A previously healthy eleven-year-old boy sustained an anterior cruciate ligament (ACL) tear of the left knee while riding a dirt bike. After discussion, the family elected to manage the injury nonoperatively with physical therapy and bracing until the boy was closer to skeletal maturity. He was seen again at age fourteen years with narrowed physes and maturity of at least Tanner Stage 3. Because of continued symptoms of instability, he underwent transphyseal arthroscopic-assisted ACL reconstruction (ACLR) with a quadrupled hamstring autograft (Fig. 1). Femoral fixation was performed with an ENDOBUTTON (Smith & Nephew), and tibial fixation was achieved with a 9-mm × 20-mm Bio-Interference screw (Arthrex) made of poly-L-lactic acid and backed up with a screw-and-washer post in the tibia. He additionally underwent repair of a peripheral tear of the posterior horn of the lateral meniscus with use of two horizontal mattress sutures with the all-inside FAST-FIX system (Smith & Nephew). The patient tolerated the procedure well and was discharged home. At the first follow-up visit at three weeks postsurgery, he reported fevers up to 101°F, headache, and abdominal pain. He did not report any knee pain. The primary care physician had diagnosed him two days earlier with a viral infection, and he was started on cephalexin therapy for unknown reasons. The wounds appeared benign on physical examination, and he did not have substantial pain with range of motion. An arthrocentesis was performed for a moderate effusion. The aspirate revealed 11,880 nucleated cells with a negative Gram stain. Other laboratory tests revealed a white blood-cell (WBC) count of 9900 cells/µL (normal range, 3400-10,200 cells/µL), an erythrocyte sedimentation rate (ESR) of 55 mm/h (normal range, 0-15 mm/h), and a C-reactive protein (CRP) level of 95.5 mg/L (normal range, 0-10 mg/L). Given the elevated inflammatory markers, the patient was admitted for administration of intravenous antibiotics. Because a short course of observation failed to show a substantial decline in the ESR or CRP level, he underwent arthroscopic debridement and irrigation at three weeks postsurgery, which revealed a benign joint with only mild hypertrophic synovium and an intact ACL graft (Fig. 2). The tibial wound was explored and revealed some necrotic material at the base of the tibial tunnel, but there was no gross purulence. The Infectious Diseases Department was consulted, and the patient was discharged on empiric clindamycin and levofloxacin therapy. The patient advanced appropriately in physical therapy and was able to jog. However, five months following the debridement and irrigation, he again had progressive erythema and focal fluctuance of the tibial incision. He had no fever, joint effusion, or pain with palpation or range of motion. Laboratory tests were normal, with a WBC of 6300 cells/µL, an ESR of 2 mm/h, and a CRP level of 2.6 mg/L. Magnetic resonance imaging (MRI) demonstrated synovitis, an intact but attenuated graft, and increased signal in the proximal part of the tibia near the area of the screw, as well as an associated fluid collection (Fig. 3).
