A 47-Year-Old Man with Worsening Thigh Pain and Fever
April 3, 2019
A forty-seven-year-old man presented to the emergency department with a two-month history of progressively worsening left thigh pain and three weeks of subjective fever. The patient had previously been seen for the leg pain by an outside physician two weeks after the onset of the pain, and at that time was diagnosed with sciatica. The patient’s medical history was pertinent for hereditary hemorrhagic telangiectasia (HHT) complicated by pulmonary arteriovenous malformations (AVMs) that had been successfully treated with angiographic coiling ten years prior to presentation. On physical examination, he was febrile and tachycardic and had severe tenderness to palpation overlying the lateral aspect of the left thigh. Laboratory testing revealed an elevated WBC (white blood-cell) count of 11,000/μL with 86% PMNs (polymorphonuclear leukocytes), an ESR (erythrocyte sedimentation rate) of 79 mm/hr, and a CRP (C-reactive protein) level of 19 mg/dL. Initial radiographs of the left femur (Figs. 1-A and 1-B) demonstrated periosteal reaction and mottled lucency, and subsequent MRI (magnetic resonance imaging) of the left thigh (Fig. 2) demonstrated altered marrow signal and enhancement involving nearly the entire left femur. An interventional radiologist attempted a percutaneous biopsy of the associated soft-tissue lesion, which proved inconclusive.
The patient was diagnosed with osteomyelitis and was subsequently taken to the operating room for irrigation, debridement, and open biopsy of the left thigh that revealed multiple abscesses along the periosteal surface of the femoral diaphysis as well as purulence within the medullary canal. The patient returned to the operating room for three additional debridement procedures. During the final irrigation, the medullary canal was reamed and antibiotic beads containing vancomycin and tobramycin were placed about the femur. Multiple culture samples were obtained during the operative course but failed to isolate any organisms. The patient was made non-weight-bearing on the involved leg and was discharged on empiric intravenous cefazolin and oral minocycline antibiotic therapy after consultation with the infectious disease service.
Four weeks after the final debridement procedure, the patient again presented to the emergency department after the sudden onset of severe left thigh pain that had developed as he was exiting his car. He had not been bearing weight during the episode. Radiographs (Fig. 3) revealed a minimally displaced fracture in the proximal third of the femur, at a location discrete from the cortical window made for his previous debridements. He underwent operative irrigation and debridement of the fracture site and placement of a locked cephalomedullary device coated with tobramycin and vancomycin antibiotic cement. Along with routine cultures, a tissue sample was also sent to an outside institution for PCR (polymerase chain reaction) analysis for culture-negative organisms.
PCR analysis, which utilized a 16S rRNA (ribosomal RNA) gene primer set and reverse transcription-PCR, revealed Fusobacterium nucleatum DNA in the tissue sample. In consultation with the infectious disease service, the antibiotic regimen was therefore changed to oral metronidazole. At the six-month follow-up after the initial presentation to the emergency department, the patient had pain-free toe-touch weight-bearing of the involved leg, a mildly antalgic gait on examination, inflammatory markers within the normal range, and radiographic (Figs. 4-A and 4-B) and CT (computed tomography) imaging consistent with a well-healing proximal femoral fracture with abundant callus. The patient was advanced to full weight-bearing at this time. In addition, the antibiotics were transitioned to amoxicillin-clavulanate, to be continued indefinitely, because of his gastrointestinal complaints while on metronidazole. At the one-year follow-up, the patient remained pain-free with full weight-bearing, had normal inflammatory markers, and had radiographic (Figs. 5-A and 5-B) and CT imaging consistent with continued healing of the proximal femoral fracture with maturing callus, stable hardware placement, and no evidence of recurrent osteomyelitis. The patient did report a small leg-length discrepancy, and he was noted clinically on physical examination to have a 1-cm increase in the length of the left leg compared with the right. This discrepancy was treated to the patient’s satisfaction with a shoe-lift orthotic.
Proceed to Discussion >>Reference: Foran I, Kinney MC, Botte MJ, Covey DC. Fusobacterium nucleatum osteomyelitis of the femur in a patient with hereditary hemorrhagic telangiectasia: A case report. JBJS Case Connect. 2016 Jan-Mar;6(1):e11.
