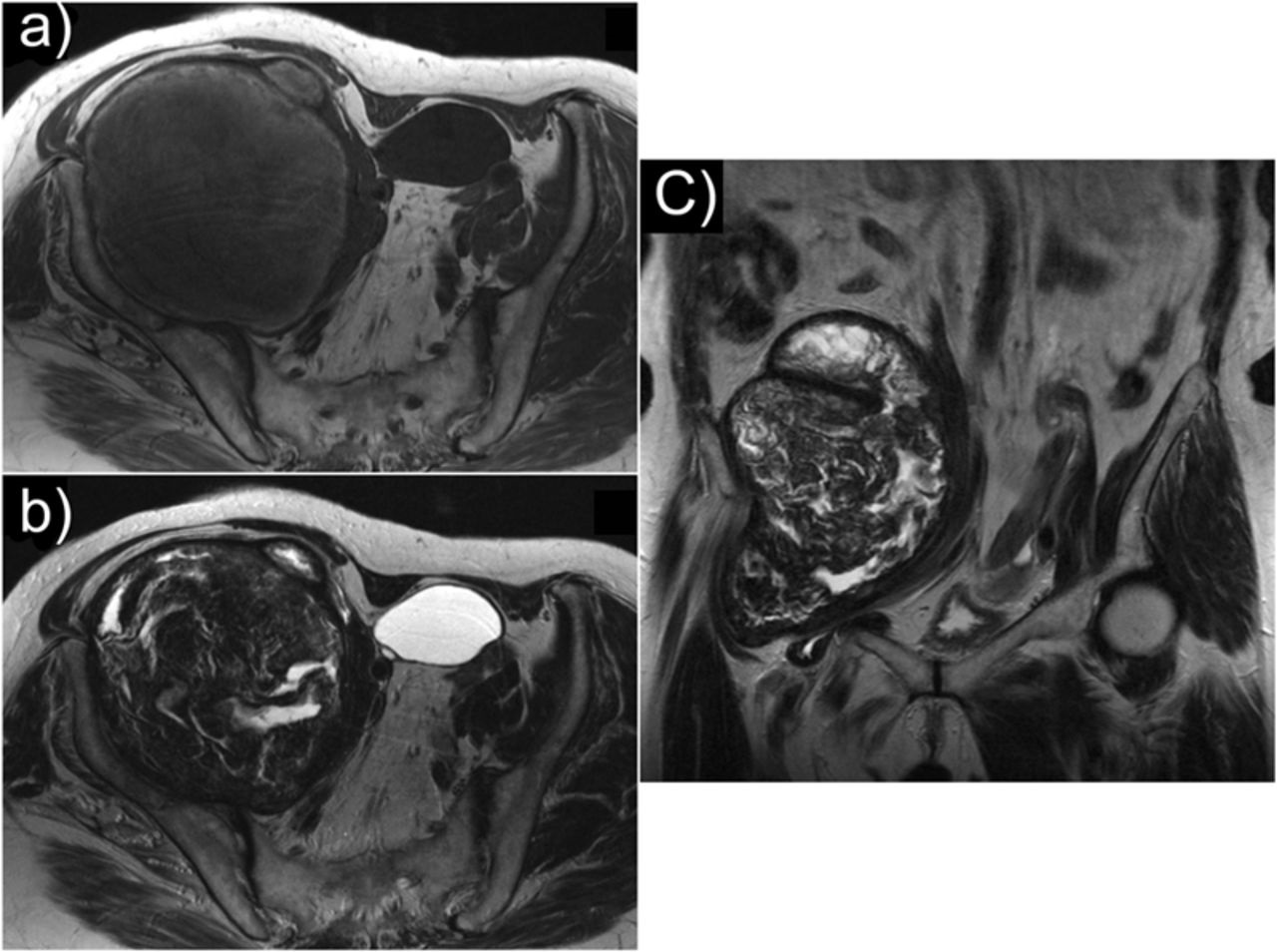
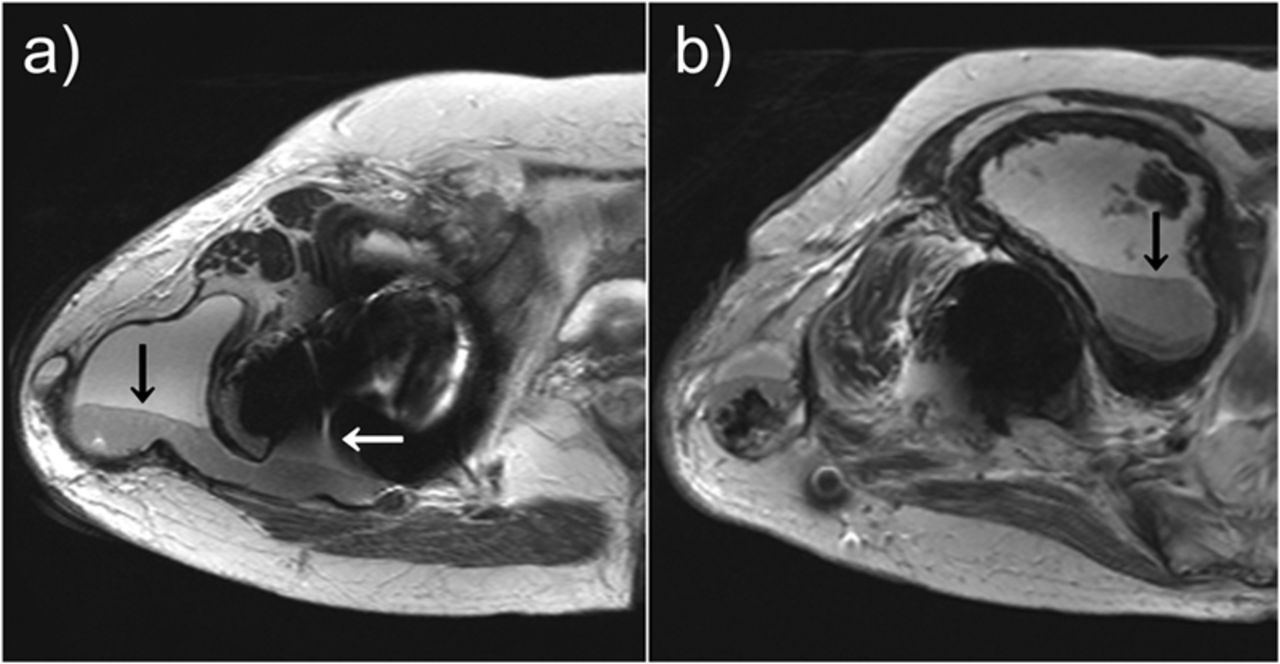

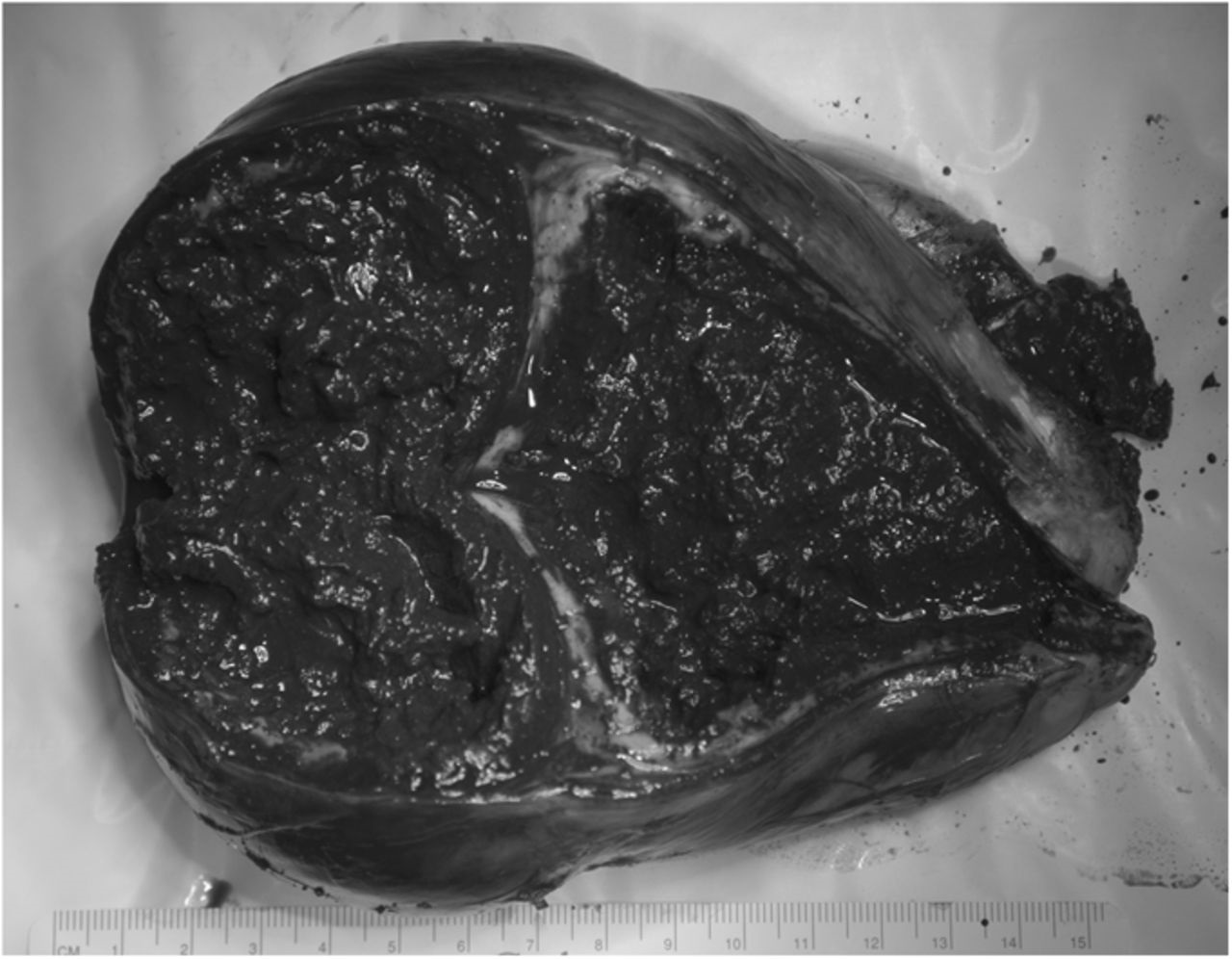
