A healthy, 27-year-old, right-hand dominant man presented with progressive pain of the right forearm. The symptoms had started 3 years ago after a minor traumatic injury to the right arm. The pain initially was intermittent but became persistent over time. The patient rated it as 3 of 10 on a visual analog scale (VAS). Pronation and supination exacerbated the symptoms. He did not report pain at night or the need for analgesics. He had no noteworthy medical, surgical, social, or family history. Initial treatment provided by his primary care physician consisted of steroid trigger-point injections for a supposed muscle strain, with limited relief. The patient moved to a new state and was referred to the orthopaedic hand service by his new care provider.
On physical examination, there was a prominence without discoloration on the radial side of the right midforearm; there was no tenderness on palpation. There were no signs of muscle atrophy or weakness. There were no palpable lymphadenopathies in the epitrochlear or axillary areas. Motor and sensory function of the ulnar, radial, and median nerves was intact. The radial and ulnar pulses were both palpable. Range of motion of the elbow included 0° of extension to 130° of flexion, 70° of supination, and 80° of pronation. The abbreviated version of the Disabilities of the Arm, Shoulder and Hand (QuickDASH) score, which was obtained as part of standard clinical practice, was 15.9.
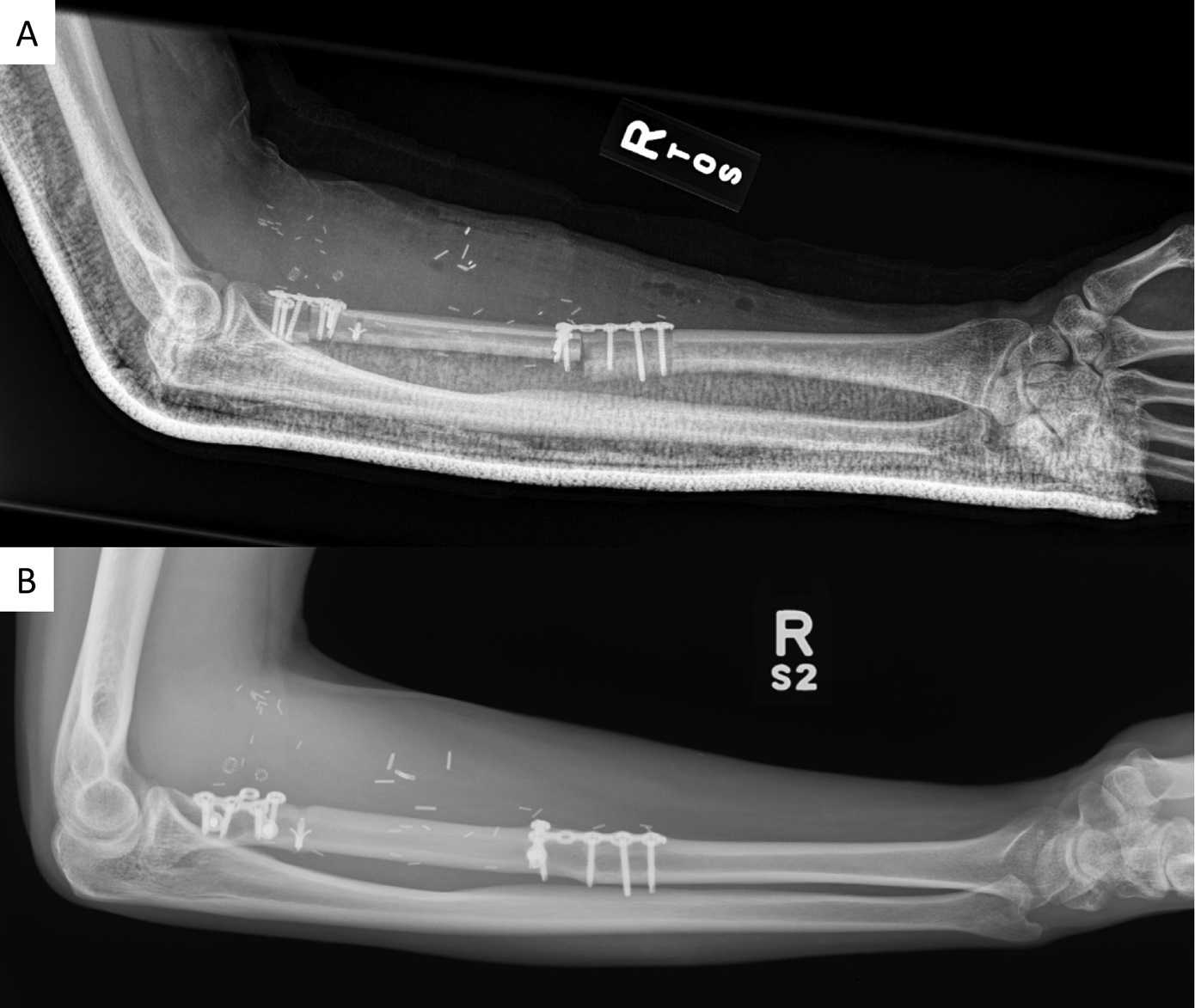
Conventional radiographs (anteroposterior and lateral views) and magnetic resonance imaging (MRI) with and without intravenous contrast of the right forearm were acquired. The radiographs showed an aneurysmal-like lesion that was lytic and had multiple thick septations with a well-defined geographic boundary in the proximal third of the radius (Fig. 1). There was no pathologic fracture. MRI showed an expansile osseous lesion (3.7 × 3.0 × 8.4 cm) with lobulated margins without extraosseous extension; there was no neurovascular invasion. The lesion was hypointense on the T1-weighted sequences and had a heterogeneous hyperintense signal on the T2-weighted sequences. There was no evidence of fluid-fluid levels. Distribution of the contrast was heterogeneous on the T1-weighted fat-suppressed sequences after gadolinium injection (Fig. 2).
