A Seventy-two-Year-Old Man with a Fractured Femur
April 6, 2016
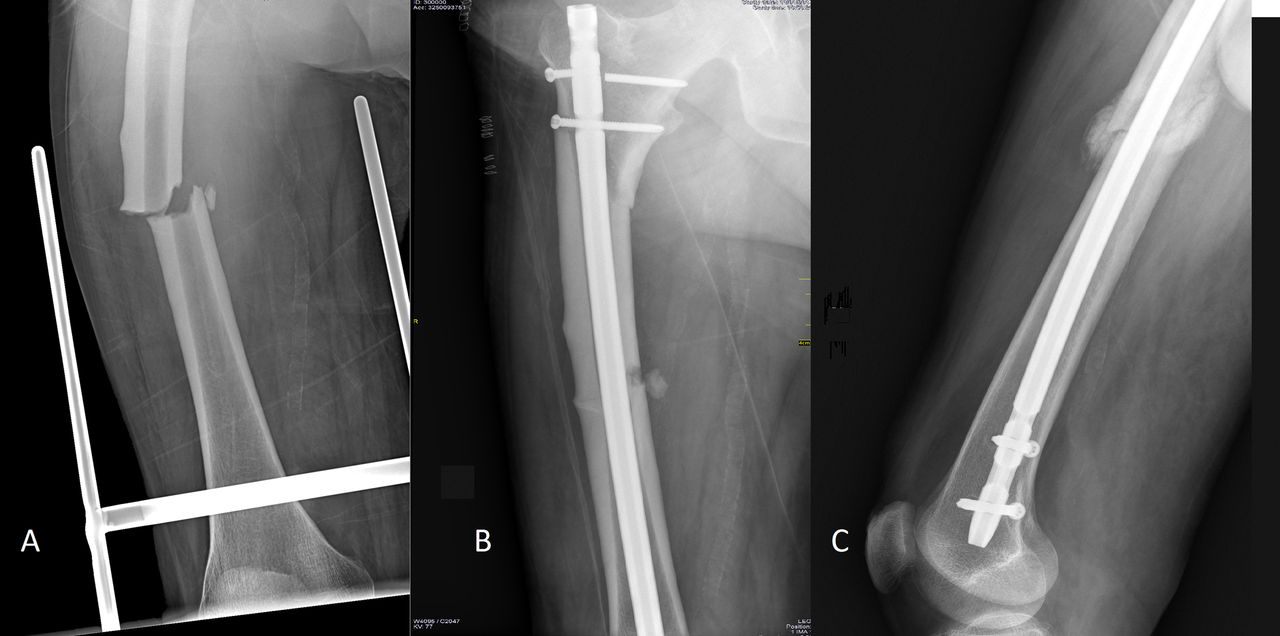
A seventy-two-year-old male patient was admitted to the hospital with a fracture of the left femur due to a low-energy trauma sustained when he fell from a step (Fig. 1-A). He underwent surgery and the fracture was fixed with anterograde femoral nailing (Fig. 1-B). The first fracture was consolidated five months after surgery (Fig. 1-C). Twenty-two months later, he sustained a second fracture that was similar to the first but in his contralateral femur. The patient had fallen from a standing position when the bus in which he was traveling came to an abrupt stop. The patient did not describe any symptoms prior to the occurrence of either fracture, nor had radiographs of either femur been made before the incidents. The patient had smoked for forty years. He had chronic renal insufficiency, mild to moderate arterial hypertension, hyperuricemia, bronchial asthma, glucocorticoid-induced osteoporosis, interstitial lung disease, and anti-neutrophil cytoplasmic antibody (ANCA)-positive Churg-Strauss syndrome. The patient also had repetitive deep vein thrombosis with residual postphlebitic syndrome and a negative thrombophilia screen. He had been treated with inhaled corticosteroids for thirteen years, alendronate weekly for eleven years, and acenocoumarol for five years.
It was determined that the patient had sustained a second, atypical fracture so quickly after the first one because of his use of alendronate, a bisphosphonate. Successive checkups showed a slower evolution of the second fracture (Fig. 2-A). Therefore, the patient began treatment with teriparatide in the second month after the operation (Fig. 2-B). The consolidation of the second fracture was confirmed seven months after the operation (Fig. 2-C). The patient died two years later, as a consequence of an aggravation of his chronic pulmonary disease and an immobility syndrome.
Proceed to Discussion >>Reference: Román M, de Prado A, de Tembleque FR. Bilateral atypical femoral fracture in a man on long-term bisphosphonate and glucocorticoid therapy: A case report. JBJS Case Connect. 2015 Apr 22;5(2):e36.
