A Forty-eight-Year-Old Woman with Severe Persistent Knee Pain
August 1, 2012
A forty-eight-year-old woman was hospitalized twice (five months apart) for severe pain and limited range of motion in the right knee. Three years earlier, she had twisted the knee and had been treated nonoperatively, after which she had had no relief of symptoms and required crutches to walk. Physical examination revealed that the patient was obese (a body mass index of 35.2) and had limited range of motion of the right knee joint (from 20° to 80°). The skin over the painful area appeared normal. The patient limped on the right side with attempts at weight-bearing. Radiographs of the right knee joint showed mild osteoarthritic changes (Ahlbäck score of I). During arthroscopy of the right knee, a diagnosis was made of degenerative damage to the posterior horn of the medial meniscus, International Cartilage Repair Society grade-II or III cartilage changes in the bearing surface of the medial condyle of the femur, and a degenerative tear of the anterior cruciate ligament at its femoral insertion. Shaving and microfractures of the damaged surface of the medial condyle of the femur were performed, and the damaged portion of the medial meniscus was removed. Postoperatively, the patient did not experience an appreciable change in symptoms. The patient was evaluated again as a result of continued pain five months later. Palpation of the area of the tuberosity of the right tibia was difficult due to severe hyperesthesia. An ultrasound examination of the right knee showed a slightly increased volume of joint fluid. A region with dimensions of 23 × 10 × 20 mm was observed medial to the tibial tuberosity (Fig.1), and the ultrasound scan demonstrated multiple blood vessels in the surrounding area. An excisional biopsy was performed, which revealed a highly vascular 1.5 × 2-cm mass on the medial side of the tibial tuberosity. The mass was bluish in color, had the consistency of jelly, and had visible blood vessels traversing it (Fig. 2). Histopathologic examination of the mass was done (Fig. 3).
Immunohistochemical staining was performed with use of monoclonal antibodies to desmin and smooth muscle actin, and the results showed positivity for smooth muscle actin and desmin and negativity for chromogranin. All of these findings were consistent with a glomus tumor or glomangioma. Immediately after the surgical removal, the pain disappeared, and a few days later the patient was walking freely without crutches. At the time of the last follow-up visit, six months postoperatively, the patient reported continued relief of pain.
