Pain and Osseous Crepitus of the Knee Following a Fall Six Weeks After Anterior Cruciate Ligament Reconstruction
July 7, 2010
A forty-one-year-old man presented to our orthopaedic clinic with a history of chronic pain and instability of the right knee. The surgical history included an extra-articular MacIntosh-type reconstruction eighteen years earlier, which had been performed as treatment for a deficient anterior cruciate ligament. Hardware had been removed secondarily. The patient reported that after a satisfactory result for many years, increasing pain and instability slowly developed in the right knee, causing him to begin wearing a knee brace. The physical examination revealed a positive Lachman test, without an end point, and a painful positive pivot-shift test. Absence of the anterior cruciate ligament, grade-III chondromalacia of the lateral femoral condyle, and a posterolateral meniscal tear were documented on magnetic resonance imaging of the right knee. No screw-holes or bone defects from previous surgery were identified. The patient underwent reconstruction of the anterior cruciate ligament. Intraoperative procedures included a subtotal posterior horn meniscectomy plus an abrasion chondroplasty and microfracture for a small but severe area of chondromalacia of the lateral femoral condyle. A standard notchplasty was followed by arthroscopic anterior cruciate ligament reconstruction with use of bone-patellar tendon-bone allograft. A femoral tunnel (12 mm in diameter, 30 mm deep) was then made after placement of a guide pin at approximately the eleven o'clock position with a 7-mm offset guide. This left an intact 1-mm posterior cortex in the femoral tunnel. A 12-mm-long tibial tunnel was placed 7 mm anterior to the tibial insertion of the posterior cruciate ligament. A bone-patellar tendon-bone allograft (12 mm in diameter) was passed into the knee through the tibial tunnel and was fixed under tension. Femoral fixation with two 2.7-mm bioresorbable cross-pins (RIGIDfix; DePuy Mitek, Raynham, Massachusetts) was followed by tibial fixation with a bioresorbable 12-mm-diameter × 28-mm-long interference screw (DePuy Mitek). There were no intraoperative complications, and the patient was instructed to remain non-weight-bearing on crutches to protect the abrasion chondroplasty. Six weeks postoperatively, the patient reported losing his balance and falling while descending a short flight of stairs with the use of crutches. Examination in the emergency department revealed diffuse swelling in the right knee and painful osseous crepitus when the knee was flexed. A contusion was noted at the point of impact over the distal end of the medial femoral condyle. The neurologic and vascular examinations revealed normal results. Radiographs were made.
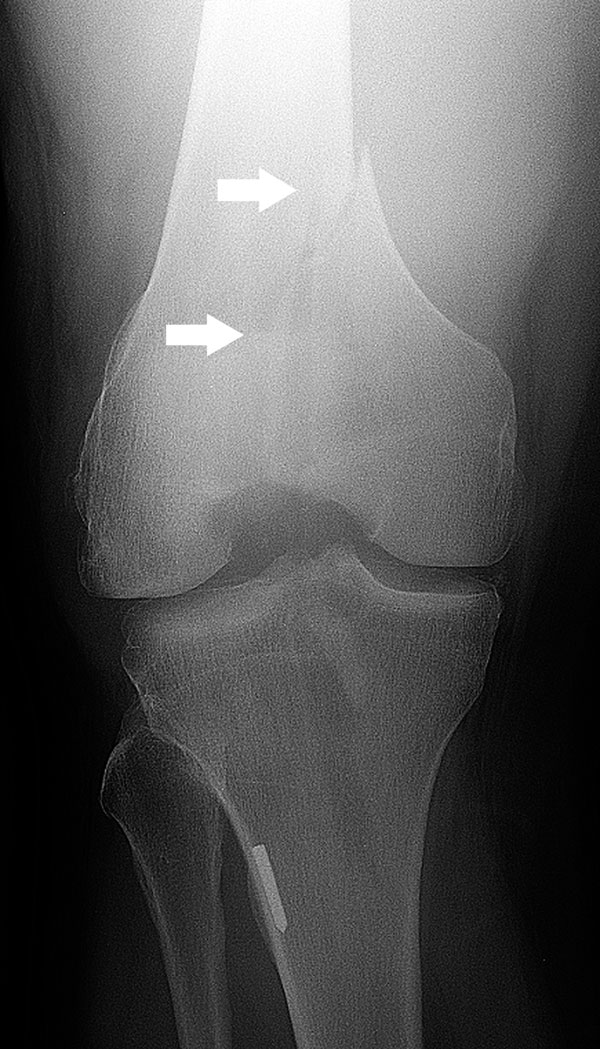
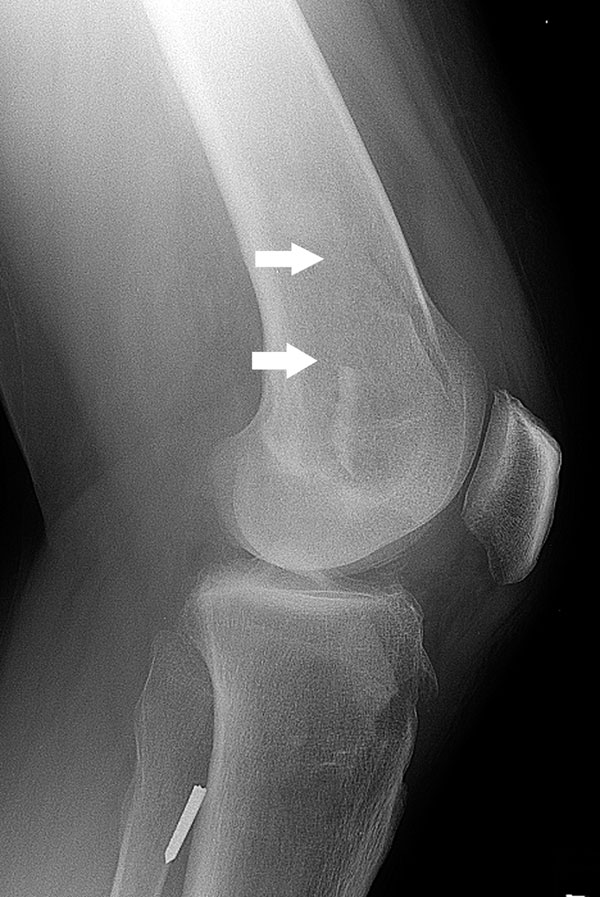
