A 19-Year-Old Man with Increasing Shoulder Pain
February 20, 2019
A 19-year-old man had been diagnosed clinically with Kniest dysplasia shortly after birth, and subsequently underwent confirmatory genetic testing as a young adult. DNA sequencing revealed a heterozygous c.905C>T transition in exon 14 of COL2A1 (collagen, type II, alpha 1), which converts a codon for alanine (GCG) to a codon for valine (GTG). This mutation has been previously identified in at least 2 other individuals with Kniest dysplasia.
The patient presented for evaluation of his left shoulder after a chest radiograph for an upper respiratory infection identified a lesion in the proximal aspect of the left humerus. When asked, he admitted to a month-long mild increase in baseline shoulder pain. The surgical history included multiple procedures to correct bilateral lower-extremity valgus deformities and planovalgus foot deformities. The patient was ambulatory but utilized a wheelchair for long-distance mobility. Apart from the increased left shoulder pain, he had chronic, yet stable, right shoulder, hip, and knee pain.
Upon presentation, radiographs of the left shoulder demonstrated an osteoid-producing lesion in the proximal humeral metaphysis, with diaphyseal extension and a periosteal reaction (Fig. 1). Subsequent magnetic resonance imaging (MRI) demonstrated a heterogeneously enhancing lesion with an associated soft-tissue lesion (Fig. 2).
An incisional bone biopsy showed an aggressive lesion. Staging studies included computed tomography (CT) of the chest, whole-body positron emission tomography (PET), and a bone scan, which demonstrated no evidence of metastatic disease. The patient subsequently underwent neoadjuvant chemotherapy, followed by wide resection of the proximal aspect of the left humerus and a cemented endoprosthetic reconstruction (Fig. 3). Surgical pathology is shown in Figures 4-A and 4-B.
The combination of radiographic findings and histology is diagnostic of an incidentally detected, osteoblastic and chondroblastic osteosarcoma in this patient with Kniest dysplasia. There is no known increase in osteosarcoma oncogenic risk associated with Kniest dysplasia, and, to our knowledge, no literature exists associating these 2 conditions.
The patient completed an additional 19 weeks of adjuvant chemotherapy. Routine long-term surveillance has demonstrated no evidence of local recurrence or metastatic disease. The endoprosthesis remains stable. At the most recent examination at 16 months following surgery, he had continued to gain strength in the left upper extremity.
Proceed to Discussion >>Reference: : Tetreault A, Ramalingam W, Black J, Miller NH, Donaldson N. Osteosarcoma in an adolescent with Kniest dysplasia: a case report. JBJS Case Connect. 2018 Oct-Dec;8(4):e78.
To our knowledge, this is the first reported case of osteosarcoma occurring in a patient with Kniest dysplasia. There has been a single reported case of a grade-I sphenoethmoidal chondrosarcoma in a pediatric patient with Kniest dysplasia. While somatic COL2A1 mutations have been identified in chondrosarcomas, there is no known predisposition to chondrosarcoma in patients with Kniest dysplasia or other type-II collagenopathies. There have been no other associations between Kniest dysplasia and tumorigenesis.
In general, cases of bone or cartilage-forming malignancies in patients with osteochondrodysplasias are rare. The majority of reported cases describe osteosarcoma in patients with osteogenesis imperfecta (OI), a skeletal dysplasia that results from abnormal type-I collagen. Yet, there are a total of only 10 reported cases of osteosarcoma in the setting of OI that have been published in the English-language literature, with the generally accepted conclusion that development of malignancy is sporadic. Aside from OI and osteosarcoma, there are few cases of malignancy in patients with chondrodystrophies. A single report of chondrosarcoma in a patient with OI was published in 2013. Additionally, spondyloepiphyseal dysplasia tarda, another osteochondrodysplasia arising from a COL2A1 mutation with a phenotype similar to Kniest dysplasia, has a single report of osteosarcoma.
This case report raises the question as to whether osteosarcoma in a patient with Kniest dysplasia represents an isolated event, or if there is any biologic explanation for the development of a malignancy that can be attributed to the underlying COL2A1 genetic mutation. Known inherited risk factors for osteosarcoma include aberrations in the tumor suppressor genes p53 and RB1 (as in Li-Fraumeni syndrome and hereditary retinoblastoma, respectively) or in DNA helicases (as demonstrated in Bloom syndrome, Rothmund-Thomson syndrome, and Werner syndrome). Our patient’s genetic testing did not reveal any germline mutations that would predispose him to malignancy.
