A Twenty-five-Year-Old Woman with Restricted Left Shoulder Motion and Progressive Neck and Shoulder Pain
January 15, 2014
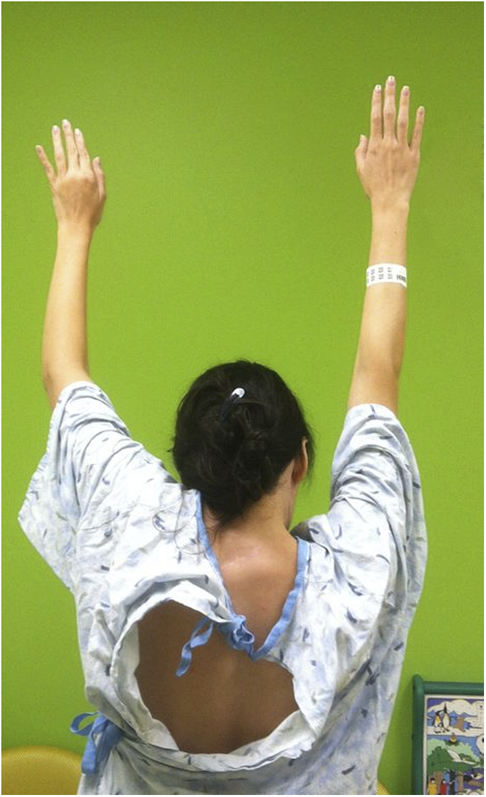
A twenty-five-year-old right-hand-dominant otherwise healthy woman presented with a lifelong history of restricted left shoulder motion and progressive neck and shoulder pain. She remembers having been told as a child that “something was wrong” with the shoulder, but she never had received treatment. She had recently started work as an administrative assistant and had noted increasing discomfort and fatigue in the neck and left shoulder, but she had no radicular symptoms. Physical examination revealed an elevated left shoulder. There was a tender, firm prominence between the left scapula and lower cervical spine. The patient had near normal active and passive motion of the affected left glenohumeral joint, but no scapulothoracic motion. The motion of the unaffected right shoulder girdle was normal. Active shoulder abduction on the left was 90°, with forward flexion of 100° (Figs. 1-A and 1-B). She could reach the anterior contralateral shoulder easily, but had difficulty reaching the occiput. With the arms adducted to her sides, she had equal internal and external rotation. She had mild restriction of neck rotation and bending to the left, with reported local discomfort. She had normal elbow, forearm, and hand function; the neurovascular examination was normal and there was no atrophy. Preoperative cervical spine and shoulder radiographs and computed tomography (CT) scans were made (Figs. 2-A, 2-B, and 2-C). There was an underlying posterolateral fusion at the left C5, C6, and C7 vertebral levels. Spinal CT showed no cord compression or syrinx.
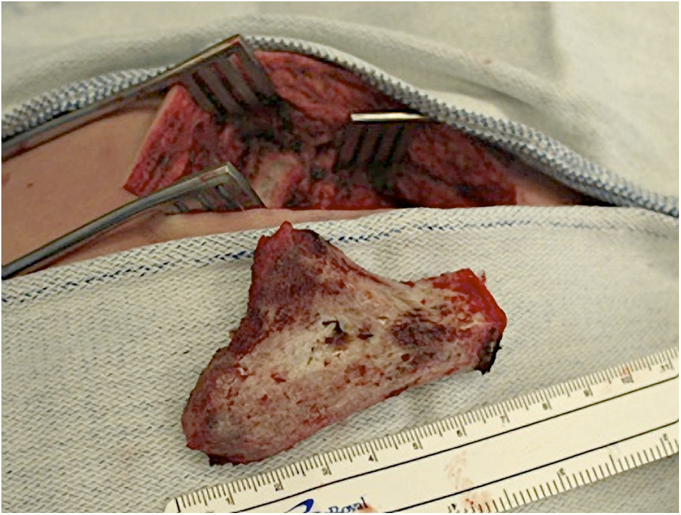
The decision was made to proceed with surgery to remove what was anticipated to be an omovertebral bone, with the goal of decreased neck and shoulder pain while improving shoulder motion. Aside from improving the contour of the shoulder, there was no intention of inferiorly shifting the location of the scapula. With the patient in the prone position, a curvilinear incision was made from the lower cervical spine to the superomedial border of the scapula. Blunt dissection yielded the omovertebral bone underneath the periscapular musculature. Subperiosteal dissection was performed circumferentially around the omovertebral bone, working from lateral toward the midline (Fig. 3-A). The fibrous union between the omovertebral bone and the scapula was removed with rongeurs. With CT as a guide, an osteotome was used to make an oblique cut through the omovertebral bone, starting 1 cm lateral to the midline and angling deep and laterally, away from the transverse processes. The omovertebral bone was removed intact (Fig. 3-B). We did not attempt to remove the posterior fusion mass from the adjacent cervical laminae. Passive scapulothoracic motion was dramatically improved. The soft-tissue defect was closed by simple reapproximation of the adjacent muscular soft tissues without any effort to reposition the scapula. The patient remained in the hospital overnight for observation and analgesia. The arm was placed into a simple sling, and she was instructed to begin active shoulder range of motion as tolerated and to wean the arm from the sling. She used oral ketorolac and oxycodone for five days for analgesia. By the two-week postoperative visit, the patient had stopped all medications and no longer used the sling. She demonstrated active left shoulder composite abduction and forward flexion of 140°, and she had returned to her job. Formal physical therapy was initiated. At the two-month and nine-month postoperative visits, the patient had a well-healed scar (Fig. 4-A). She had experienced relief from left neck and shoulder pain and was able to perform her job without limitations. She did not have any noteworthy change in cervical spine motion compared with preoperative motion, but the active left shoulder composite abduction and forward flexion was 150° (Figs. 4-B and 4-C); this motion was maintained at the nine-month follow-up visit. Left shoulder radiographs nine months after surgery showed no recurrent omovertebral bone or heterotopic bone formation.