The pathogenesis of extracerebral infection in HHT is poorly understood. Both immunologic and mechanical factors likely play a role in the hematogenous seeding of infection. Cirulli et al. provide evidence that neutrophils and monocytes in patients with HHT exhibit a reduced oxidative burst, inhibiting their killing capacity—thus predisposing to infection. Additionally, because of the high prevalence of epistaxis in patients with HHT (as high as 95% according to one study), manipulation of the nasal mucosa has been hypothesized to be a potential entry route for bacteria into the bloodstream, resulting in increased frequency of transient bacteremia and subsequent seeding of bone and other end organs. Finally, the presence of altered vascular connections in these patients may allow bacteria to bypass capillaries, which normally serve as immunologic filters to pathogenic organisms. Because patients with HHT possess arteriovenous connections, bacteria may therefore be able to directly seed bone and other end organs, resulting in the increased rate of infection seen in HHT.
Staphylococcus aureus is overwhelmingly the most commonly reported organism in HHT-related orthopaedic infections. A review of the literature revealed only a single case of a nonstaphylococcal infection involving an articular space or bone in a patient with HHT—spondylodiscitis in a sixty-five-year-old man secondary to Streptococcus mutans. To our knowledge, the present case represents the first report of F. nucleatum causing osteomyelitis in HHT, although it has been reported to be the pathogenic organism in brain abscesses in these patients.
Fusobacterium species are gram-negative bacilli that are part of the normal flora in the oral cavity and female genital tract, as well as in the distal part of the gastrointestinal tract. Although F. nucleatum is part of the normal flora, there is increasing evidence that it is involved in several pathologic entities. There is a