A 55-Year-Old Woman with Persistent Wrist Pain
February 1, 2017
A 55-year-old right-hand-dominant woman with no noteworthy medical history initially had presented to an outside hospital in July 2012 with left ulnar-sided wrist pain attributed to a hypermobile fifth ray (Fig. 1). She had been treated with fifth carpometacarpal fusion, which had been supplemented with pin fixation and an allograft in June 2013. The pain persisted, and she developed a distal ulnar nerve palsy with loss of intrinsic function as well as a low ulnar claw hand, which originally was attributed to hardware migration. The patient next underwent nerve release with hardware and scar removal in November 2013 for presumed nerve entrapment. After returning again with pain, swelling, and erythema, she underwent operative debridement in April 2014 for suspected infection and osteomyelitis. No purulence was encountered intraoperatively, prompting a biopsy for histopathologic examination.
The patient presented to our institution for additional evaluation in May 2014, 2 years after the initial symptoms. Physical examination revealed swelling along the ulnar aspect of the dorsal part of the hand, muscle wasting most notable along the first dorsal interosseous muscle, and mild clawing of the ulnar digits (Fig. 2). Magnetic resonance imaging (MRI) demonstrated a mass with an epicenter along and radial to the fifth metacarpal (Fig. 3), and a bone scan demonstrated uptake in the ulnar aspect of the left hand.
On the basis of the outside diagnosis, the medical oncology service initiated a neoadjuvant chemotherapy regimen designed to treat possible metastases and to shrink the primary tumor. After 3 cycles of chemotherapy, physical examination showed less wasting of the interossei, decreased clawing, and nearly complete resolution of the ulnar-sided mass. Posttreatment MRI demonstrated a substantial decrease in the size of the mass. Given the excellent clinical response, we believed that the tumor could be resected via a fifth ray resection with tight margins of 0.5 to 1 cm and preservation of the fourth ray.
The patient underwent fifth ray resection in August 2014. The entire lesion was resected en bloc with the fifth ray (Figs. 4-A, 4-B, and 4-C). Particular attention was drawn to areas of possible contamination from previous incisions and procedures. The extent of the diseased tissue, combined with the previous carpometacarpal fusions, required sacrificing the insertions of the flexor carpi ulnaris and extensor carpi ulnaris muscles, and only thin dorsal skin was available to cover the ulnar border of the hand (Fig. 4-B).
Histology from the resection specimen is shown in Figures 5-A, 5-B, and 5-C.
The patient completed 13 cycles of chemotherapy, and at the 22-month follow-up, routine surveillance imaging showed no evidence of recurrence or metastatic disease. The patient was happy with the progress and pleased with the cosmetic appearance and functionality of the hand (Figs. 6-A and 6-B). Hypersensitivity to pain around the thin dorsal skin had improved with time and was no longer limiting activity (Fig. 6-C). The altered wrist mechanics caused weakened grip strength and a mildly extended and radially deviated wrist position, which improved with therapy.
Immunohistochemical stains of the initial biopsy specimen showed that the neoplastic cells were positive for CD99 and negative for desmin, SMA, CD3, CD20, TdT, CK OSCAR, TTF1, snaptophysin, NSE, EMA, CK7, CK AE1/AE3, chromogranin, and CD45. Those immunohistochemical stains help to exclude diagnoses of rhabdomyosarcoma, lymphoma, and primary or metastatic carcinoma and suggest a primitive neuroectodermal tumor or Ewing sarcoma. Reverse transcriptase-polymerase chain reaction evaluation demonstrated EWSR1 (Ewing sarcoma breakpoint region 1)-FLI1 and EWSR1-ERG fusion transcripts. Validation studies showed the clinical sensitivity to be 91% and the specificity to be 100% for the diagnosis of Ewing sarcoma (ES).
