A Female Athlete with Developing Pain in the Right Foot
March 2, 2016
A female shot-putter developed pain in the right midfoot when she was fourteen years old. Her medical history was negative for any rheumatologic disorders, diabetes mellitus, or trauma. The pain, located in the tarsal sinus and the lateral aspect of the midtarsal (Chopart) joint, was aggravated by sports activities. The findings on physical examination of the foot and ankle were nearly normal, with no restriction of range of motion and no redness, swelling, or increased local heat. Radiographs were negative for fracture, dislocation, soft-tissue injury, degenerative changes, cavus deformity, and talar beaking (Fig. 1). Because of persistent symptoms, additional imaging studies of computed tomography (CT) and magnetic resonance imaging (MRI) were obtained. On the basis of the results of the imaging, the patient was initially managed with an accommodative foot orthosis and physical therapy. Her symptoms then improved and she was able to participate in sports activities with the right ankle taped.
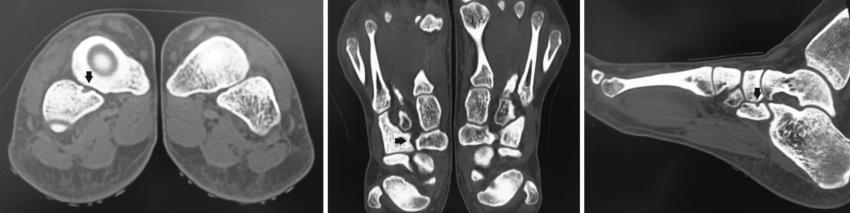
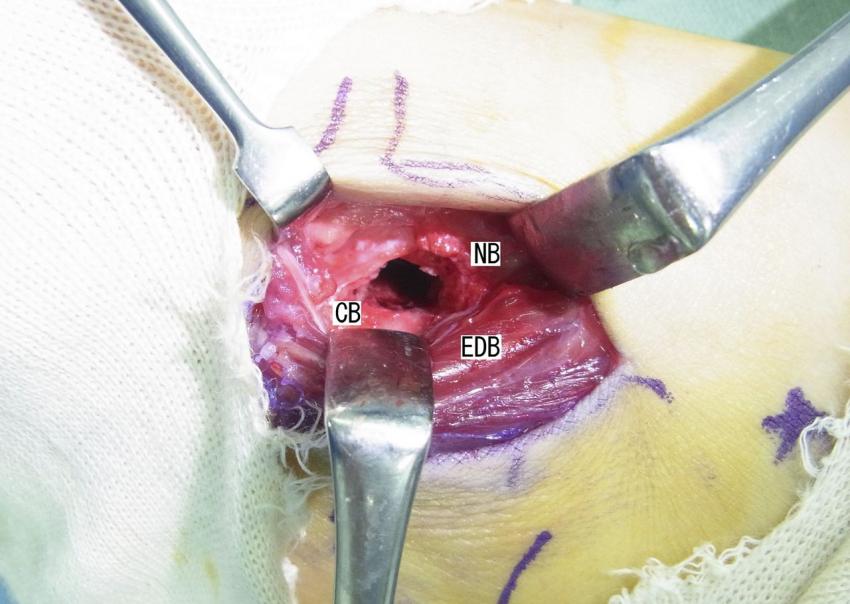
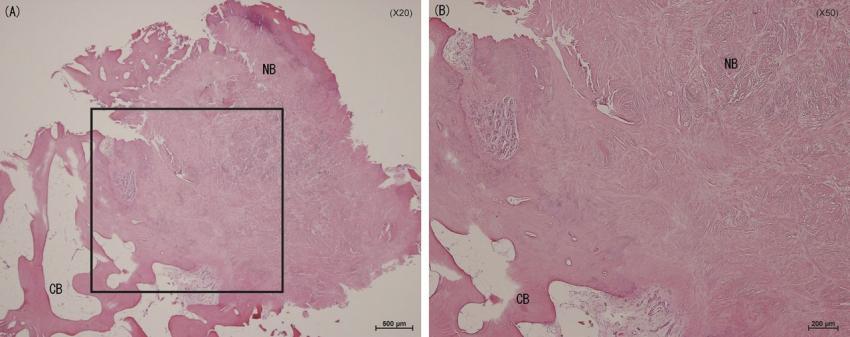
CT revealed a cystic lesion in the cuboid in contact with the navicular (Fig. 2). MRI showed an abnormal soft-tissue signal in the space between the cuboid and the navicular (Fig. 3). An incomplete fibrous cuboid-navicular coalition was suspected as a cause of the symptoms. However, two years later, the patient presented to our clinic because of a right ankle sprain. In addition to the new lateral ligament injury of the right ankle, she had pain at rest, pain with midfoot motion, and tenderness around the lateral part of the ankle and the midfoot, especially over the junction of the cuboid and the navicular. The symptoms persisted after the acute ankle sprain resolved, and she could not return to performing the shot put. A local anesthetic (lidocaine) with contrast medium was injected into the region between the cuboid and the navicular, and it relieved her pain temporarily (Fig. 4). The symptoms subsequently returned and became persistent. At the age of seventeen years, the patient elected to undergo surgery. A 5-cm linear skin incision was made over the dorsal aspect of the cuboid. The muscle belly of the extensor digitorum brevis was retracted laterally to expose a distinct fibrous bridge between the cuboid and the navicular. We resected the fibrous bridge along with the adjacent cortices of both the cuboid and the navicular to create a definite space between the two bones. Each cancellous bone surface was covered with bone wax (Fig. 5). Histological examination demonstrated that fibrous tissue had filled the area between the cuboid and the navicular. The fibers were seen to be arranged randomly under high magnification (Fig. 6). Immediately postoperatively, exercises to improve range of motion of the ankle and foot and muscle tightness were performed, and full weight-bearing was permitted after two weeks. The patient was able to return to playing sports two months after the procedure. At the time of follow-up, twelve months after the operation, the patient stated that she had been able to participate in a shot-put competition and experienced no pain. Her American Orthopaedic Foot & Ankle Society ankle-hindfoot score was 100.
