An 87-Year-Old Woman with a Worsening Skin Lesion
April 1, 2020
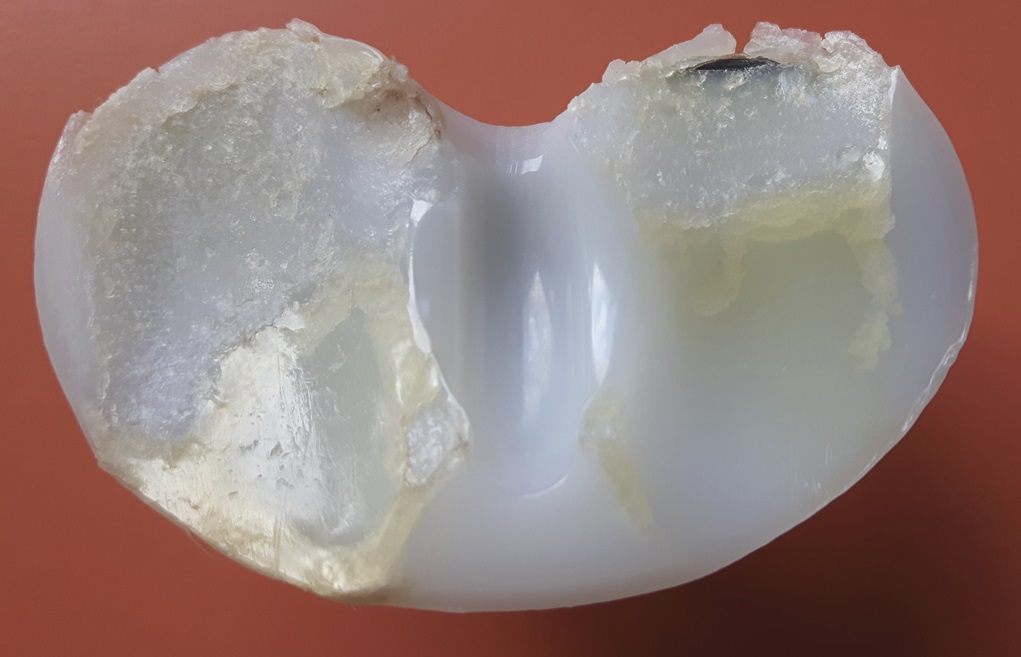
An 87-year-old woman with a body mass index (BMI) of 26.4 kg/m2 and a history of congestive heart failure presented 13 years after left total knee arthroplasty. She had received a cruciate-retaining, anatomic, graduated femoral component with a tibial monoblock component composed of molded ultra-high-molecular-weight polyethylene (Biomet). The procedure and rehabilitation were without complications, and she had satisfactory function for 12 years. One year before presentation, she developed instability and pain in the left knee, and her family doctor prescribed a knee brace. Two months before presentation, she was seen at a dermatology clinic with a 4 × 4-cm popliteal skin lesion. The dermatologist suspected lymphedema, probably after cellulitis. A punch biopsy showed inflammation of the skin with lymphohistiocytic infiltration, multinuclear giant cells, and small granulomas without necrosis. The superficial dermis contained neutrophilic granulocytes and extravasation of erythrocytes along with edema with spongiosis and parakeratosis in the epidermis. The patient was referred to a general surgeon, who subsequently performed an ultrasound examination and then referred the patient to the orthopaedic department. There were no signs of infection apart from a severe joint effusion, although the erythematous popliteal lesion had developed serous excretion with minimal ulceration (Fig. 1). Radiographs of the knee demonstrated anterior subluxation of the tibia and polyethylene wear (Fig. 2), and ultrasound showed a 13 × 11 × 6-cm popliteal cyst with a compressible homogenous mass not suspicious for malignancy. The serologic markers of inflammation were normal, but infection could not be excluded in the absence of cultures. Consideration was given to revision total knee arthroplasty, but the ulcerating skin lesion was more urgent to address to prevent further skin damage and a deep periprosthetic infection; therefore, the posterior mass was debrided first. During the excisional biopsy through a posterior approach, the implant was visible, clear synovial fluid was aspirated, and thick, yellowish-brown debris resembling pudding was evacuated through the popliteal cyst and was sent for culture (Fig. 3). Because there were no macroscopic signs of infection, the implant was not extracted during the same procedure. The wound could be closed primarily, and after later debridement of marginal skin necrosis, the wound healed without further complications. The histology of the excised lesion is shown in Figs. 4 and 5 (link to digital whole-slide images: Pathologic specimens Fig. 4-B and Pathologic specimens Fig. 5).