Proceed to Discussion >>Reference: Mahan MC, Frisch N, Durrant B, Parsons T III, Woods T, Mott M. Ewing sarcoma in the fifth metacarpal of an adult woman: a case report. JBJS Case Connect. 2016 Dec 14;6(4):e95.
ES presenting in the fifth metacarpal of an adult woman is exceedingly rare. The clinical and radiographic findings of ulnar-sided wrist pain with minor radiographic changes can generate a broad differential diagnosis. The similarities between ES and infection are well described; however, other benign and malignant tumors must be ruled out. Osteosarcoma, primary lymphoma, acute leukemia, undifferentiated high-grade pleomorphic sarcoma, and metastasis all may have similar clinical presentations. Morphologically, ES has a similar appearance to other small round blue cell tumors such as small-cell osteosarcoma, rhabdomyosarcoma, primitive neuroectodermal tumor, and other related tumors in the Ewing sarcoma family of tumors (EFT). It is important to consider information from the history, physical examination, radiographs, advanced imaging, and tissue biopsy with histologic, molecular, and immunohistochemical analysis.
The EFT includes a group of neoplastic diseases that share histologic/immunohistochemical characteristics and nonrandom chromosomal translocations. The majority of EFT neoplasms express a surface glycoprotein known as CD99. Although CD99 expression is a sensitive marker for EFT, it lacks specificity because other neoplasms, including rhabdomyosarcoma, and even normal tissue express this glycoprotein. Much more specific to ES is a unique pattern of translocations involving the EWSR1 gene on chromosome 22. Up to 90% of the EFT expresses the recurrent translocation, t(11,22)(q24,q12), which fuses the 5′ end of the EWSR1 gene on chromosome 22 to the 3′ end of the FLI1 gene on chromosome 11.
Patients with atypical presentations of prolonged hand pain, including night pain and pain at rest, and/or destructive lesions with soft-tissue masses warrant a more advanced workup. The classic radiographic features of ES may not be present or may be more difficult to appreciate in the hand. Soft-tissue masses with any bone changes mandate additional investigation with advanced imaging and biopsy. Noncystic solid masses without clinical symptoms of infection should raise the possibility of neoplasm. Because of the rarity and complexity of these tumors, sarcomas should be treated at institutions with multidisciplinary teams, and surgical treatment should be performed by an orthopaedic oncologist.
The workup of our patient included radiographs and MRI of the affected hand, bone scintigraphy, and computed tomography of the chest. The establishment of a definitive diagnosis was completed with biopsy specimens. With this patient, the biopsy was performed at an outside institution at the time of a planned debridement for infection. Fortunately, when apparently noninfectious material was encountered, the specimen was sent for histopathologic examination in addition to cultures.
Optimal treatment of upper-extremity bone tumors requires a careful balance of local tumor control and preservation of hand function. With fifth ray resection, loss of subcutaneous padding on the ulnar border of the hand leaves only thin skin with subcutaneous bone, which can be symptomatic. At the 22-month follow-up, the patient was satisfied with the cosmetic appearance and functionality of the hand.
Reference: Mahan MC, Frisch N, Durrant B, Parsons T III, Woods T, Mott M. Ewing sarcoma in the fifth metacarpal of an adult woman: a case report. JBJS Case Connect. 2016 Dec 14;6(4):e95.
What is the diagnosis?