Whether there is a true increased risk of malignancy in patients with osteochondrodysplasias is yet to be determined. Nevertheless, early diagnosis of malignancy is crucial, as this has a strong impact on prognosis. Whereas long-term survival rates are as high as 60% to 78% with localized osteosarcoma, this declines substantially to 20% to 30% in the presence of clinically detectable metastases. Establishing an early diagnosis in cases of malignancy demands a high level of suspicion for new musculoskeletal symptoms in individuals. The most common presenting characteristic of osteosarcoma is intermittent pain, often related to increased activity but not necessarily present at night. A preexisting skeletal disorder may cloud this clinical picture. In patients with skeletal dysplasias, these symptoms may be masked by chronic pain, as was potentially the case with our patient. A change in the pattern or quality of pain may help differentiate chronic pain from that associated with tumor development. Additionally, when baseline activity level is decreased, as is common in individuals with skeletal dysplasia, the potential for exacerbating activity-related pain is limited.
On radiographs, a pathologic lesion may be more difficult to identify in the setting of abnormal bone development. This is especially true in the setting of OI because hyperplastic callus formation and associated symptoms following a fracture can mimic those of osteosarcoma and cause a delay in diagnosis. There have been reports of patients with Kniest dysplasia who have undergone successful total hip arthroplasty and mandibular distraction surgery without bone-healing issues. While this indicates the potential for adequate bone healing and remodeling, there are no reported cases of fractures or fracture-healing characteristics in the setting of Kniest dysplasia. Therefore, clinical suspicion of malignancy in these patients must remain high when there is any change in musculoskeletal symptoms, and appropriate radiographic and histologic analysis is necessary.