After discharge, the intraoperative cultures from the initial debridement ultimately grew Mycobacterium fortuitum. The patient was diagnosed with a mycobacterial infection. The antibiotic regimen was changed to a six-month course of clarithromycin and levofloxacin. Repeat debridement and irrigation was performed, which demonstrated purulence and necrotic material upon opening of the tibial incision. The Bio-Interference screw and the tibial post screw and washer were removed. There was no longer graft in the tibial tunnel to which the Bio-Interference screw was apposed. The tunnel was curetted and irrigated copiously. Arthroscopy demonstrated no intra-articular purulence, and the graft had appropriate tension to probing and the Lachman maneuver. Intraoperative cultures remained negative. The patient was continued on azithromycin and levofloxacin therapy at that time. Six weeks following the second debridement, the patient returned with serous drainage from the tibial wound without increased pain, fever, or signs of instability. MRI demonstrated continued increased signal in the proximal part of the tibia around the tibial tunnel, concerning for ongoing osteomyelitis with the formation of an articular sinus tract (Fig. 4). A third debridement and irrigation was performed. Again, there was no substantial intra-articular pathology, and there was necrotic material in the tibial tunnel (Fig. 5). A high-speed burr was used to debride the sclerotic rim of bone within the tibial tunnel that was potentially harboring an indolent infection, and the tibial tunnel was bone-grafted with cancellous allograft that was mixed with tobramycin powder and soaked in saline solution. This local antibiotic was selected because the organism was sensitive to aminoglycosides, fluoroquinolones, and sulfamethoxazole/trimethoprim. Biopsy of the proximal part of the tibia was consistent with chronic osteomyelitis. Cultures from this procedure remained negative, with the exception of one culture that was positive for Staphylococcus epidermidis on postoperative day five, which was believed to be a contaminant. The antibiotics were changed to sulfamethoxazole/trimethoprim and levofloxacin. The proximal tibial wound healed uneventfully, and the patient completed a six-month course of antibiotics. After this final debridement, he reported no additional symptoms and had returned to full activities, including motocross, at the time of the final follow-up seventeen months postoperatively. An evaluation for an underlying immunodeficiency was not pursued because he did not have a recurrent infection. The knee examination remained benign, but there was mild increased excursion with a firm end point compared with the Lachman examination on the contralateral side. There was no evidence of growth disturbance related to the transphyseal reconstruction (Fig. 6).
Proceed to Discussion >>Reference: Grantham WJ, Raynor MB, Martus JE. Articular Sinus Tract with Mycobacterium fortuitum Osteomyelitis After Anterior Cruciate Ligament Reconstruction: A Case Report. JBJS Case Connect 2015 Nov 25;5(4):e105.
Diagnosis of postoperative infection after ACLR may be difficult and is frequently missed, leading to delay in care. As such, adjunct laboratory tests and arthrocentesis should be used liberally in a patient who does not adhere to the standard postoperative course. Laboratory examinations should include a complete blood-cell count, ESR, and CRP level. Margheritini et al. demonstrated the normal postoperative decline of CRP level and ESR in the noninfected ACLR patient with an expected return to normal at fifteen and thirty days postoperation, respectively. Therefore, any patient with a persistently elevated CRP level beyond two weeks or an elevated ESR beyond one month should be suspected of having a postoperative infection. As stated above, arthrocentesis of the knee should be performed if there is suspicion of infection. Synovial fluid should be sent for analysis and include cell count with differential, crystal analysis, Gram stain, and culture. As observed in our patient, the synovial fluid nucleated cell count can often be low in the setting of postoperative infection. When this is the case, extra-articular infection should be suspected; the proximal part of the tibia is the most common site for extra-articular infection in this setting. Judd et al. demonstrated that the average cell count in the setting of intra-articular infection was 52,735 nucleated cells, whereas the average for an extra-articular infection was 1133 nucleated cells. The draining articular sinus from the tibial tunnel was perceived to be one of the barriers to clearing the mycobacterial osteomyelitis. The goal of the final procedure was to alleviate the draining sinus by closing off the tibial tunnel. The tunnel was debrided and packed with cancellous allograft mixed with tobramycin to produce high concentrations of local antibiotic. Other options such as iliac crest autograft could have been utilized to fill the tibial tunnel; however, this was avoided because of donor-site morbidity. Antibiotic-laden cement also could have been considered, although this would have been more difficult to remove if it became necessary as a result of persistent infection. This case represents a postoperative infection with an atypical organism that had a protracted treatment course despite early diagnosis. We recommend that all obtained cultures be held by the laboratory for at least two weeks and, as this report suggests, be tested for mycobacterial species as well. Additionally, mycobacterial osteomyelitis should be considered in any infection with a sinus tract or a prolonged course that requires multiple debridements. Our patient did not have complete resolution of the symptoms until the tibial tunnel was debrided with a high-speed burr and bone-grafted with antibiotic-laden allograft, a technique that, to the best of our knowledge, has not been reported in the literature for infection after ACLR but should be considered in this setting.
Reference: Grantham WJ, Raynor MB, Martus JE. Articular Sinus Tract with Mycobacterium fortuitum Osteomyelitis After Anterior Cruciate Ligament Reconstruction: A Case Report. JBJS Case Connect 2015 Nov 25;5(4):e105.