A computed tomography (CT)-guided core biopsy of the lesion was performed preoperatively for histologic diagnosis. Microscopically, the sections showed a fibrous to fibro-osseous lesion composed of fibroblast-like cells arranged in a fascicular to storiform pattern with varying degrees of hypercellularity (Fig. 3). Many areas showed mixed fibrous and osseous components with woven bone formation that lacked surrounding osteoblasts. Within the fibrous areas with abundant collagen deposition, there was expansile growth by the fibroblastic component. There were hypercellular spindle-shaped nuclei showing plumper cells with less surrounding collagen deposition and an intermixture of osteoclast-type giant cells. No cytologic atypia was observed. There were only rare mitotic figures, and scattered apoptotic cells were identified. Immunohistochemical profiling showed tumor cells that were negative for MDM2 and CDK4. Additionally, the fluorescence in situ hybridization (FISH) and next-generation DNA sequencing failed to show MDM2 amplification or other targeted mutations.
The diagnosis of desmoplastic fibroma of the proximal aspect of the radius was made (Link to the digital whole-slide image: desmoplastic fibroma), and surgery was elected.
We performed a wide margin resection with intraoperative frozen sections to confirm negative margins. The radial head was preserved, and an 8.5-cm defect remained. Because of the size of the defect, a vascularized fibular autograft reconstruction was selected, anastomosing the peroneal artery to a proximal branch of the radial artery. We felt that use of a vascularized graft would increase the chances of healing at both junctions compared with a nonvascularized graft. The bone graft was fixed proximally with a web plate and distally with a T-plate (Zimmer Biomet). The biceps tendon was reinserted into the fibula with use of suture anchors (Mitek Quickanchor GII; DePuy Synthes) (Fig. 4). The bowing of the radius was sacrificed due to the intercalary nature of the reconstruction. However, to ensure that rotation was restored, the bicipital reinsertion to the fibula was ulnar and the radial styloid was lateral on anteroposterior views during intraoperative fluoroscopy. All of the margins were negative for tumor cells.
No postoperative peroneal palsy or ankle instability was noted, nor were there any complications at the level of the forearm or the donor site. After nearly 1 year, the postoperative QuickDASH score was 13.6; after 2 years, the score had decreased to 2.7. The Patient-Reported Outcomes Measurement Information System (PROMIS) Upper Extremity and Physical Function Short Form T-score was 42 (50 is the average for the U.S. general population). After 24 months of follow-up, there had been no recurrence; there was integration of the fibular bone graft with elbow flexion of 135° and extension of 0°, along with forearm pronation of 70° and supination of 60° (Fig. 5). Other than forearm supination, all motions had improved or had remained the same compared with preoperative motion. Additionally, at the distal graft-radius junction, fixation screws were palpable under the extensor muscles, but this was not the cause of the restricted supination. The patient continues clinical and radiographic follow-up on an annual basis.
Proceed to Discussion >>Reference: Lans J, Chebib IA, Castelein RM, Chen NC, Lozano-Calderón S. Reconstruction of the proximal aspect of the radius after desmoplastic fibroma resection: a case report. JBJS Case Connect. 2019 Jan-Mar;9(1):e12.