Proceed to Discussion >>Reference: Puchala M, Kruczynski J, Szukalski J, Lianeri M. Glomangioma as a rare cause of knee pain. A report of two cases. J Bone Joint Surg Am. 2008;90:2505-8. doi:10.2106/JBJS.G.01094
Glomus bodies are located in the reticular layer of the dermis and are composed of an afferent arteriole and an efferent venule with multiple anastomoses. The arterial end of the glomus body is surrounded by uniform glomus cells. Glomus tumors make up approximately 1% to 5% of all soft-tissue tumors. Two clinical presentations of these tumors can be identified: solitary and multiple. The etiology of a solitary glomus tumor is unknown, whereas the etiology of multiple glomus tumors is associated with an autosomal dominant heritable mutation in the glomulin gene, localized to chromosome 1p 21-22, which encodes the glomulin protein. Glomus tumor variants include glomangioma and glomangiomyoma. As much as 70% to 75% of these tumors involve the hand, and they present more frequently in women than in men. The majority of glomus tumors are found in the thirty to sixty-year-old age group. Glomus tumors have not been observed in individuals who are less than one year of age (glomus bodies form after that age) or in elderly persons (glomus bodies undergo atrophy and degeneration in elderly persons). The typical distribution of glomus bodies is to the distal parts of the phalanges and nail beds of the hand. Subungual glomus tumors are the easiest to identify, as they often exhibit a bluish discoloration that is <10 mm in diameter. The differential diagnosis includes melanoma, blue nevus, and angioma. Glomangiomas found deep in the subdermal tissue may not be visible or palpable. There have also been reports of atypical locations, including the stomach, lungs, trachea, bones, and intestines. There are three main clinical tests used to diagnose glomus tumors. The first is the Love pin test, in which the head of a pin or the end of a paper clip is pressed gently against the tender area to localize the pain. A positive test result is the patient’s experience of severe pain, occasionally accompanied by an involuntary withdrawal of the hand. This test was positive in our patient. The second, the Hildreth