Radiographs revealed a displaced fracture (AO/OTA type-33-B2) of the medial condyle of the femur (Figs. 1-A and 1-B). Computed tomography showed the sagittal intracondylar fracture line exiting through the femoral bone tunnel (Fig. 2). No osteolysis was identified within the femoral tunnel, and no cross-pin fixation bone tunnels were identified. Treatment consisted of fluoroscopic navigation plus arthroscopically assisted closed anatomic reduction of the fracture and percutaneous fixation with four 7.3-mm-diameter cannulated screws and washers (Synthes, Paoli, Pennsylvania). The operative setup entailed both arthroscopic visualization and fluoroscopic navigation. The patient was placed in a supine position on a radiolucent table. The end of the table was removed to allow c-arm access and to facilitate manipulation of the extremity. Standard anterolateral and anteromedial arthroscopic portals were established. Arthroscopic lavage and debridement of the hematoma was followed by direct visualization and debridement of the fracture site prior to closed reduction. Longitudinal traction on the limb with the knee in mild flexion and with valgus manipulation allowed the medial femoral condylar fragment to be pulled into proper alignment with ligamentotaxis. Two 2.8-mm-diameter guidewires for the 7.3-mm-diameter cannulated screws were inserted percutaneously into the medial condylar fragment to manipulate it. With use of both guidewires (one in each hand), the proximal aspect of the medial condylar fragment was manipulated into its origin on the distal aspect of the femur and held in place. The distal body of the fragment was then reduced anatomically with the distally placed guidewire. Combined fluoroscopic and arthroscopic visualization of the fracture site confirmed an anatomic reduction. Provisional fixation of the reduction was then obtained as the 2.8-mm guidewires were driven across the fracture. Fracture-fragment compression was observed arthroscopically as the screws were tightened over the guidewires (Fig. 3), and anatomic reduction and fixation were confirmed radiographically (Figs. 4-A and 4-B). Arthroscopy also provided visualization of the intact anterior cruciate graft during intraoperative stability testing after reduction and fixation of the fracture. Both the Lachman test and stability testing with a nerve-hook probe demonstrated graft stability that was unchanged in comparison with the stability noted at the completion of the anterior cruciate ligament reconstruction. Postoperatively, the patient was at first restricted to non-weight-bearing on crutches and was then allowed to gradually begin range-of-motion and then strengthening exercises. Graduated weight-bearing was begun at six weeks. At twelve weeks after fracture repair (eighteen weeks after anterior cruciate reconstruction), the patient had achieved a full range of motion of 0° to 140°. He was bearing full weight, the KT-1000 arthrometer testing and Lachman tests were classified as grade A according to the system of the International Knee Documentation Committee, and the pivot-shift test was negative. At no time was posterior, varus, or valgus instability detected, and there was no subjective instability. Radiographs showed that the fracture had healed in excellent alignment.
Proceed to Discussion >>Reference: Montgomery CO, Evans RP. Arthroscopic reduction and internal fixation of a medial femoral condylar fracture after anterior cruciate ligament reconstruction. A case report. J Bone Joint Surg Am. 2008;90:863-8.