The microbiologic cultures were negative. The granulomatous inflammation associated with birefringent particles in the absence of acute inflammation indicates a macrophage and giant cell reaction to polyethylene wear debris extending into the soft tissue and skin.
Five months after popliteal surgery, 1-stage revision knee surgery was performed through a medial parapatellar arthrotomy and showed extensive synovitis and lateral polyethylene wear (Fig. 6). The components were easily removed because of implant loosening, and there were no signs of metallosis or extensive osteolysis of the distal part of the femur and the proximal part of the tibia. There was no erosion of the unresurfaced patella. Debridement of the knee joint was performed followed by revision with posterior stabilized stemmed femoral and tibial components and a polyethylene insert (Fig. 7). The patient’s recovery was without complications, and the cultures were negative. At the latest examination at 1 year postoperatively, the patient had experienced pain relief and had a stable knee joint without any clinical or radiographic complications.
Proceed to Discussion >>Reference: van Veen SC, Huizinga MR, van Raaij JJAM. Popliteal skin lesion due to wear disease in total knee arthroplasty: a case report. JBJS Case Connect. 2019 Dec;9(4):e0484.
Previous studies have shown that wear disease in patients with hip and knee joint arthroplasties is associated with load (activity level and weight), implant design (constrained compared with nonconstrained), alignment, ligamental balancing, metallosis, and thickness, quality, and sterilization method of the polyethylene insert. Positioning of the implant components might have influenced the development of wear in our case as well. The femoral component was slightly oversized, and in some flexion, the tibial component was in a mild varus and had a posterior slope of 7°, which is just within the manufacturer’s instructions. The radiograph after 13 years showed an increase of the posterior slope to 16°, suggesting subsidence. Wear debris is induced by wear and fatigue of the polyethylene insert; as a result, macrophages produce cytokines, which, in turn, cause bone resorption. Osteolysis and loosening of the implant increase micromotion at the component interface, leading to more extensive wear debris accumulation, a mechanism that was seen in our case as well. Wear particles cause synovitis and joint effusion and especially accumulate in pseudotumor-like cysts forming a granulomatous tissue mass, as was obvious in our case and has previously been described in both total hip and knee arthroplasty. These granulomas are nodules consisting of inflammatory cells phagocytizing the debris particles and can concomitantly be seen with central necrosis, fibrosis, or scar tissue within the capsule. The formed cysts compress surrounding structures; relevant structures around the knee are the tibial nerve and the deep veins causing correspondingly nerve palsy and thrombosis. Cysts can also invade periarticular soft tissues and bone, even leading to fractures. Expansion of the birefringent particle debris (i.e., polyethylene wear) containing cyst to just deep of the dermis after total knee arthroplasty has not previously been described. As a result of this aggressive continuous cyst, even the overlying popliteal skin contained giant cells with birefringent particles. The polyethylene particles induced an aseptic inflammation, which aggravated and caused a secondary mild ulceration of the skin, and evolved into acute necrotizing inflammation. Concluding, ulceration and necrosis were indirectly related to the polyethylene accumulation.
Although dermatitis and swelling have been described as hypersensitivity reactions to metal wear and polymethylmethacrylate in arthroplasty, our case is the first to describe wear disease presented with skin inflammation. The dermatitis in our case was localized superficial to the popliteal cyst, whereas allergic dermatitis due to prosthetic components is seen lateral to the anterior midline incision. Besides, allergic dermatitis can present eczematous, as the result of a delayed hypersensitivity reaction, resulting in a pruritic rash, which our patient did not have. Bone cement allergy can cause a fistula, which was not present in our case. However, the frailty caused by the inflamed skin resulted in serous excretion, a phenomenon that can be seen in severe cases of allergic dermatitis. Other similarities with an allergy include aseptic loosening of the implant. Polyethylene allergy has never been described in the literature, and so far, no one has suggested that this allergy exists.
Histologically, the foreign body response to metal-on-polyethylene implants is typically granulomatous and dominated by macrophages with only a few lymphocytes, which was the case in our patient, whereas an allergic reaction is characterized by abundant lymphocytes and limited numbers of macrophages. Granulomas and polyethylene particles can disseminate to the liver, kidney, spleen, lymph nodes, and blood. In the joint surrounding tissues, granulomatous tissue has only been described directly around the joint cavity, primarily located at the bone-implant interface or in a popliteal cyst like in our patient. Our case is the first to describe foreign body granulomas with giant cells containing birefringent particles in the popliteal skin that migrated from the knee joint.