Low-energy transverse or short oblique femoral fractures have been observed to occur in patients on bisphosphonate therapy. These fractures are noncomminuted or minimally comminuted with a medial spike and are located in the subtrochanteric region and diaphysis of the femur, presenting focal cortical thickening. Their morphology suggests a preexisting stress fracture of the femoral lateral cortex progressing to a full fracture. A similar radiographic pattern can be found in disorders such as adult hypophosphatasia, cross-linked hypophosphatemia, osteopetrosis, or Paget disease. Recently, the Medicines and Healthcare products Regulatory Agency (MHRA) has reported rare cases of atypical femoral fracture in patients receiving 60-mg denosumab for more than 2.5 years. The incidence ranges from one per 1000 patients per year to 5.9 per 100,000 person-years. According to the literature, the percentage of patients affected by atypical femoral fracture who were treated with bisphosphonates is between 30% and 90%. A systematic review published in 2010 observed that 84% of patients with atypical femoral fracture had undergone a prolonged treatment with alendronate and found a relationship between the atypical femoral fracture and exposure to glucocorticoids. In their study, Meier et al. concluded that such fractures are time-dependent. However, atypical fractures have also been observed in patients never exposed to these drugs. Furthermore, circumstances such as Asian ethnicity, glucocorticoids, and proton-pump inhibitors have been described as risk factors; there has been a case associated with a prolonged exposure to estrogens. Corticotherapy for more than six months, active rheumatoid arthritis, and serum 25(OH)-vitamin D levels below 40 nmol/L were described by Girgis et al. as potential risk factors. Lo et al. found that women who had sustained atypical fractures were younger than those who had sustained osteoporotic femoral fractures. A recent study using the French National Database revealed that the adjusted risk of sustaining an atypical femoral fracture is substantially higher in cases of obesity and dementia compared with the risk of sustaining a hip fracture. However, this adjusted risk is lower in cases of hypertension. A prolonged inhibition of bone turnover would cause an increase of secondary mineralization and the subsequent homogeneity and fragility of the bone. Thus, an insufficiency fracture appears at the point of maximum mechanical stress. Bala et al. suggested that prolonged use of alendronate is associated with the alteration of micromechanical properties, as a consequence of a reduction of mineral crystallinity. An abnormality in collagen crosslinks caused by nonenzymatic glycation end-product accumulation may increase bone fragility. Other hypotheses have suggested a heterogeneous form of osteoporosis, a small subgroup of the population more susceptible to the effects of a prolonged suppression of bone turnover, the presence of osteoclasts physiologically vulnerable to bisphosphonates, or an alteration in osteoblastic function. Vascular implication and bacterial implication have also been suggested. In addition to the case definition of atypical femoral fracture given by the task force of the American Society for Bone and Mineral Research, Schilcher et al. observed a fracture angle of 75° to 105°, a local reaction in the form of bone callus, and a diaphyseal location, when describing a case of atypical fracture. Rosenberg et al. suggested that the most sensitive, specific, and precise criteria to make a diagnosis are a focal cortical thickening and a transverse fracture line. Prodromal thigh pain has been reported in 70% to 75% of cases and the patients may describe this symptom anytime from two months to one week before diagnosis. Magnetic resonance imaging is useful when radiographic results are normal or inconclusive for patients treated with bisphosphonates who present with an ache in the upper thigh. La Rocca Vieira et al. suggested that the bone turnover markers serum C-telopeptide and urine N-telopeptide are the most useful parameters when identifying patients with asymptomatic fractures or those at risk of developing them. Contralateral involvement occurs in almost 50% of cases, according to Shane et al. Dell et al. demonstrated that the incidence of bilateralism in patients who continued treatment for more than three years after the first fracture was 41.2%. In incomplete fractures, the results of conservative treatment (load limitation and electrical stimulation) are not encouraging. Therefore, prophylactic intramedullary nailing must be considered if moderate to severe pain is present, if pain or a fracture line persists after three months of conservative treatment, or if fracture progression is identified by serial monitoring. In complete and displaced fractures, the long intramedullary nail technique is used in endochondral fracture repair (not altered by bisphosphonates). Potential complications include pseudarthroses (Weil et al. established a consolidation rate of only 54%), a delay in consolidation (in 26% according to Shane et al. and 39% according to Giusti et al.), and a difficulty in nail insertion with intraoperative fractures as in this case. Currently, there is a consensus for interrupting bisphosphonate therapy after five years in patients who have an adequate bone mineral density. There are new treatment guidelines and therapeutic algorithms to facilitate the management of these patients. The duration of this “drug holiday” depends on the patient’s fracture risk and the pharmacokinetics of the bisphosphonates used. We wish to highlight the need for a rigorous follow-up of certain patients to avoid this high-morbidity event.
Reference: Román M, de Prado A, de Tembleque FR. Bilateral atypical femoral fracture in a man on long-term bisphosphonate and glucocorticoid therapy: A case report. JBJS Case Connect. 2015 Apr 22;5(2):e36.
Osteogenesis imperfecta variant
Steroid-related osteoporosis
Atypical femoral fracture related to bisphosphonate use
Osteopetrosis
Osteomalacia


 Fig. 1
Fig. 1 Fig. 2
Fig. 2