Additional study is warranted to address the possible risk of malignancy in patients with Kniest dysplasia and other hereditary osteochondrodysplasias. Patient and tumor genetic testing in any future cases will play a crucial role in elucidating this relationship.
Reference: : Tetreault A, Ramalingam W, Black J, Miller NH, Donaldson N. Osteosarcoma in an adolescent with Kniest dysplasia: a case report. JBJS Case Connect. 2018 Oct-Dec;8(4):e78.
What is the diagnosis?
Incidentally detected osteosarcoma in a patient with Kniest dysplasia
Incidentally detected chondrosarcoma in a patient with Kniest dysplasia
De-differentiated chondrosarcoma
Parosteal osteosarcoma
Remote bone infarct with endochondral bone formation

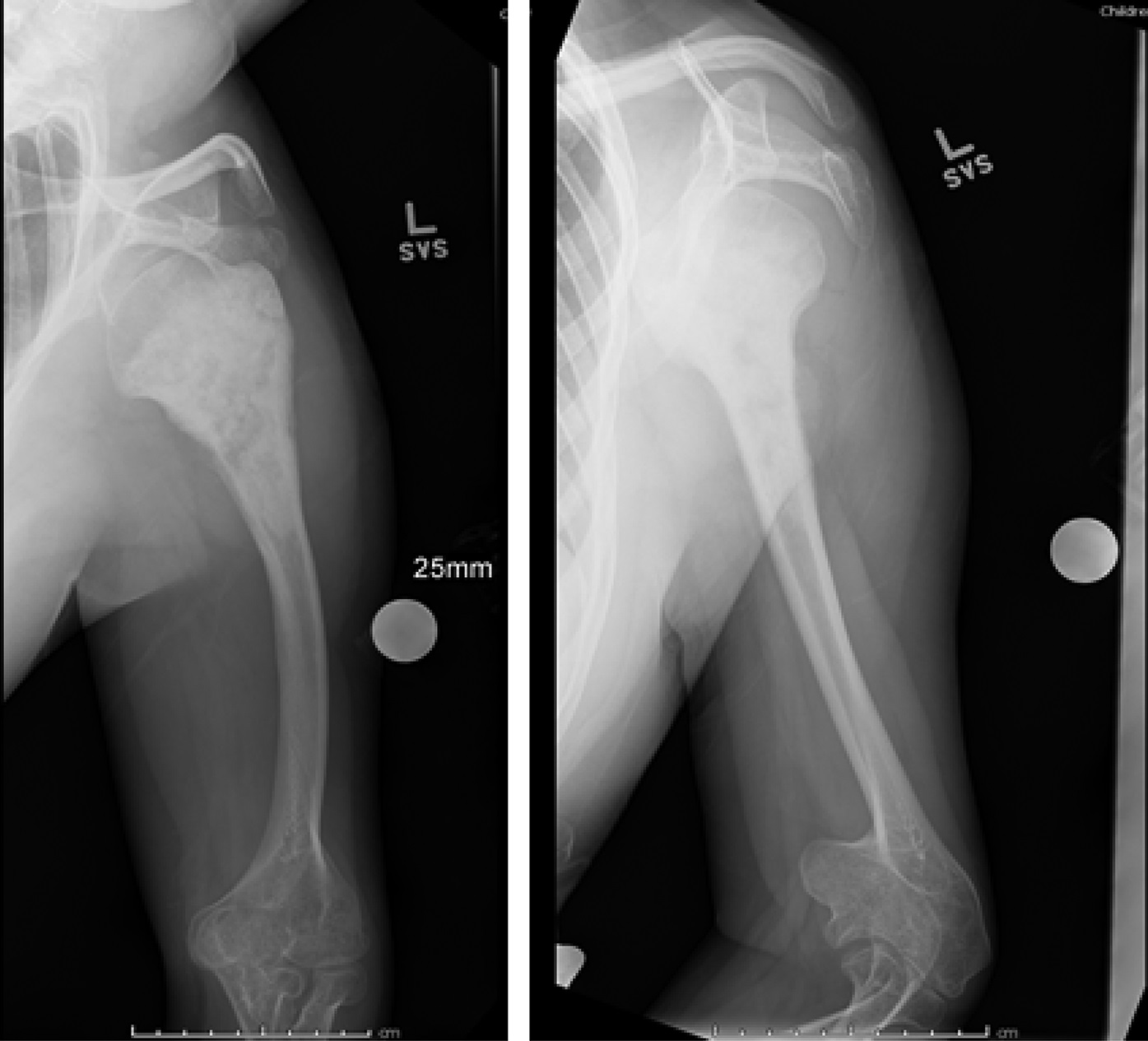
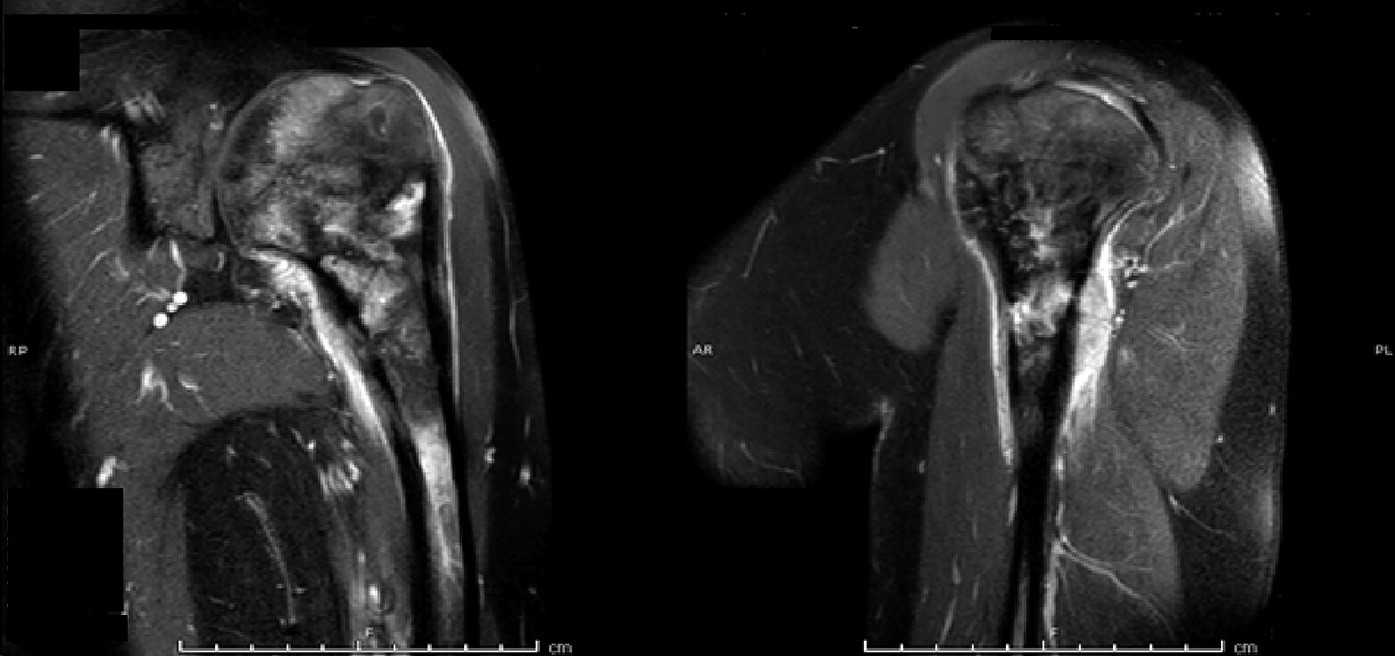

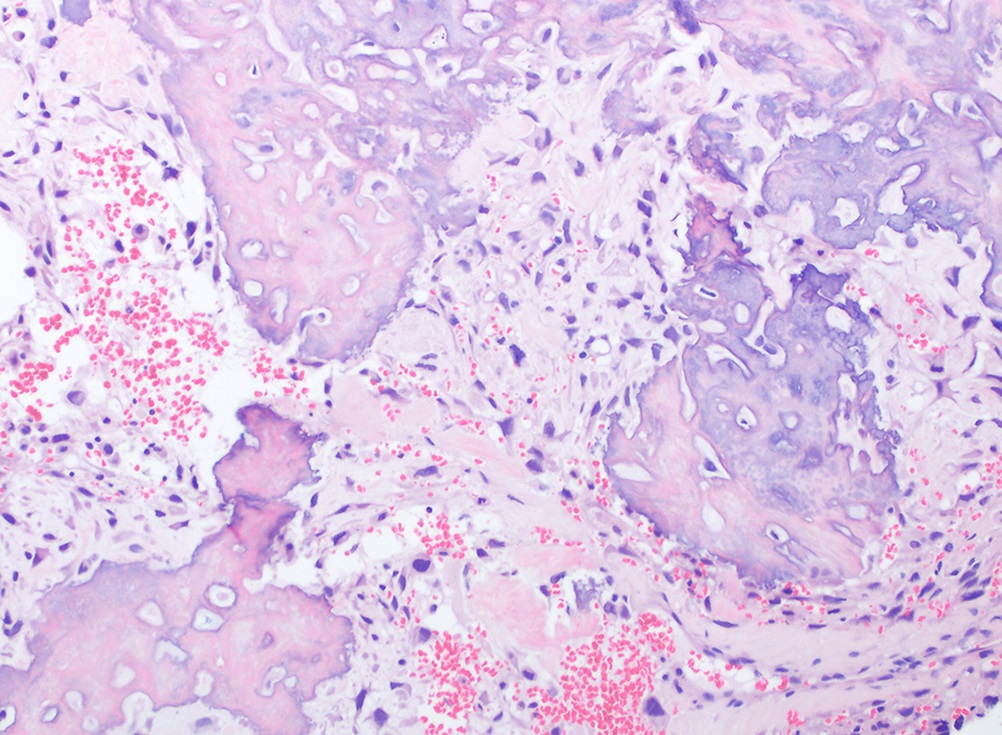
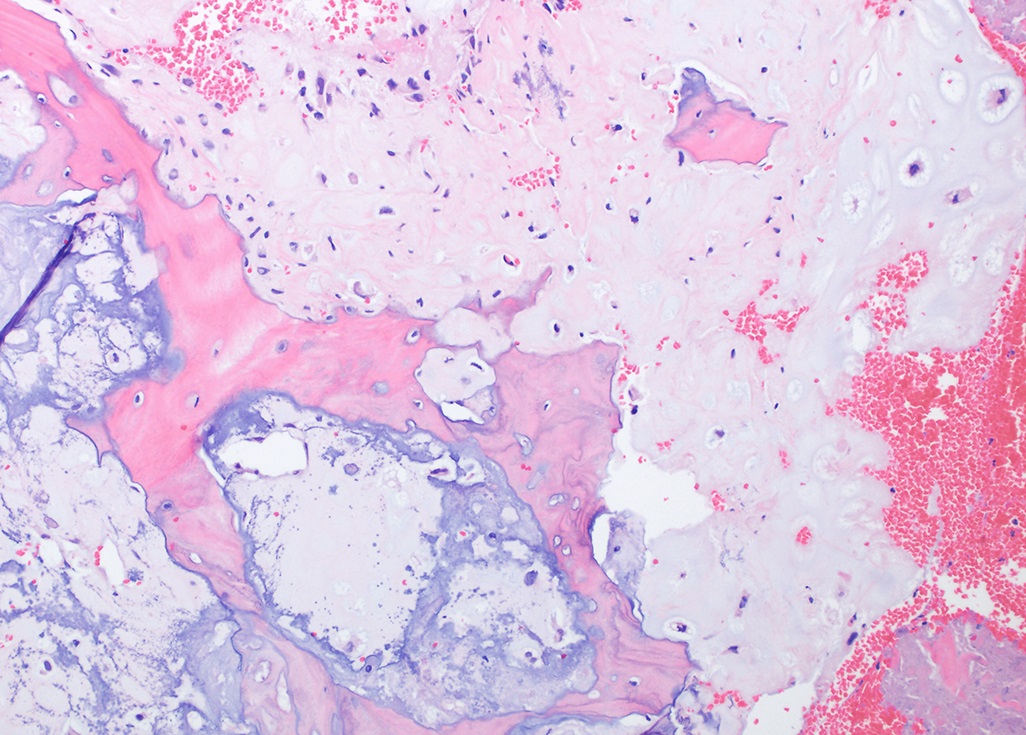
 Fig. 1
Fig. 1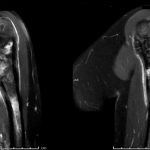 Fig. 2
Fig. 2 Fig. 3
Fig. 3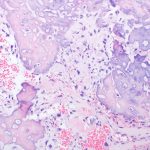 Fig. 4-A
Fig. 4-A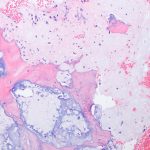 Fig 4-B
Fig 4-B