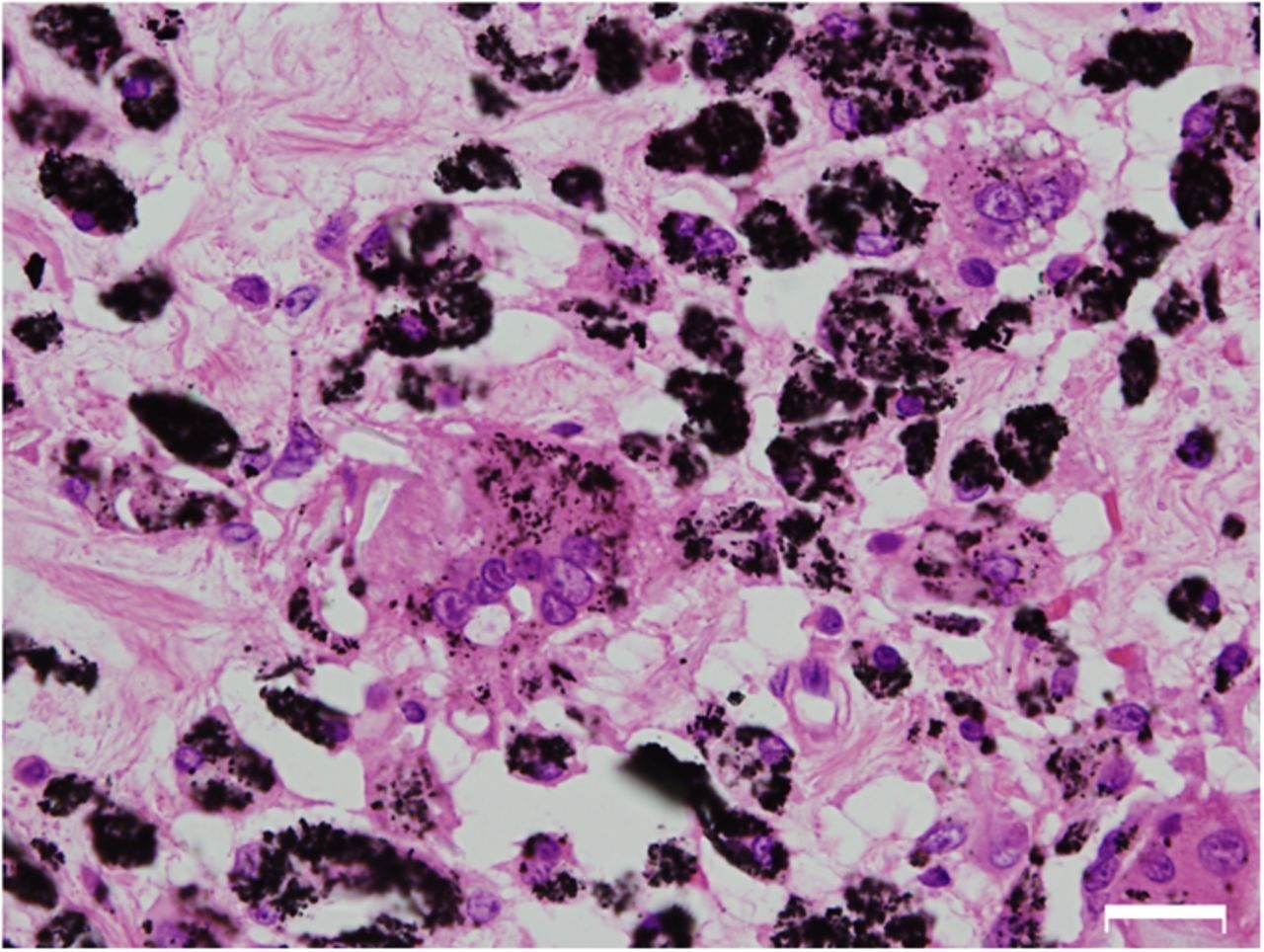
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4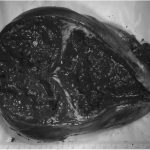 Fig. 5
Fig. 5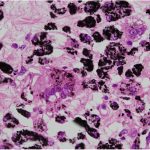 Fig. 6
Fig. 6