test, involves applying a tourniquet to the base of the suspected digit and repeating the Love pin test. A positive result is the lack of pain in the patient. The third test is exposure to cold, which should produce pain related to cold sensitivity; this test was negative in our patient. These tests have limited use, as they are not 100% specific. Furthermore, the Hildreth test can only be performed on the upper limbs. Other diagnostic tools available include magnetic resonance imaging (which is the most sensitive) and ultrasound. An ultrasound study does not yield conclusive evidence, and the examination itself is subjective and depends on the experience of the person conducting the test. Advantages of an ultrasound study include the speed with which the examination is conducted, the relatively easy access to the equipment, and low costs. The results of an ultrasound study were inconclusive, as the examination yielded only the picture of a well-vascularized change. Ultrasound examination of a patient with suspected glomus tumor is, however, useful for the purpose of building a differential diagnosis. Histopathological examination of the tissue is performed with use of hematoxylin-eosin stain, while the immunohistochemical study seeks to confirm the presence of tissue similar to smooth muscle cells. Combined, the two tests can confirm a diagnosis of glomus tumor. There are a small number of reported cases of glomus tumor localized to the knee joint, usually associated with a long-term clinical course. In our patient, the diagnosis was made more difficult not only by the atypical location of the tumor but also by coexisting degenerative changes and reports of trauma to the knee area, resulting in a focus on other pain etiologies, which obscured the clinical picture. The time between the start of symptoms until the removal of the tumor was three years. This case report illustrates the importance of including glomus tumor in the differential diagnosis of patients who present with pain of unknown cause, regardless of location.
Reference: Puchala M, Kruczynski J, Szukalski J, Lianeri M. Glomangioma as a rare cause of knee pain. A report of two cases. J Bone Joint Surg Am. 2008;90:2505-8. doi:10.2106/JBJS.G.01094
Hamartoma
Hemangiopericytoma
Hemangioma
Glomangioma

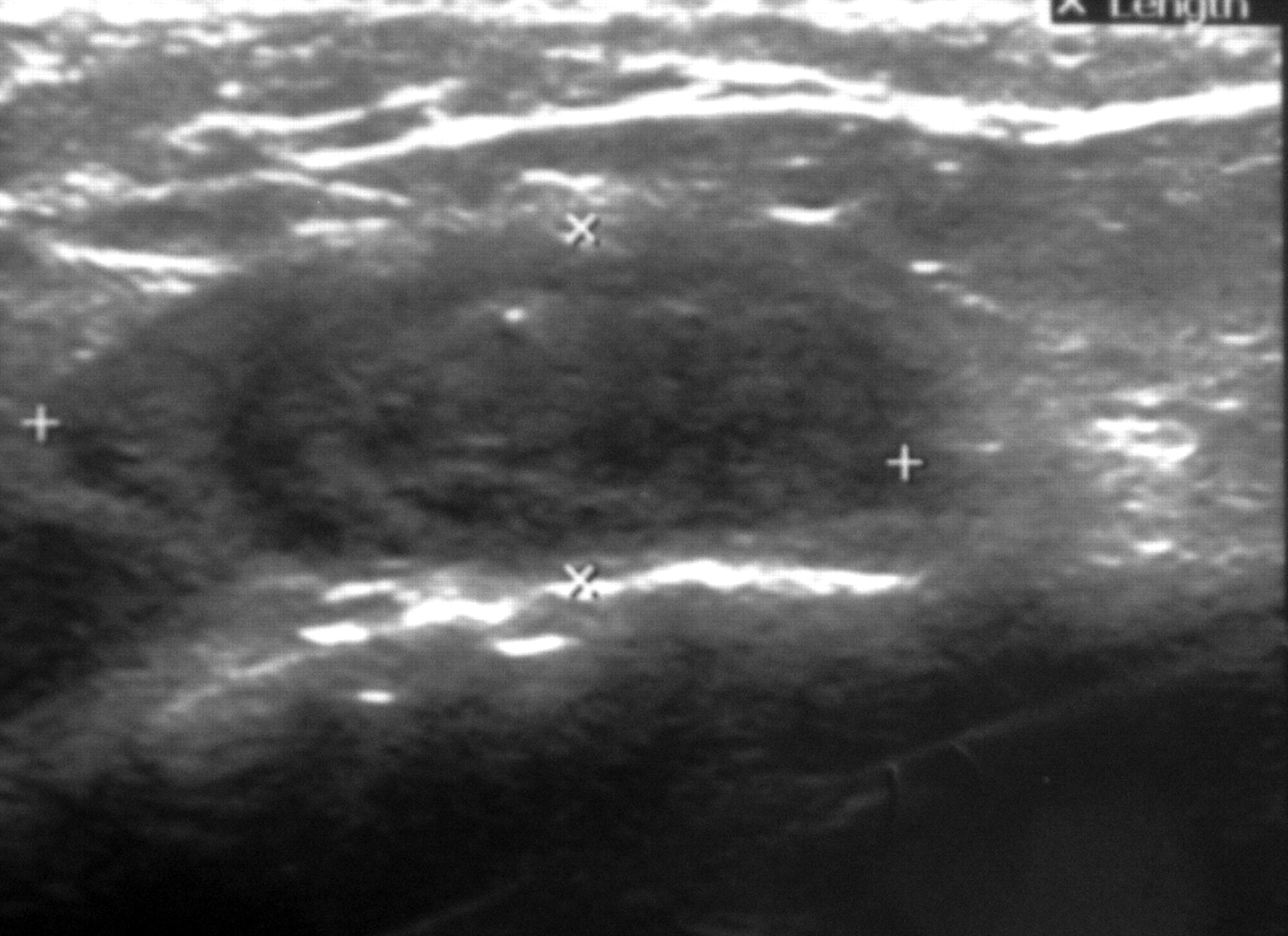

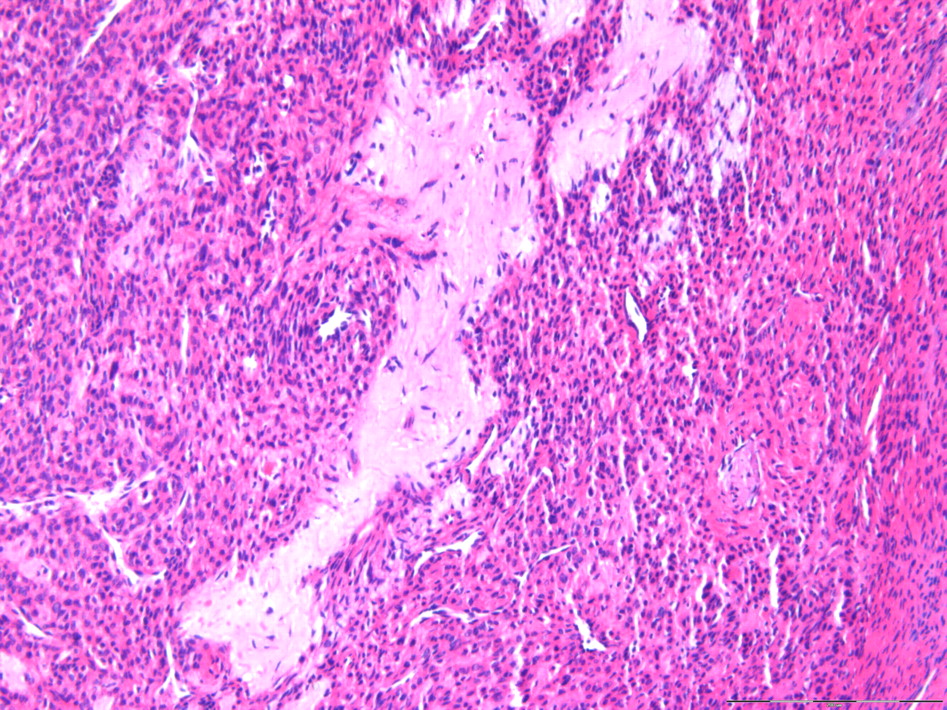
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3