An otherwise-healthy 9-year-old girl developed a low-grade fever and right hip pain over a period of 48 hours, with inability to bear weight. She reported a fall during a basketball game the day before symptom onset but did not recall any hip pain immediately following the fall. After hip ultrasonography at an outside institution was interpreted as showing a large effusion (Fig. 1), she was transferred for further care. On arrival, she was febrile, with a temperature of 38.2°C, and physical examination revealed exquisite pain with any hip motion and inability to bear weight. There was no skin rash, lymphadenopathy, or hepatosplenomegaly. She had no pain in other joints. Laboratory work-up revealed a peripheral WBC (white blood cell) count of 9.85 × 103/μL, ESR (erythrocyte sedimentation rate) of 18 mm/hr, and CRP (C-reactive protein) of 7.56 mg/L. Radiographs of the pelvis and right hip were unremarkable. Ultrasound-guided right hip aspiration yielded bloody fluid with 611,932 RBC (red blood cells)/μL, 49,529 WBC/μL with 92% neutrophils, a negative Gram stain, and no crystals.
Given the patient’s fairly unusual presentation of an acutely irritable hip, fever, and a bloody joint aspirate all following a low-energy fall, MRI (magnetic resonance imaging) of the hip was performed. The MRI revealed a 1.3 × 2.2 × 2-cm intracapsular lesion anterior to the femoral neck, with a thin T2-hypointense rim and some intrinsic T1 hyperintensity. No blooming artifact was identified on gradient-echo localizer images, and no substantial post-contrast internal enhancement was noted. Additionally, mild enhancing edema was seen within the right pectineus and adductor brevis muscles. No osseous abnormalities or signs of osteomyelitis were identified (Fig. 2 and Fig. 3).
Given the acuity of the presentation, 49,500 WBC/μL in the synovial aspirate, and the mass identified on MRI, a recommendation for operative irrigation of the hip and excision of the mass was made and the parents decided to proceed. The hip was approached through the Smith-Petersen interval and an anterior capsulotomy was performed, revealing dark bloody fluid. A well-circumscribed nodular pedunculated lesion was readily identified, excised in its entirety with some of the capsular attachment, and submitted for pathologic evaluation. No intraoperative frozen section was obtained. Examination of the joint at this point revealed healthy-appearing femoral head cartilage and no other lesions. The remainder of the synovium appeared entirely normal.
Grossly, the resected material was soft and pink-tan with red-brown areas (Fig. 4). Microscopically, there were nodules of hypercellular tissue containing sheets of small to intermediate-sized mononuclear cells with round to ovoid nuclei, inconspicuous nucleoli, and moderate amounts of cytoplasm (Fig. 5-A). Interspersed multinucleated giant cells and occasional lymphocytes and pigment-laden mononuclear cells were present. There were areas of eosinophilic fibrinoid material; aggregates of apoptotic cells; sheet-like areas with nuclear karyolysis, pyknosis, and cytoplasmic eosinophilia (resembling recent infarction); and frequent collections of neutrophils (Fig. 5-B). Distended venous channels and interstitial hemorrhage were present in these areas. Special stains for microorganisms were negative. Immunohistochemical staining revealed patchy staining for D2-40 and no staining for desmin. Cytogenetic analysis of resected material showed a normal female karyotype (46,XX[20]). Synovial fluid cultures, both from the initial aspiration and from an intraoperative sample, were negative. A Lyme antibody ELISA (enzyme-linked immunosorbent assay) was also negative.
The biopsy was interpreted as a localized tenosynovial giant cell tumor.
The patient was afebrile and comfortably ambulatory on postoperative day 1, and was discharged home. Eighteen months postoperatively, she remained completely asymptomatic, walking without a limp.
Proceed to Discussion >>Reference: Saadat E, Vargas SO, Anderson M, Glotzbecker M. Pediatric intra-articular localized tenosynovial giant cell tumor presenting as an acutely irritable hip: A case report. JBJS Case Connect. 2016 Jul 27;6(3):e60.
We present a case of a previously undiagnosed localized tenosynovial giant cell tumor of the hip in an otherwise healthy 9-year-old girl with a highly unusual presentation resembling a septic hip, and characterized microscopically by neutrophils interspersed within an otherwise histologically classic appearance of such a tumor.