Proceed to Discussion >>Reference: Kamiya T, Watanabe K, Teramoto A, Yamashita T. Cuboid-navicular tarsal coalition in an adolescent female athlete: A case report. JBJS Case Connect. 2015 Nov 11;5(4):e93.
Tarsal coalitions occur in less than 1% of the general population. Talocalcaneal and calcaneonavicular coalitions comprise 48% and 44% of all tarsal coalitions, respectively. Talonavicular and calcaneocuboid coalitions each make up another 1% of tarsal coalitions, and the remaining 6% occur in other tarsal joints. We have found only nine other reports of a cuboid-navicular tarsal coalition. Most of the cases of tarsal coalition between the cuboid and the navicular have involved osseous union and have been associated with a decreased range of motion of the subtalar joint. It is not difficult to diagnose a tarsal coalition on radiographs when an osseous bar between the cuboid and the navicular is observed. However, in the case of our patient, the coalition consisted of fibrous tissue and the radiographs did not reveal any obvious sign of coalition. Both CT and MRI aided in the diagnosis in this case. Nonetheless, the findings were relatively minor and included a small cyst in the cuboid and a nonspecific signal change in the narrow space between the cuboid and the navicular. The local injection of anesthetics into the coalition area was very helpful in making a definitive diagnosis in this case. Temporary pain relief was completely achieved after the injection, and we believe that such an injection of local anesthetics should be performed early in suspected cases of fibrous tarsal coalition. Tarsal coalitions are primarily treated conservatively. Activity modification, use of arch supports and other foot orthoses, and physical therapy may be helpful for individuals with symptoms. In our case, the patient was able to play sports following the use of these initial conservative measures and ankle-taping. However, her symptoms became more severe after she sustained a sprain of the lateral ligaments of the ankle. Because the pain persisted, she underwent operative management. A successful short-term outcome was achieved. A variety of operative approaches to the cuboid-navicular tarsal coalition have been described. Sarage et al. made a single 7-cm dorsolateral linear incision over the superior aspect of the cuboid and divided the extensor digitorum brevis muscle belly centrally. Johnson et al. reported that a one-finger-breadth-wide incision beginning inferior to the lateral malleolus and extending to the base of the fourth metatarsal, with medial retraction of the extensor digitorum brevis, could be used. We made a 5-cm linear skin incision over the dorsal aspect of the cuboid and retracted the extensor digitorum brevis muscle belly laterally, and the coalition between the cuboid and the navicular was readily identified with use of this approach. While in our case the resected space was filled with bone wax, the use of adipose grafts or extensor digitorum muscle interposition has also been described following coalition resection to prevent recurrent bridging. In our case, only short-term success is reported and long-term follow-up will be required to ensure continued success of the treatment employed.
Reference: Kamiya T, Watanabe K, Teramoto A, Yamashita T. Cuboid-navicular tarsal coalition in an adolescent female athlete: A case report. JBJS Case Connect. 2015 Nov 11;5(4):e93.
Osteonecrosis of the talus
Lymphoma of bone
Incomplete cuboid-navicular coalition
Osteoblastoma of the navicular
Osteoid osteoma of the cuboid


 Fig. 1
Fig. 1 Fig. 2
Fig. 2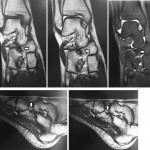 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6