Proceed to Discussion >>Reference: Gillespie B, Shaw BA, Waters P. Surgical excision of an omovertebral bone in an adult with untreated Sprengel deformity: a case report. JBJS Case Connector, 2013 Oct 09;3(4):e96.
Within two months after surgery, our patient had greatly improved shoulder motion and felt less pain. This was accomplished with simple excision of the omovertebral bone and did not require any attempt to place the scapula into a more anatomic position. Most published studies of Sprengel deformity discuss children and adolescents. Milder forms of the deformity are amenable to conservative management but should be followed until skeletal maturity because the deformity and functional loss can progress. Overall, these young patients can expect about 40° of improved shoulder abduction following surgical treatment in childhood with a scapular displacement surgery, such as the Woodward procedure. These gains are typically reserved for those patients undergoing surgery before six to eight years of age. Ross and Cruess reviewed thirty-six young patients who underwent simple excision of omovertebral elements and/or the proximal part of the scapula; the overall improvement of shoulder abduction was from 90° preoperatively to 126° at the time of final follow-up. However, many patients had mild or no improvement. After undergoing this type of procedure, our patient certainly exceeded this level of improvement, even in adulthood. The results of the other three published cases of surgical treatment of Sprengel deformity with an omovertebral bone in adulthood have been mixed, and our patient exceeds two of them with regard to shoulder motion. The most recently published case, reported by Füllbier et al., was a thirty-four-year-old woman whose chief symptoms were progressive gait ataxia and intermittent urinary incontinence. Imaging demonstrated an omovertebral bone that invaginated the posterior arch of the C6 vertebral body, causing spinal stenosis and subsequent cervical myelopathy. Preoperative restricted neck and shoulder range of motion was reported, but there were no additional details. Surgery involved a C6 laminectomy to decompress the spinal cord and partial excision of the omovertebral bone. At two years after surgery, the urinary incontinence had resolved; she had improved neck motion with less pain, but she had only slight improvement in gait ataxia and shoulder motion. Doita et al. presented the outcomes of two adult women following omovertebral bone excision for previously untreated Sprengel deformity. Both patients also had underlying Klippel-Feil syndrome. One patient had experienced substantial pain reduction and improved cosmesis, but at one year after surgery, the forward flexion had only improved from 110° to 120°, and shoulder abduction had only slightly improved from 95° to 100°. The other patient had been satisfied with the decreased pain and improved cosmesis three years after surgery, and the shoulder motion had been greatly improved. The forward flexion had increased from 115° to 165°, and the abduction had improved from 100° to 160°. At nine months after surgery, our patient was working without limitations and with much less pain. She had made large gains in shoulder motion and was quite happy with the results. She does not have a hypertrophic scar, recurrent bone formation, or recurrent pain/stiffness that has been seen in younger patients following surgery for Sprengel deformity. This case illustrates the importance of carefully evaluating adult patients who present late with possible Sprengel deformity. The presence of an omovertebral bone may indicate the role for simple excision with the expectation of improved shoulder motion, less pain, and improved cosmesis. Potential adult surgical candidates should be advised of the variable, but potentially positive, clinical response to simple excision of a symptomatic omovertebral bone.
Reference: Gillespie B, Shaw BA, Waters P. Surgical excision of an omovertebral bone in an adult with untreated Sprengel deformity: a case report. JBJS Case Connector, 2013 Oct 09;3(4):e96.
Cervical rib
Myositis ossificans of the lower cervical spine
Hypophosphatasia
Omovertebral process



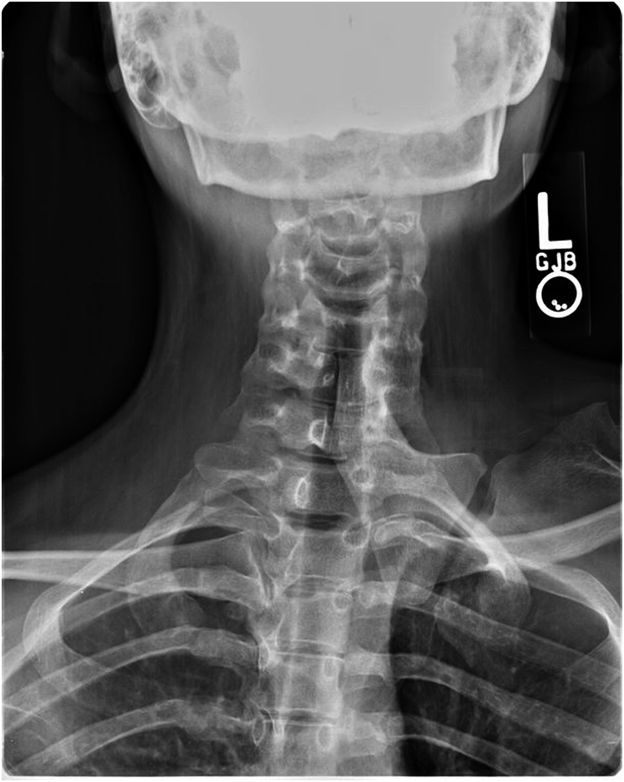


 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 2-C
Fig. 2-C Fig. 3-A
Fig. 3-A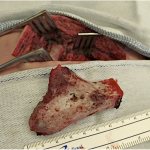 Fig. 3-B
Fig. 3-B Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B Fig. 4-C
Fig. 4-C