Common clinical symptoms associated with intra-articular tenosynovial giant cell tumor are pain (in 79% to 90% of cases) and swelling (72% to 79%). Joint dysfunction (26% to 28%) and a soft-tissue mass (6% to 19%) are less common. It is quite unusual for patients with this condition to have an acute presentation: in a study of 166 cases of pigmented villonodular synovitis (PVNS) by Myers and Masi, the mean duration of symptoms prior to presentation was 10 months (range, 1 to 30 months) for localized intra-articular disease, and no patients in that group presented with acute symptoms (a duration of only days). It is unclear why our patient presented with an acutely irritable hip despite having had no antecedent symptoms. Many diffuse tenosynovial giant cell tumors present with hemarthrosis, and it is conceivable that the acute presentation in this case was due to torsion and/or bleeding of the lesion secondary to the patient’s fall the day before symptom onset. The histologic evidence of recent infarction and interstitial blood supports that theory.
The lesion in the present case exhibited several characteristic features of tenosynovial giant cell tumor on MRI, including a localized synovially based mass without osseous involvement and prominent low signal intensity on T2-weighted images. Interestingly, no blooming artifact was identified on gradient-echo images, but the lesion demonstrated some intrinsic T1 hyperintensity, suggestive of the possibility of bleeding and hemosiderin deposition; only the former was histologically prominent in the resected tissue. Notably, the lesion was also visible on the pre-aspiration ultrasonography, but that was only noticed in hindsight after the mass was identified on MRI.
The combination of a bloody synovial fluid aspirate and an intracapsular lesion in the hip with MRI characteristics of tenosynovial giant cell tumor made that diagnosis likely. However, our patient presented with 2 of the 4 Kocher criteria for a septic joint (fever and inability to bear weight), and the synovial fluid WBC count was 49,529; thus, a septic hip could not be safely ruled out. Additionally, Lyme arthritis remained in the differential diagnosis given the mild myositis observed on MRI, which has been described in cases of pediatric Lyme arthritis.
A literature search revealed only 1 reported case of pediatric intra-articular tenosynovial giant cell tumor that mimicked a septic hip, reported by Patel et al. Interestingly, the patient in that case report had had 2 presentations of an acutely irritable hip 2.5 years apart and had undergone surgical irrigation during the first admission, but no masses were noted and the diagnosis of PVNS was made only after a second presentation when MRI and biopsy were performed. Tissue obtained via image-guided needle biopsy was characterized as “limited.” It was described as containing “fibroconnective skeletal muscle [sic] and synovial fragments rich in foamy macrophages.” No mention was made of any intralesional neutrophils. Based on the brief description of limited tissue, it is difficult for a reader to confirm the diagnosis as a bona fide PVNS as opposed to reactive synovium.
Tenosynovial giant cell tumor has recently been identified as a clonal neoplasm in which the neoplastic cells are characterized by a chromosomal rearrangement involving 1p21-p13. Translocation of the CSF1 gene at this locus leads to overexpression of a cytokine believed to recruit and stimulate the proliferation of bystander inflammatory cells. The inflammatory cells in tenosynovial giant cell tumor characteristically consist of histiocytes (tissue macrophages), multinucleated giant cells, and lymphocytes. It is thought that the receptor for CSF1 (CSF1R, a tyrosine kinase receptor) within the “inflammatory” component mediates the non-neoplastic cell response. In an animal model, CSF1R has been shown to modulate neutrophil chemotaxis.
We note that the tumor in the present case lacked a demonstrable chromosome 1 rearrangement. It is possible that a variant genetic alteration affecting CSF1/CSF1R or other unique factors intrinsic to the tumor contributed to neutrophil recruitment. Of particular note, the tumor in the present case showed areas resembling early coagulative necrosis (infarction), which may also have played a role in neutrophil chemotaxis. Furthermore, the tumor lacked demonstrable pyogenic organisms. Thus, the constellation of features supports the possibility that factors intrinsic to the tumor stimulated the neutrophil recruitment and contributed to the fever, acute pain, and other clinical features of a septic hip.