We have described a patient at the typical age and with the typical symptoms of a desmoplastic fibroma of the proximal aspect of the radius. On conventional radiographs, the lesion had features of a lytic bone lesion. Typical features for a desmoplastic fibroma are cortical aneurysmal expansion, thick pseudotrabeculation, and a narrow zone of transition. There was no cortical breakthrough. To confirm the diagnosis, a CT-guided core biopsy was performed. This showed a fibro-osseous lesion with fibroblastic and collagen components, without cellular atypia. With knowledge of the aggressive local behavior of a desmoplastic fibroma and its high rate of recurrence, we planned a wide resection and confirmation of negative margins with intraoperative frozen sections.
Desmoplastic fibromas are benign, locally aggressive, collagen-producing tumors that were first described by Jaffe in 1958. They are extremely rare, with an estimated incidence of 2.5 patients per 100 million people per year. Approximately three-quarters of patients present within their first 3 decades of life, and there is no sex predilection. Patients usually present with a painful mass. The most common locations are the long bones and the mandible, where tumors typically arise from the metaphysis. The etiology is unknown, but a possible relationship between prior trauma and hormonal dependence has been proposed. Furthermore, an association with trisomy 8 and/or 20 has been described. Treatment options are intralesional curettage or resection; the latter is the preferred treatment method because of lower recurrence rates. Overall, recurrence rates of 15.4% to 72% have been reported. Evans et al. showed that soft-tissue invasion was associated with higher recurrence rates. When tumors are inoperable, radiation therapy can reduce pain and prevent tumor progression.
There have been 3 case reports in the literature documenting desmoplastic fibromas of the radial shaft. In these reports, the radial shaft defect was reconstructed with a vascularized fibular autograft (n = 1) or a nonvascularized fibular autograft (n = 2). The study by Giessler et al., written in German, described a 16-year-old patient who had undergone vascularized fibular autograft reconstruction of a large 11-cm defect of the radial shaft, and reported pronation and supination of 80° and 45°, respectively. The other 2 studies did not elaborately describe the patient outcomes after nonvascularized fibular autograft reconstruction. Therefore, the case reported herein adds to the English-language literature on desmoplastic fibroma by describing the presentation, diagnostics, treatment, and outcomes of a patient with a desmoplastic fibroma of the proximal aspect of the radius.
On conventional radiographs, desmoplastic fibromas appear as aneurysmal lytic bone lesions, similar to giant-cell tumors, aneurysmal bone cysts, solitary bone cysts, hemangiomas, fibrous dysplasia, nonossifying fibromas, and chondromyxoid fibromas. CT is preferred for evaluating the cortical breakthrough that is present in 23% to 29% of desmoplastic fibromas, and its presence should alert for a malignancy. MRI is used to assess soft-tissue extension, showing that most lesions are confined to the intramedullary space and the cortical bone. On T1-weighted images, lesions show low-to-intermediate intensities, and a heterogeneous hyperintense signal is seen on T2-weighted images. Because of the high fibrous composition of these tumors, T2-weighted images also may show areas of low intensity. These features are similar to extra-abdominal desmoid tumors. Intravenous contrast with gadolinium shows a nonhomogeneous signal distribution due to pseudotrabeculation, varying hypocellular zones, dense fibrous tissue, and collagen depositions.
Histopathologically, desmoplastic fibromas show slender fibroblastic to stellate cells in an abundant collagenous matrix. Mitotic figures are scarce and, rarely, there may be deposition of osteoid or chondroid matrix, especially with recurrent desmoplastic fibromas, making it difficult to distinguish them from fibrous dysplasia. There are no specific immunohistochemical markers for desmoplastic fibromas. There is histologic overlap between desmoplastic fibromas and desmoid-type fibromatosis with regard to histology and epidemiology; however, desmoplastic fibromas lack mutations in the adenomatous polyposis coli (APC)/β-catenin pathway. Additionally, desmoid tumors are more common in women. Another important histologic differential diagnosis is a low-grade fibrosarcoma of bone because it also shows collagen-rich matrix. Additionally, a low-grade central osteosarcoma with little cytologic atypia can be mistaken for a desmoplastic fibroma.
This case report describes a young man with a desmoplastic fibroma of the proximal aspect of the radius that was successfully treated with wide resection and vascularized fibular autograft reconstruction. This patient had good functional outcomes despite the restricted supination.
Reference: Lans J, Chebib IA, Castelein RM, Chen NC, Lozano-Calderón S. Reconstruction of the proximal aspect of the radius after desmoplastic fibroma resection: a case report. JBJS Case Connect. 2019 Jan-Mar;9(1):e12.