Invasive basal cell carcinoma
Ewing sarcoma
Dedifferentiated chondrosarcoma
Metastatic carcinoma, consistent with lung origin
Malignant non-Hodgkin lymphoma


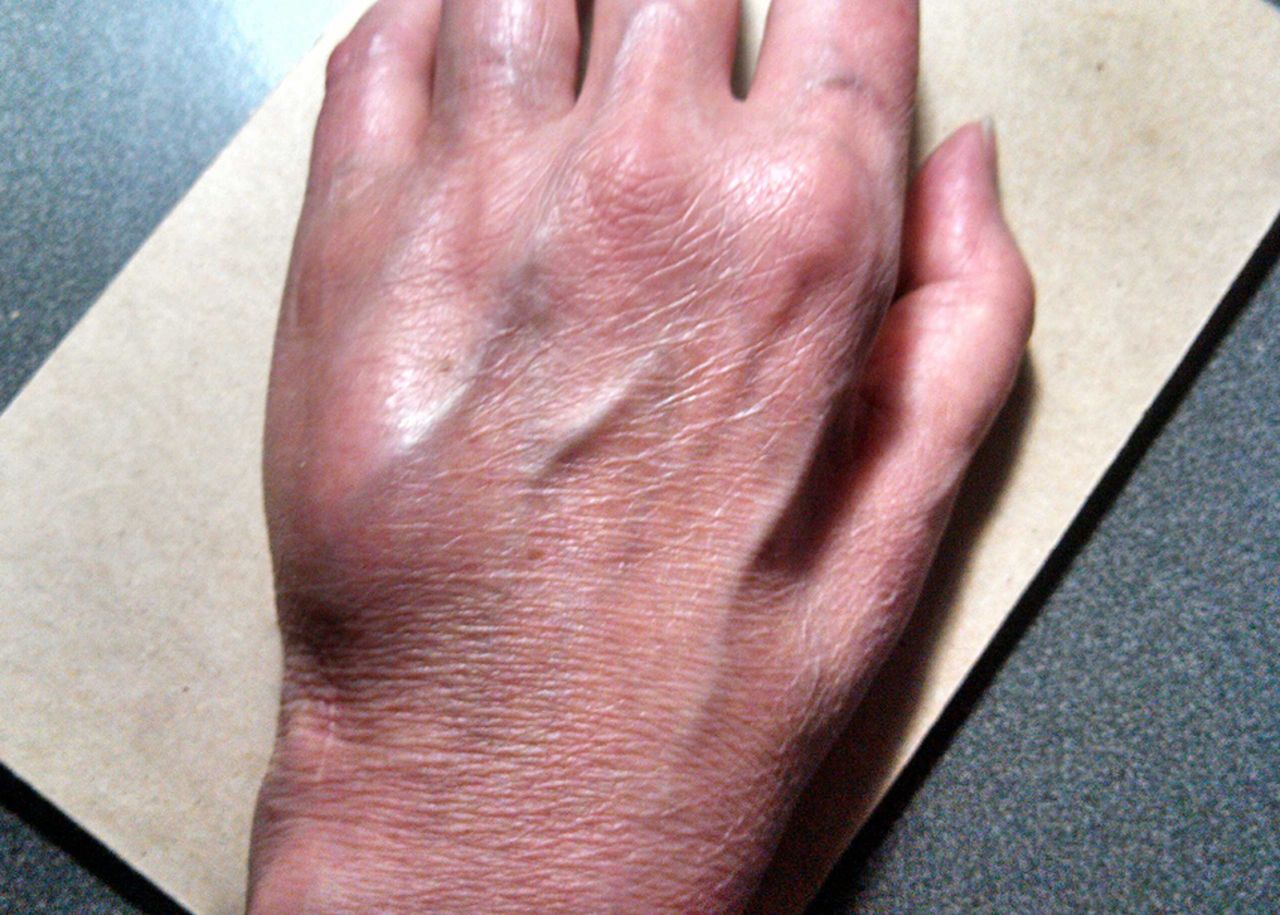
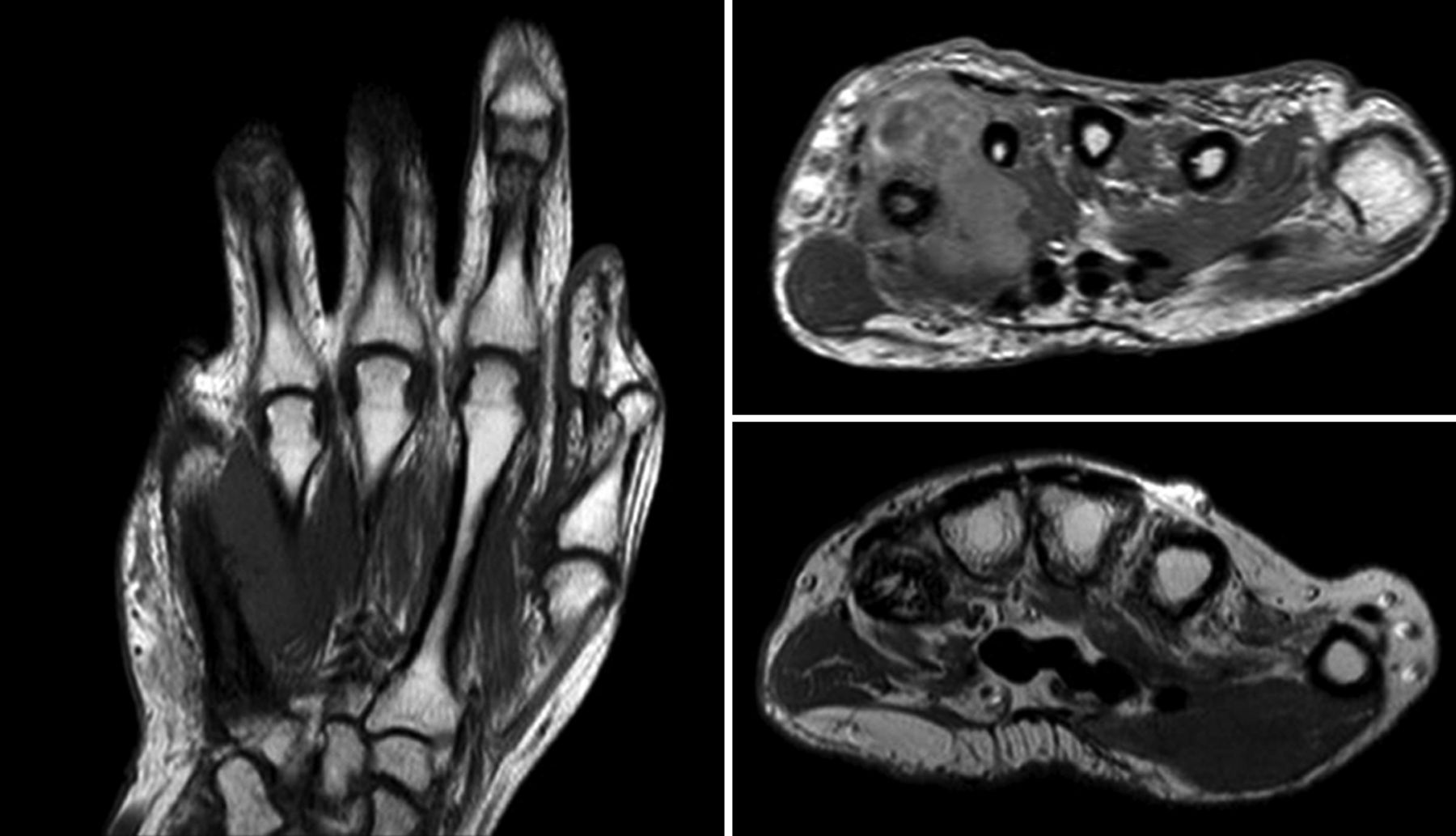



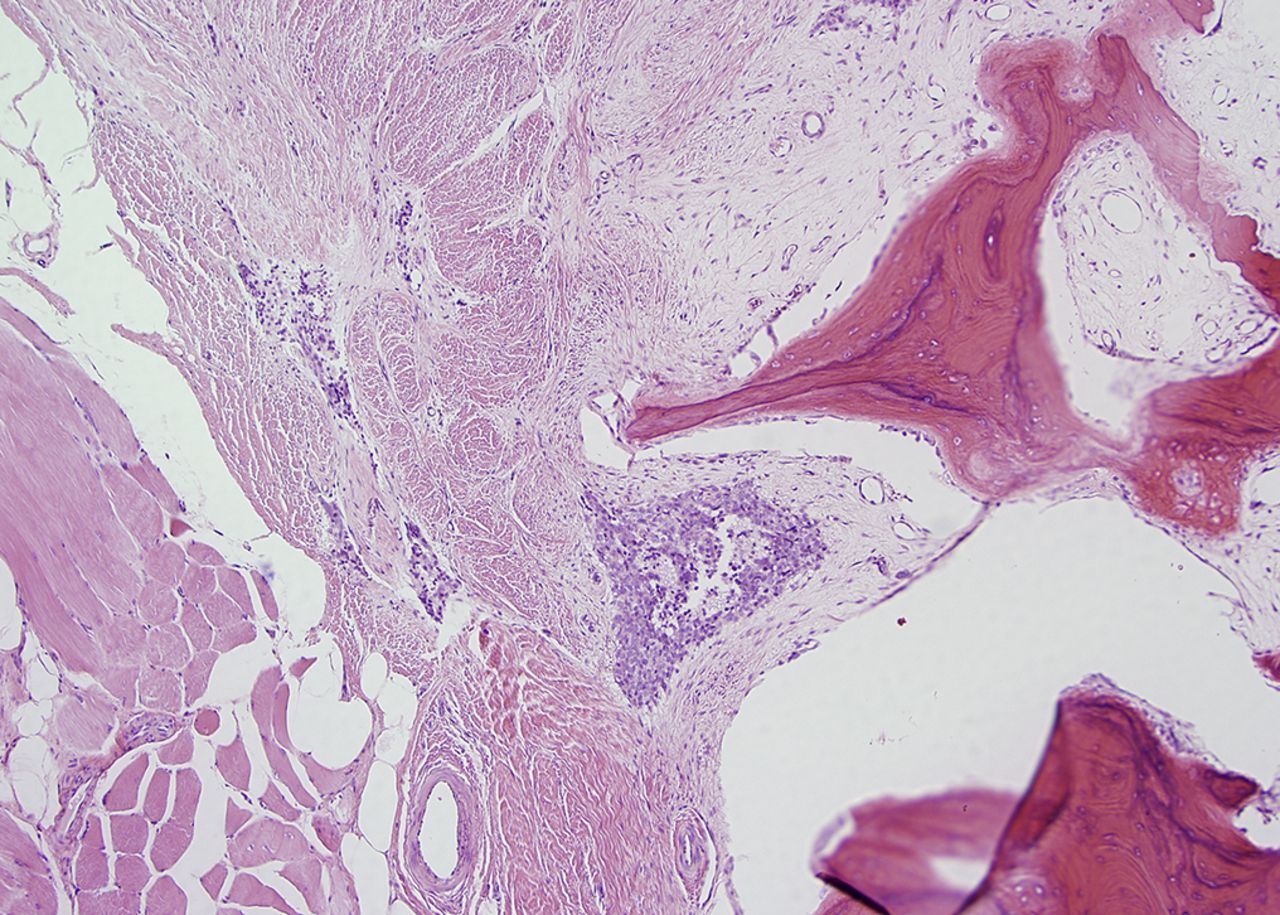