Our findings serve to expand the clinical and histologic spectrum of tenosynovial giant cell tumor. It remains unclear to us whether a neutrophilic infiltrate within the tenosynovial giant cell tumor represents a truly rare or perhaps an underreported occurrence. It is possible that previous cases similar to the present one have been interpreted clinically and histologically as septic synovitis. In any case, we propose that a tenosynovial giant cell tumor should be included in the differential diagnosis when an intra-articular mass is identified in the setting of acute joint pain and fever. An increased neutrophil count in joint fluid may sometimes reflect a “sterile” tumor-associated reaction, although we must recommend caution when considering this clinically. Pathologists encountering neutrophilic inflammation within proliferative synovium otherwise classic for tenosynovial giant cell tumor need not implicate infection or superinfection if that is not supported by microbiologic studies. Furthermore, if a localized mixed cellular inflammatory process is identified in a joint sample, it is important not to overlook tenosynovial giant cell tumor as a diagnostic consideration altogether if the appropriate imaging findings are also present.
Reference: Saadat E, Vargas SO, Anderson M, Glotzbecker M. Pediatric intra-articular localized tenosynovial giant cell tumor presenting as an acutely irritable hip: A case report. JBJS Case Connect. 2016 Jul 27;6(3):e60.
What is the diagnosis?
Venous malformation
Localized tenosynovial giant cell tumor
Synovial chondromatosis
Focal reactive synovitis
Infection


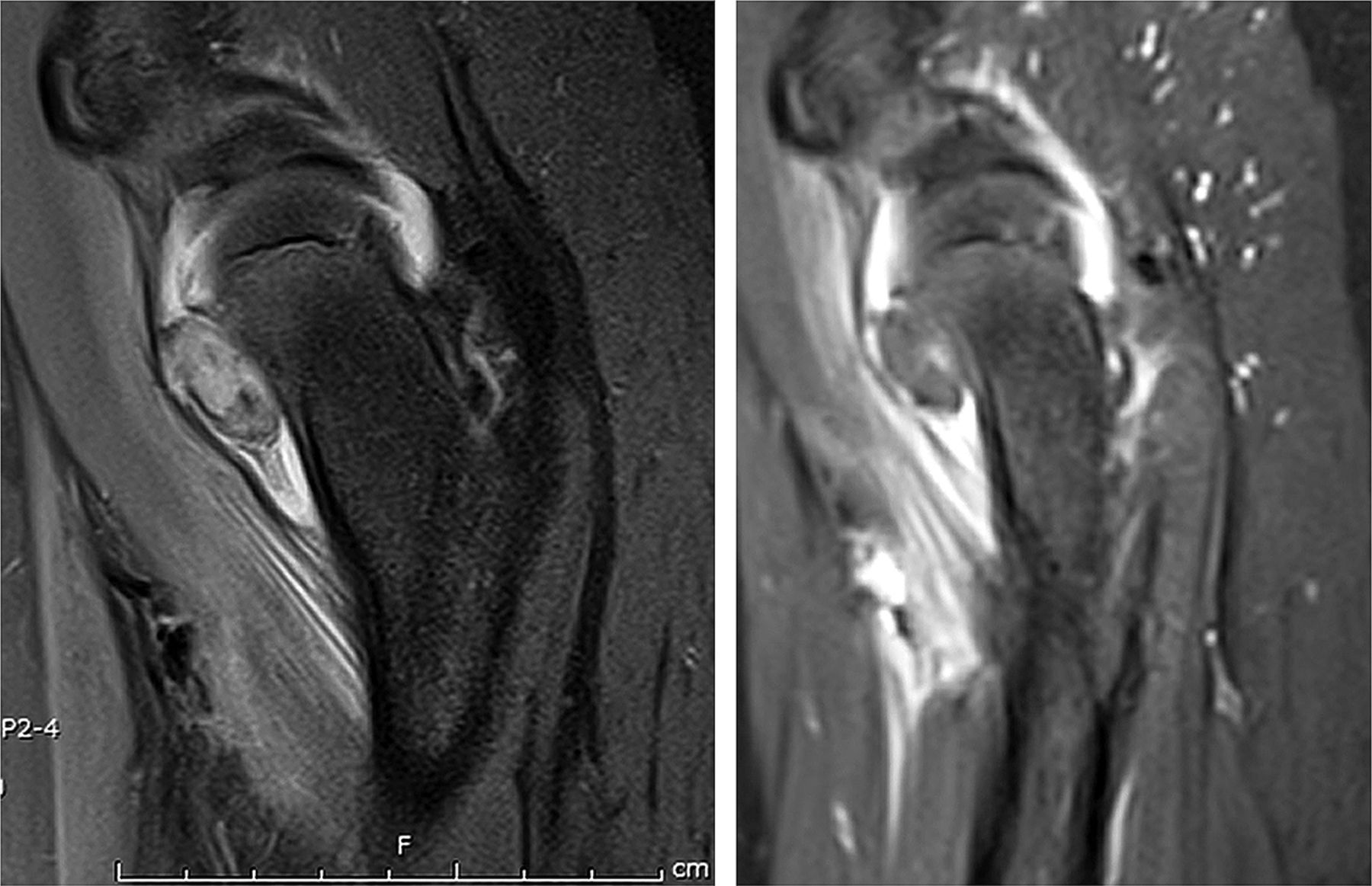
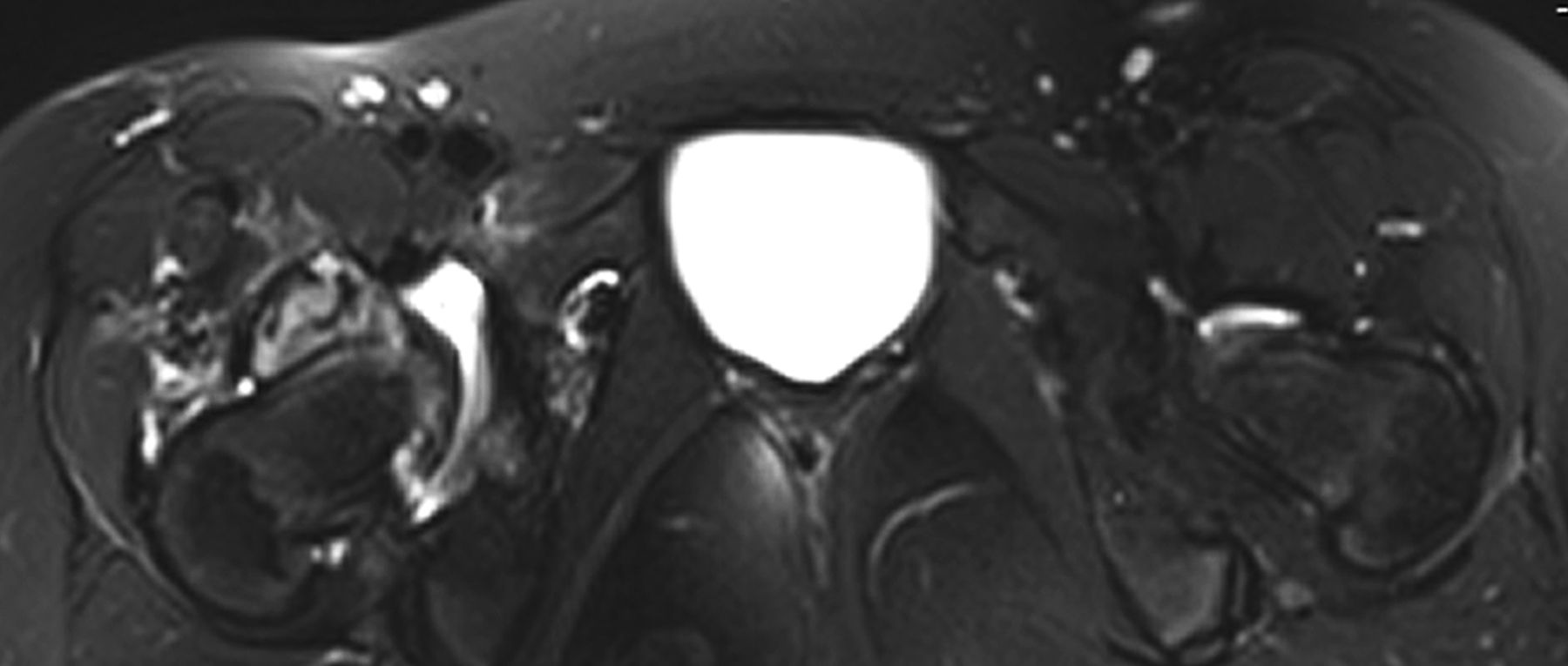

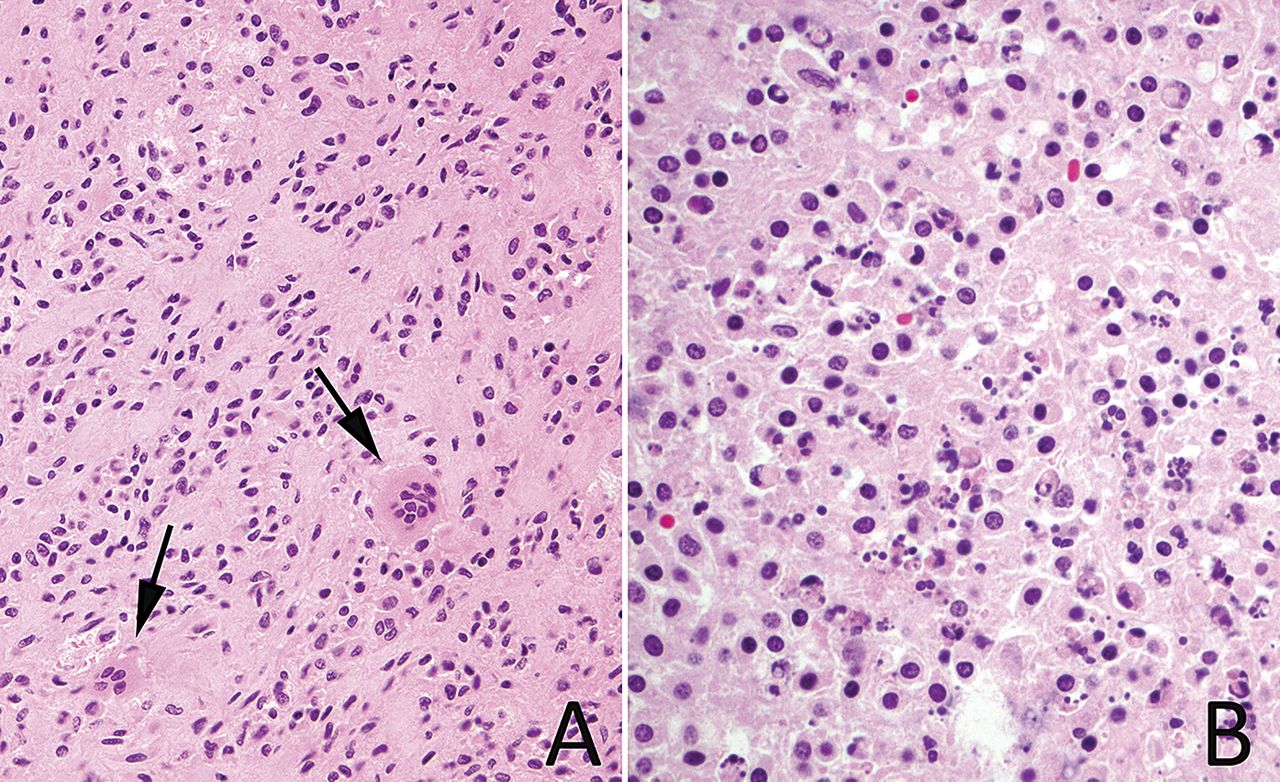
 Fig. 1
Fig. 1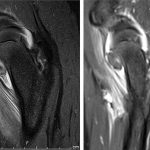 Fig. 2
Fig. 2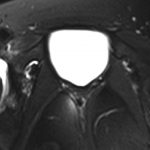 Fig. 3
Fig. 3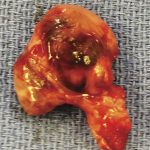 Fig. 4
Fig. 4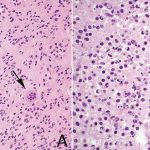 Fig. 5
Fig. 5