Viral synovitis
Pigmented villonodular synovitis
Staphylococcus epidermidis infection
Mycobacterial infection
Allergic reaction to the Bio-Interference screw

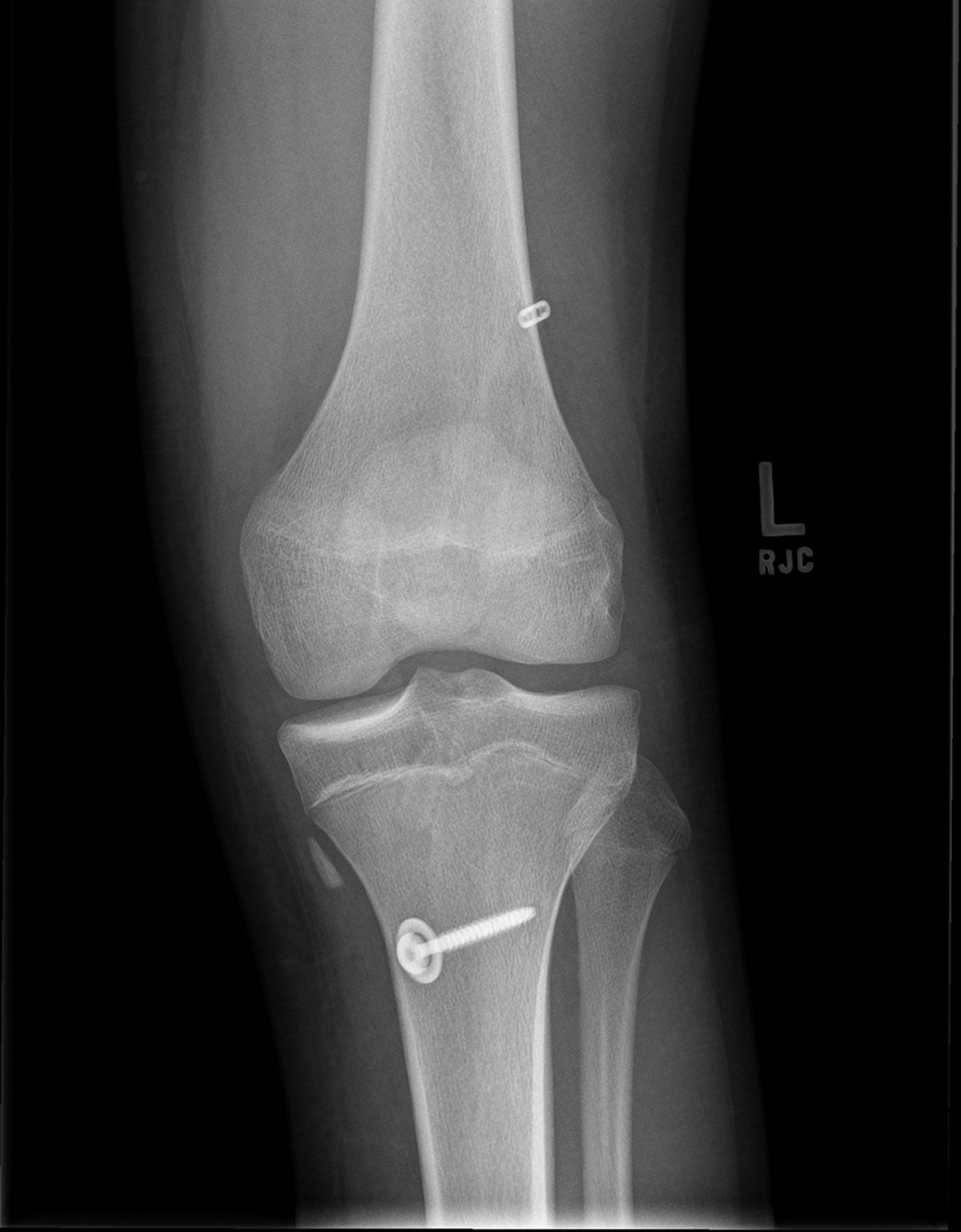
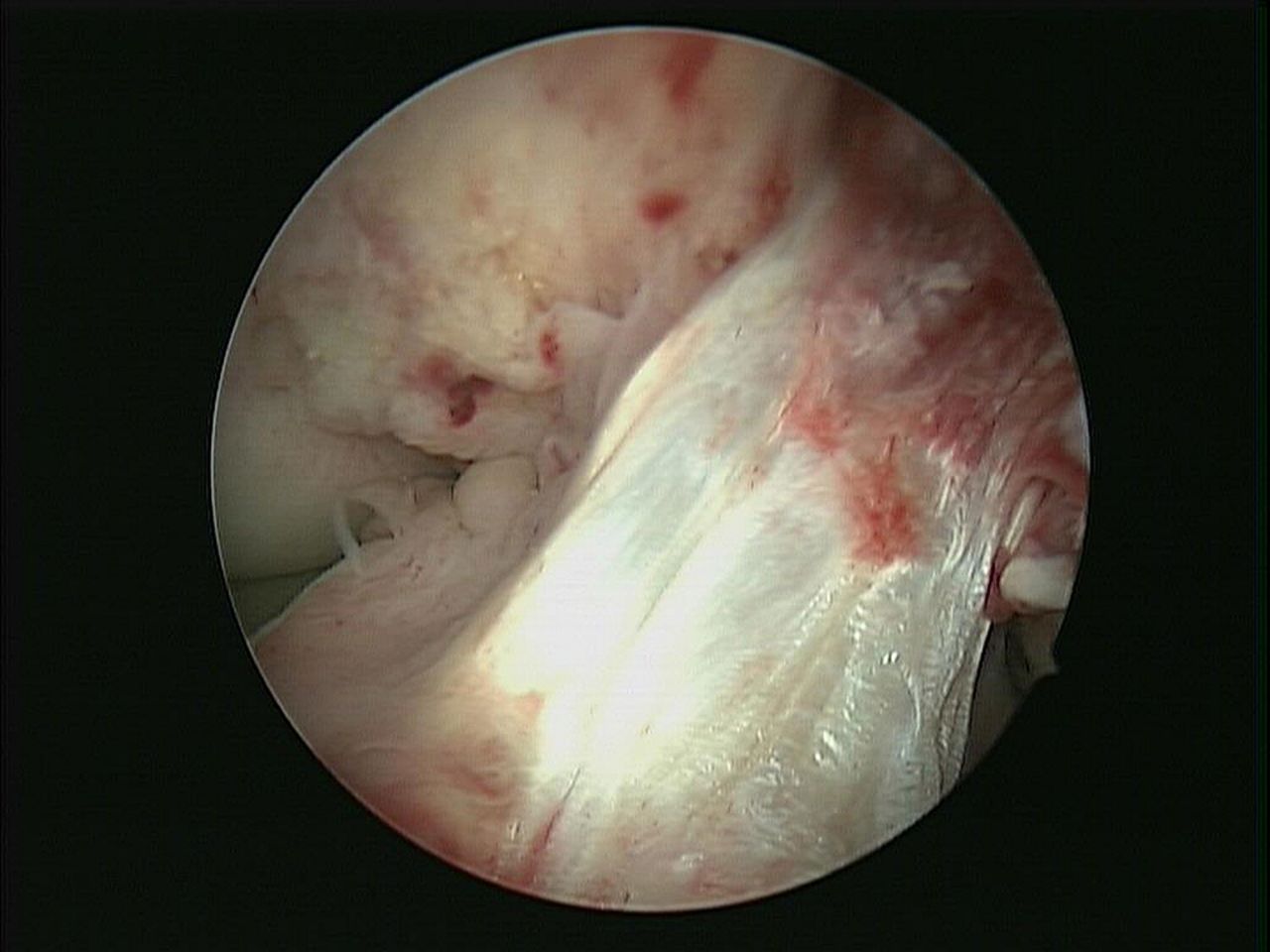

 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6