No birefringent particles were found in the primary punch biopsy of the skin using polarized light. There were obvious multinuclear giant cells, although the causal agent could not be located. The excisional biopsy of the skin did show very small birefringent particles in the skin, some enclosed in multinuclear giant cells, in the proximity of multinuclear giant cells without birefringent particles. This leads to the hypothesis that the smallest polyethylene particles can migrate to the skin, although very few actually do; it could be advocated that some birefringent particles were situated close to the punch biopsy site.
These findings are relevant because this monoblock tibial component with conventional polyethylene is still being implanted. Furthermore, there are patients with similar unrevised total knee implants with conventional polyethylene. If these patients have an insufficient posterior cruciate ligament and/or a malaligned prosthesis, this is a complication that might occur in some cases.
It is essential that patients with an atypical inflammation of the skin with an underlying joint implant are referred to an orthopaedic surgeon for further analysis because it might be induced by implant failure. Besides, we would like to advise dermatopathologists to examine these biopsies with polarized light to check for birefringent particles.
Reference: van Veen SC, Huizinga MR, van Raaij JJAM. Popliteal skin lesion due to wear disease in total knee arthroplasty: a case report. JBJS Case Connect. 2019 Dec;9(4):e0484.
What is the diagnosis?
Cutaneous extension of a granulomatous reaction to polyethylene wear debris
Granulomatous inflammation consistent with mycobacterial or fungal infection
Metallosis involving skin over failed total knee prosthesis
Granulomatous inflammation consistent with sarcoidosis
Periprosthetic infection complicated by reaction to polyethylene debris





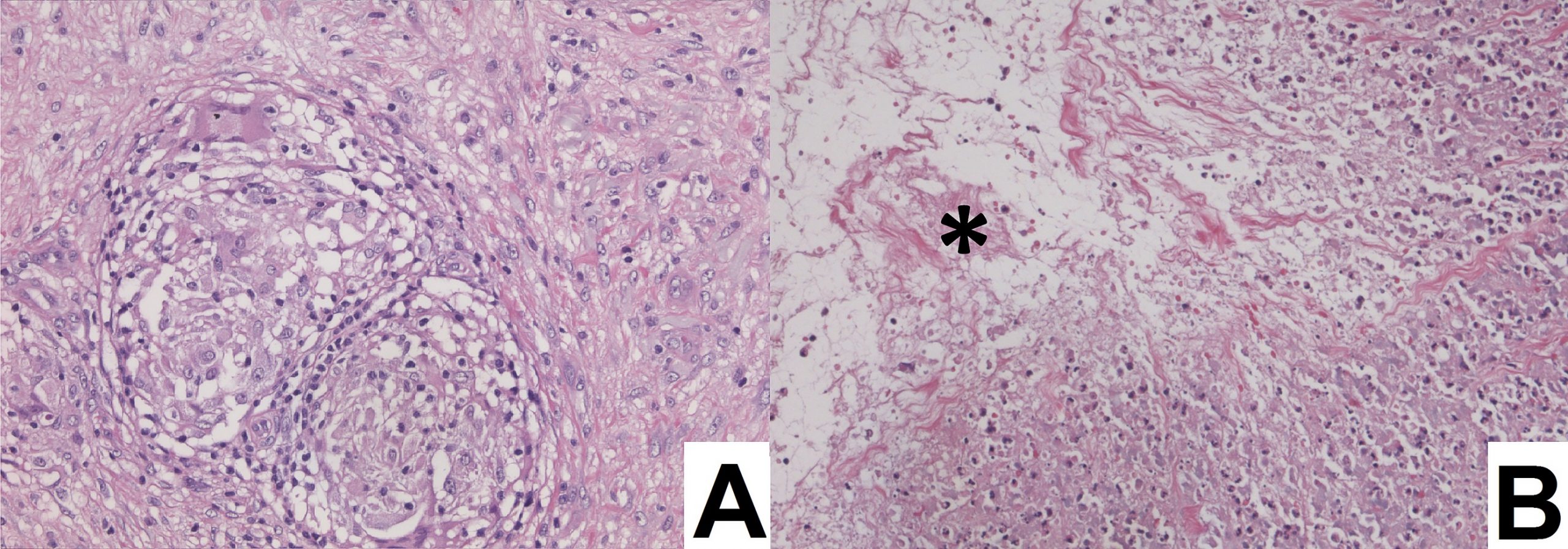
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4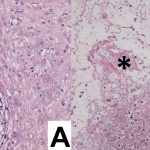 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7