What is the diagnosis?
Fibrous dysplasia
Desmoplastic fibroma
Giant cell tumor
Chondroblastoma
Aneurysmal bone cyst

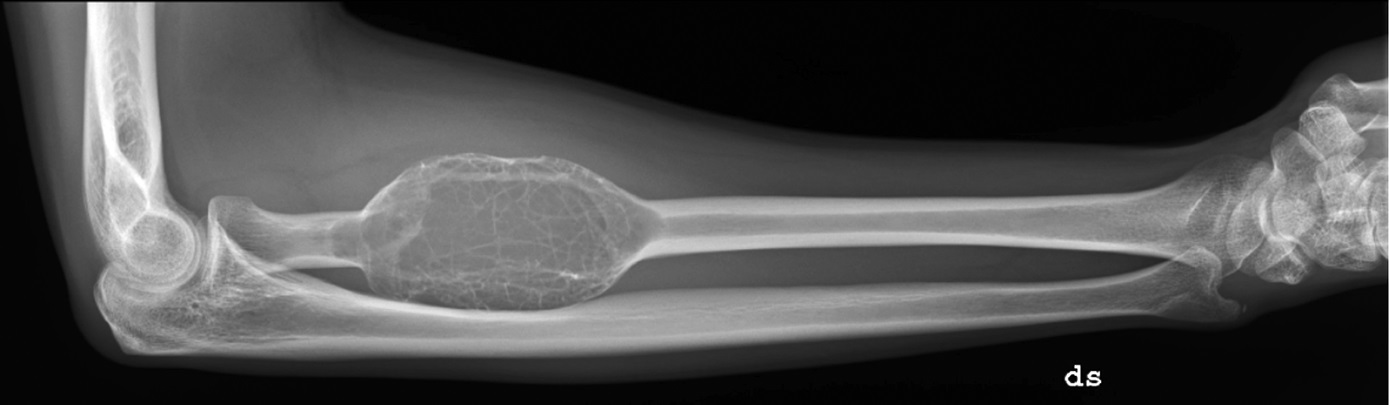
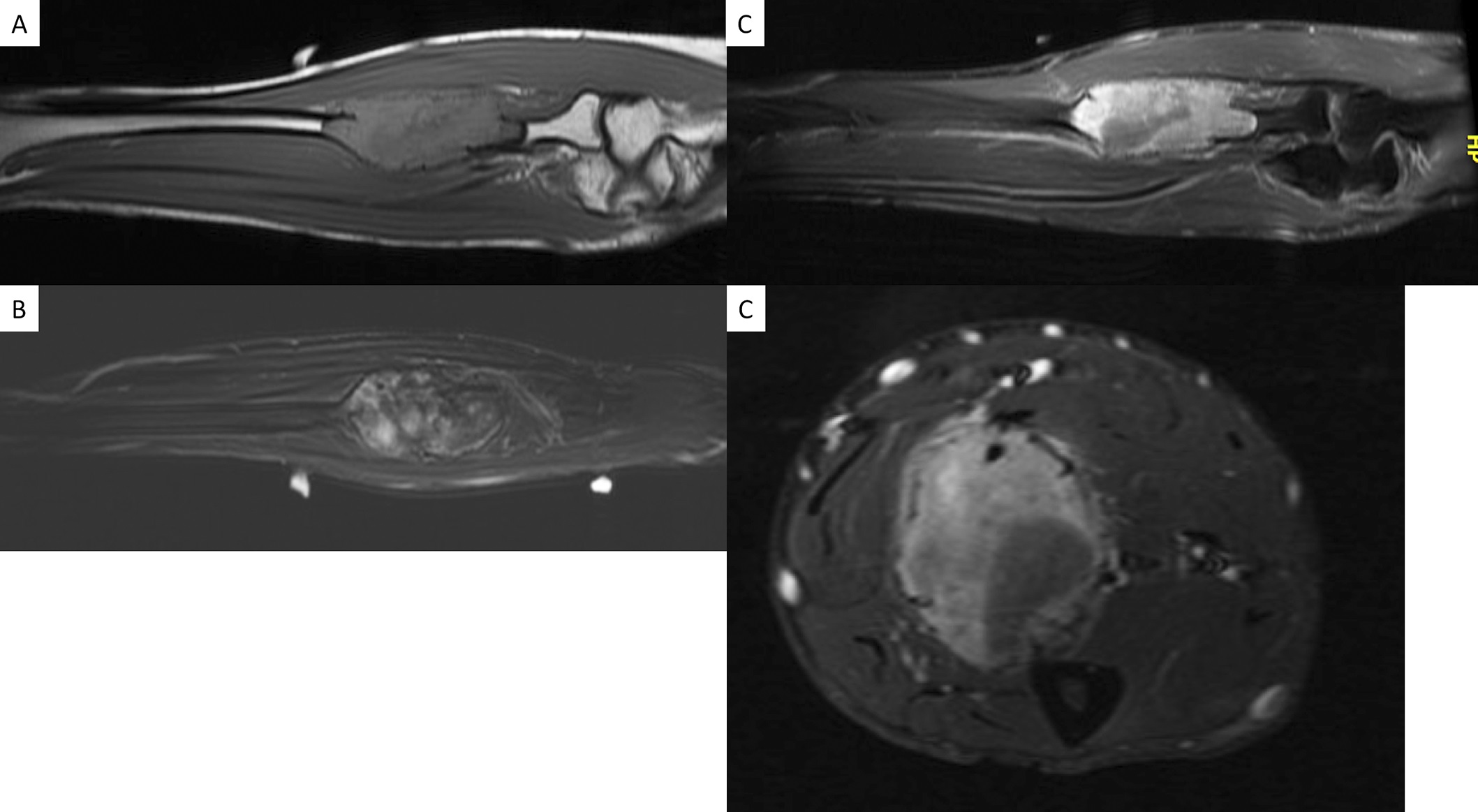
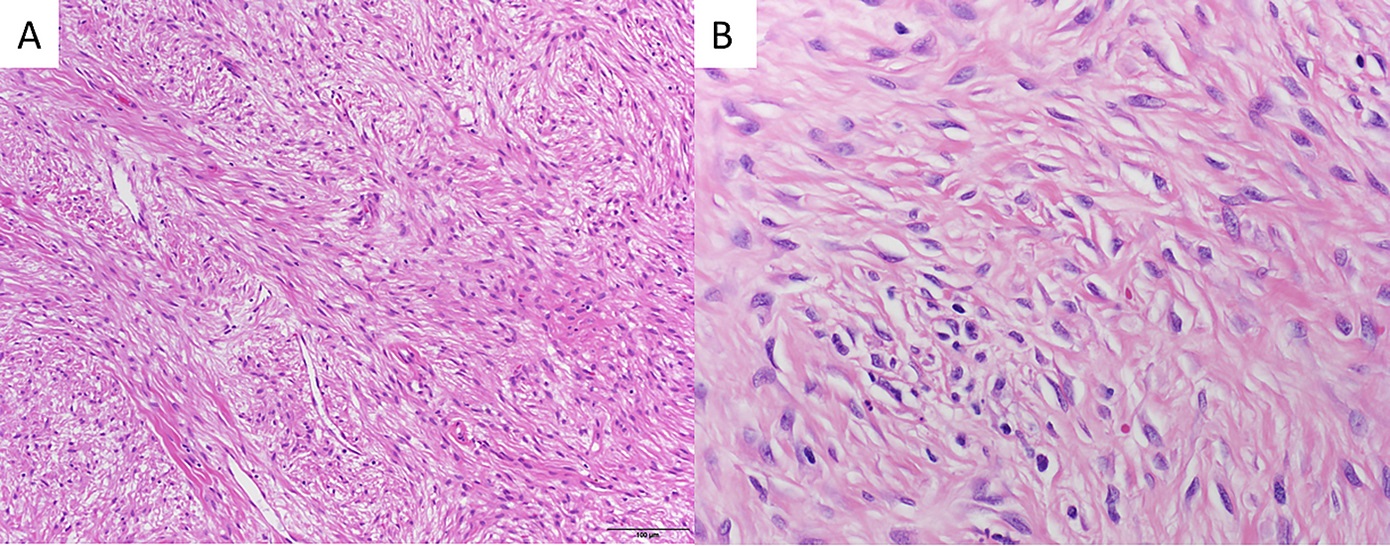
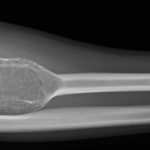 Fig. 1
Fig. 1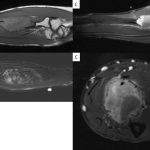 Fig. 2
Fig. 2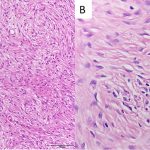 Fig. 3
Fig. 3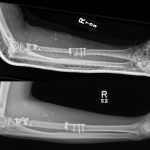 Fig. 4
Fig. 4 Fig. 5
Fig. 5