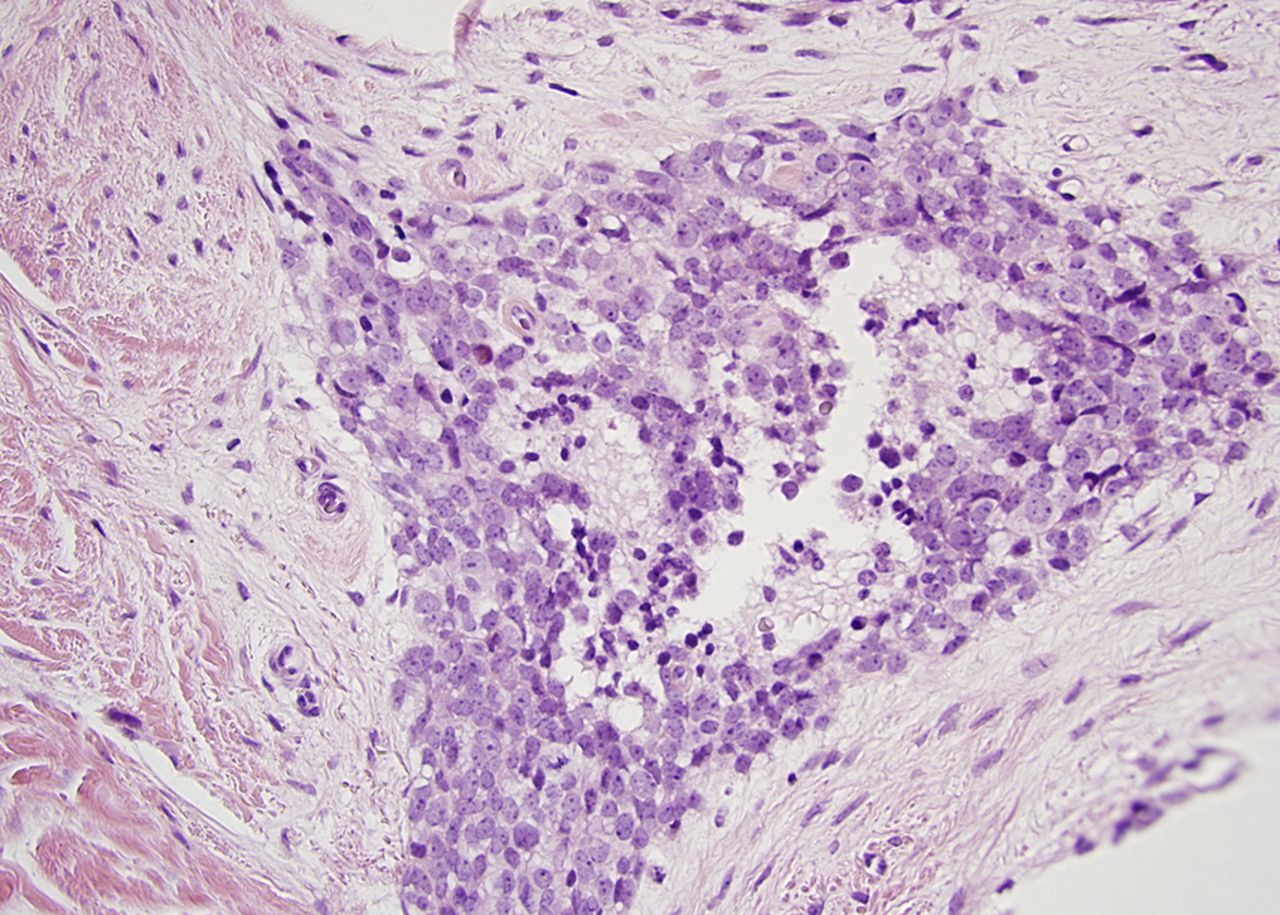
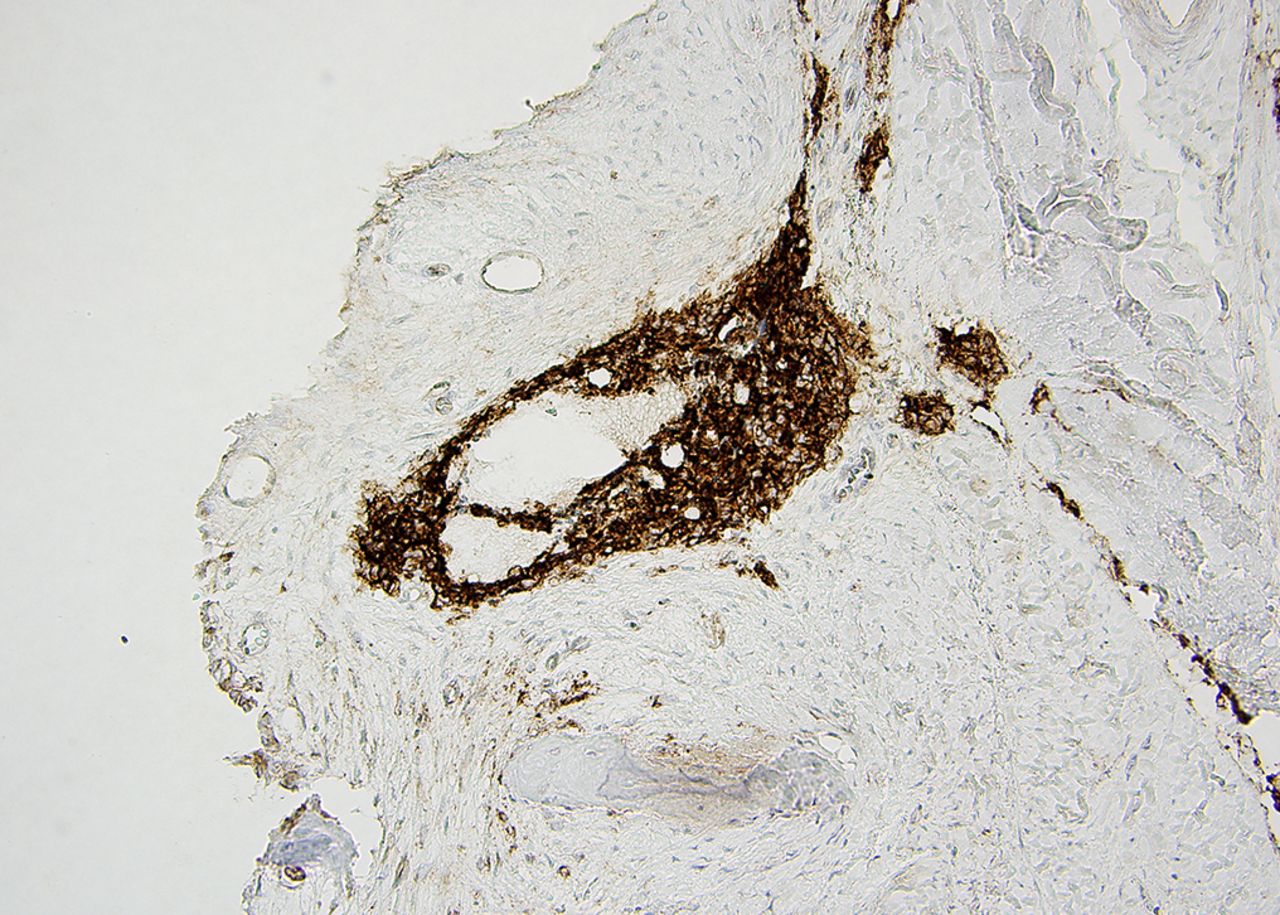



 Fig. 1
Fig. 1 Fig. 2
Fig. 2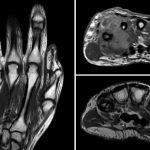 Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B Fig. 4-C
Fig. 4-C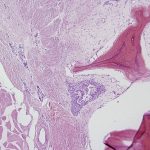 Fig. 5-A
Fig. 5-A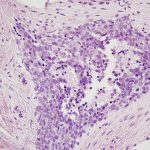 Fig. 5-B
Fig. 5-B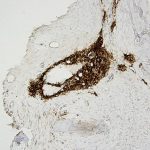 Fig. 5-C
Fig. 5-C Fig. 6-A
Fig. 6-A Fig. 6-B
Fig. 6-B Fig. 6-C
Fig. 6-C