Periarticular fracture of the knee is an uncommon complication of anterior cruciate ligament reconstruction. To our knowledge as of the time of writing of the original case report, there were no reports of medial femoral condylar fracture after arthroscopically assisted anterior cruciate ligament reconstruction. In the patient highlighted in this Image Quiz, the impact force from the fall was directed to the medial side of the flexed knee, thus resulting in a fracture of the medial condyle through the femoral tunnel stress-riser. A review of the literature with regard to periarticular fracture of the knee after anterior cruciate ligament reconstruction revealed that most fractures are associated with trauma in association with an iatrogenic stress-riser. These stress-risers occur as a result of bone tunnels, autograft host defects, and cortical defects from extra-articular fixation. It has been shown that a drill-hole can elevate stress concentration and result in a fracture through the drill-hole. One report described a lateral femoral condylar fracture after anterior cruciate ligament reconstruction in which the femoral tunnel was overdrilled and violation of the lateral femoral cortex resulted in the creation of a stress-riser. Two other case reports described supracondylar and lateral femoral condylar fractures through femoral tunnel stress-risers. The four remaining distal femoral fractures (two lateral condylar fractures, one supracondylar fracture, and one distal femoral shaft fracture) occurred through a femoral tunnel stress-riser, an extra-articular fixation site for a prosthetic graft, an iliotibial tenodesis screw fixation site, or a ligament augmentation device site. The patient highlighted in this Image Quiz underwent bioresorbable 2.7-mm cross-pin fixation through the femoral tunnel and graft. The patient's physicians were not able to identify the cross-pin bone tunnels on the postinjury computed tomography scan. The femoral fracture exited through the inferior and medialmost aspect of the femoral tunnel and not through the cross-pin tunnels. Preoperatively, this patient's physicians did not find a distal medial femoral condylar plate designed for fixation of this fracture type. All condylar plates that were available at that time were contoured to fit the lateral femoral condyle. Although a T-buttress plate could have been bent into a modified shape in an attempt to contour it to the medial femoral condyle through an incision and arthrotomy, the patient's physicians chose to proceed with operative repair of the fracture with arthroscopically assisted closed reduction and percutaneous screw fixation. Case reports of this technique for lateral femoral fracture repair are rare. Its benefits include the enhanced ability of the surgeon to achieve an excellent intra-articular reduction and decreased blood loss. The minimal amount of soft-tissue dissection may lead to a more rapid postoperative recovery. Additionally, if difficulty is encountered with this technique, the surgeon still has the option of switching to the more standard procedure of open reduction and internal fixation. This less invasive technique can provide a good clinical result, and we believe it should be considered as one way to treat this type of intra-articular fracture.
Reference: Montgomery CO, Evans RP. Arthroscopic reduction and internal fixation of a medial femoral condylar fracture after anterior cruciate ligament reconstruction. A case report. J Bone Joint Surg Am. 2008;90:863-8.
infection of anterior cruciate ligament graft
distal femoral fracture at graft site
distal femoral fracture through early bone tumor


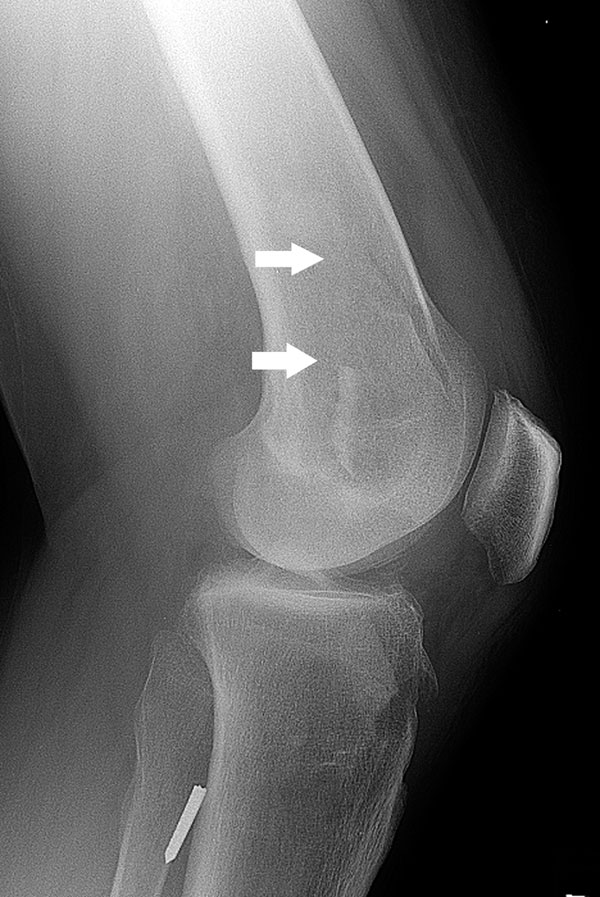
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B