well-known association between F. nucleatum and periodontal infections including adenoiditis, where abscess formation is common. F. nucleatum has also been linked more recently to colorectal carcinoma and preterm births. A review of the present patient’s medical record revealed that he had undergone a routine screening colonoscopy several weeks prior to onset of his symptoms. Thus, along with hematogenous spread associated with manipulation of nasal mucosa as described above, an additional explanation for the patient’s unusual presentation is development of F. nucleatum bacteremia secondary to his colonoscopy, with subsequent seeding of the femur. Although infection of bone secondary to Fusobacterium species is rare, there are reports describing hematogenous osteomyelitis due to F. nucleatum in the vertebrae, pelvis, and long bones. In one series, targeted antibiotic regimens were universally successful in resolving the infection in these patients, although surgical debridement is a necessary adjunctive intervention because of the tendency for abscess formation associated with Fusobacterium osteomyelitis.
Orthopaedic surgeons, emergency room physicians, and radiologists should be aware of the increased risk for osteomyelitis in patients with HHT who may have no other risk factors for infection. Early imaging of the region of concern is essential to diagnosis. PCR can be helpful to identify rare organisms that will not grow in normal culture media and tailor antibiotics to them.
Reference: Foran I, Kinney MC, Botte MJ, Covey DC. Fusobacterium nucleatum osteomyelitis of the femur in a patient with hereditary hemorrhagic telangiectasia: A case report. JBJS Case Connect. 2016 Jan-Mar;6(1):e11.
What is the diagnosis?
Vascular malformation
Metastatic carcinoma
Osteosarcoma
Malignant lymphoma
Osteomyelitis


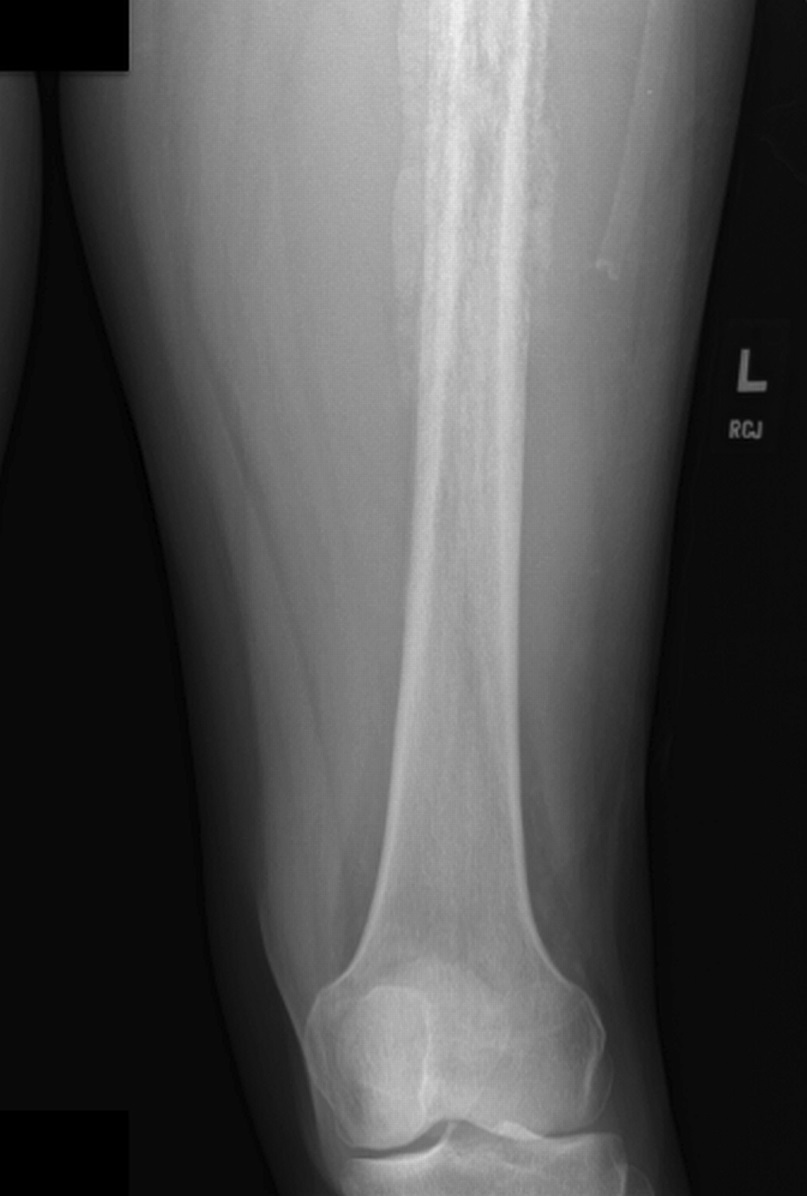
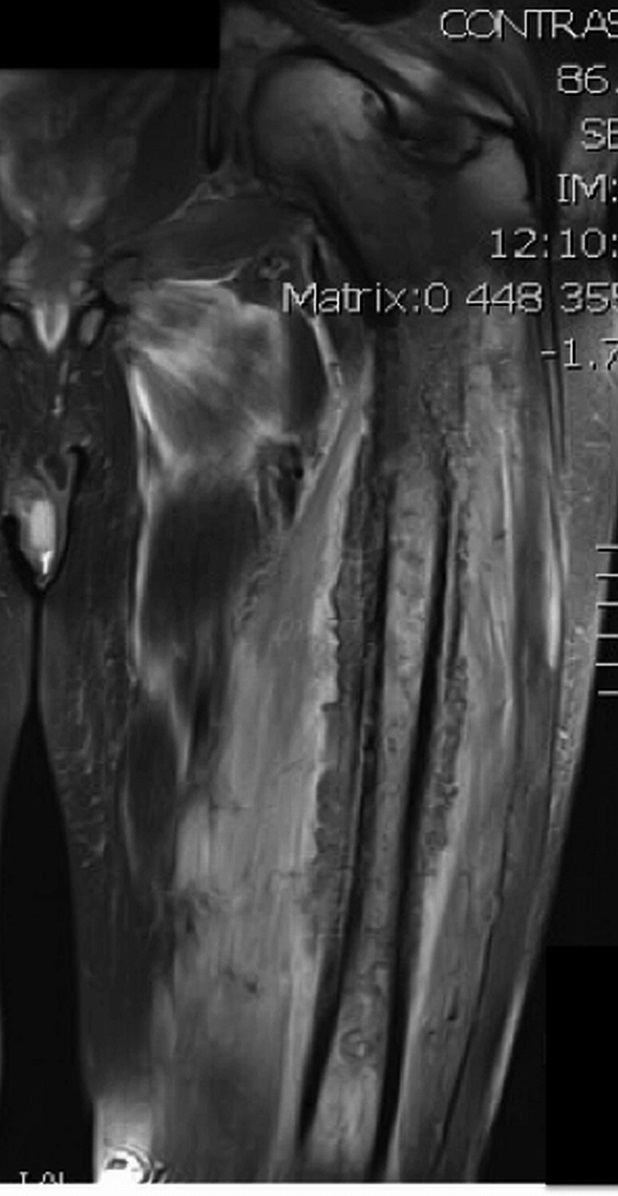
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B



