A Sixty-one-Year-Old Man with Hypertension Experiencing Seizures Following a Surgical Procedure
February 17, 2016
The patient was a sixty-one-year-old man with a medical history pertinent only for hypertension and a five-year history of being a one-pack-per-day smoker. In 1996, he underwent resection of a mass from the medial aspect of his left thigh at an outside facility followed by radiation therapy. He originally presented to our facility in 2007 for follow-up visits for the thigh lesion that included yearly surveillance radiographs, which were not concerning for neoplastic disease at the site of the original lesion.
In June 2013, the patient had one episode of unprovoked seizure-like activity. The work-up included assessment for a possible cardiac etiology. Electrocardiography results were abnormal, and nuclear medicine scans demonstrated an anterior apical perfusion defect concerning for infarction. A coronary angiogram was notable for diminished flow in the left anterior descending coronary artery, and echocardiography demonstrated a possible mass in the left ventricle. Cardiac MRI (magnetic resonance imaging) was interpreted as showing a possible pseudoaneurysm of the apical area of the left ventricle as well as a pericardial effusion (Figs. 1 and 2).
On admission to our facility, the patient indicated that he had no chest pain or difficulty breathing, and he was hemodynamically stable. An echocardiogram was suggestive of a mass effect at the apex of the heart, consistent with a pseudoaneurysm. A CT (computed tomography) angiogram was notable for mild coronary artery calcification without occlusion and a 30 × 28-mm circular mass at the apex of the left ventricle, without extension into the right ventricle, which might have been due to a thrombus or neoplasm. A PET (positron emission tomography) scan did not show evidence of metastatic disease. At this point it was decided to take the patient to the operating suite to repair what was believed to be a pseudoaneurysm.
The pericardium was incised through a median sternotomy and, after a large serous pericardial effusion was evacuated, a large tumor was identified over the apical region and expanding into the anterior and lateral walls of the left ventricle. Multiple biopsies were taken and sent to the pathology facility for frozen and permanent sections. At this time, the surgical team discussed the case with an oncology consultant along with the patient’s family, who agreed with the decision to abort the current procedure in order to obtain final pathological results and reformulate a treatment plan.
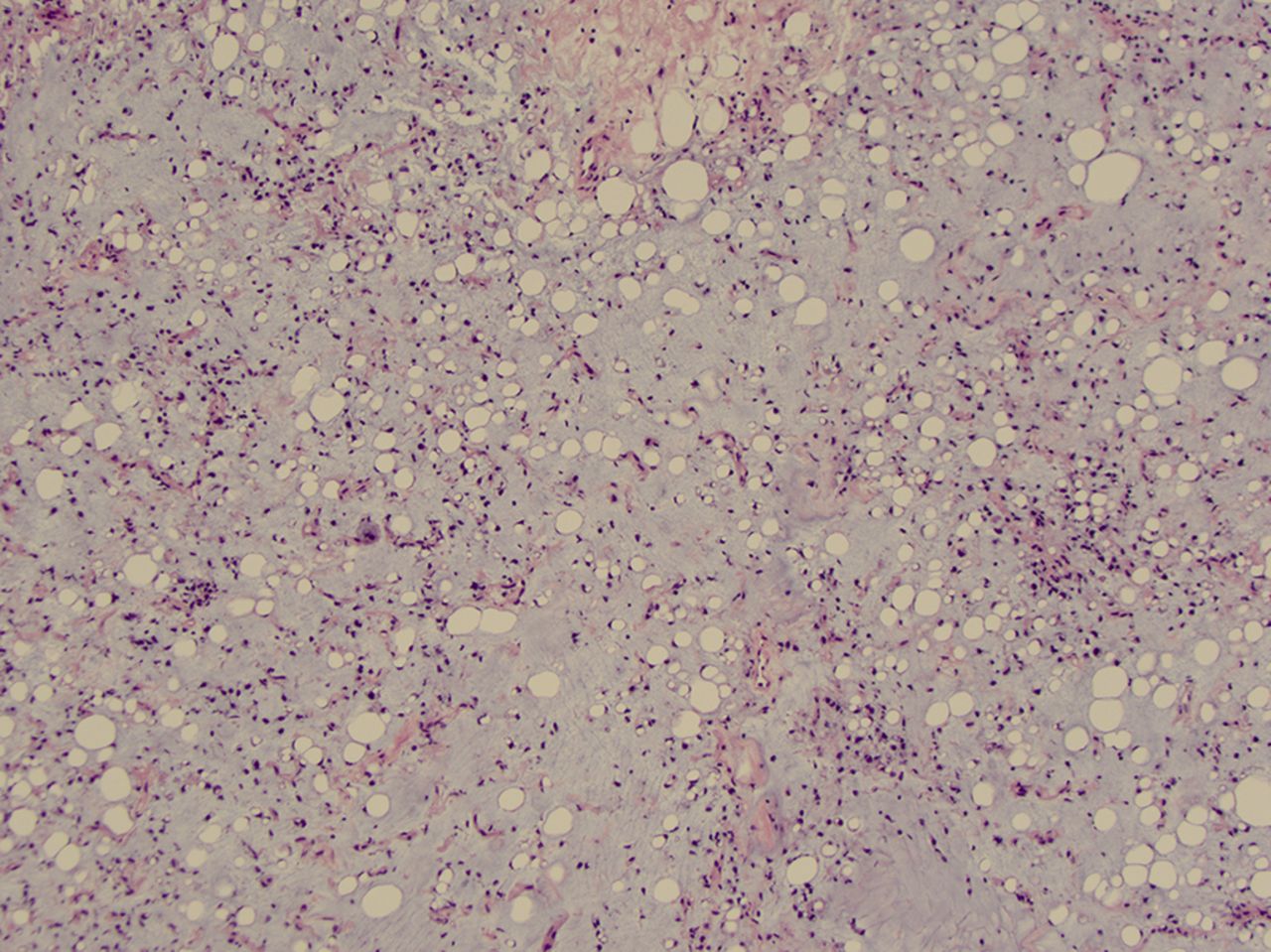
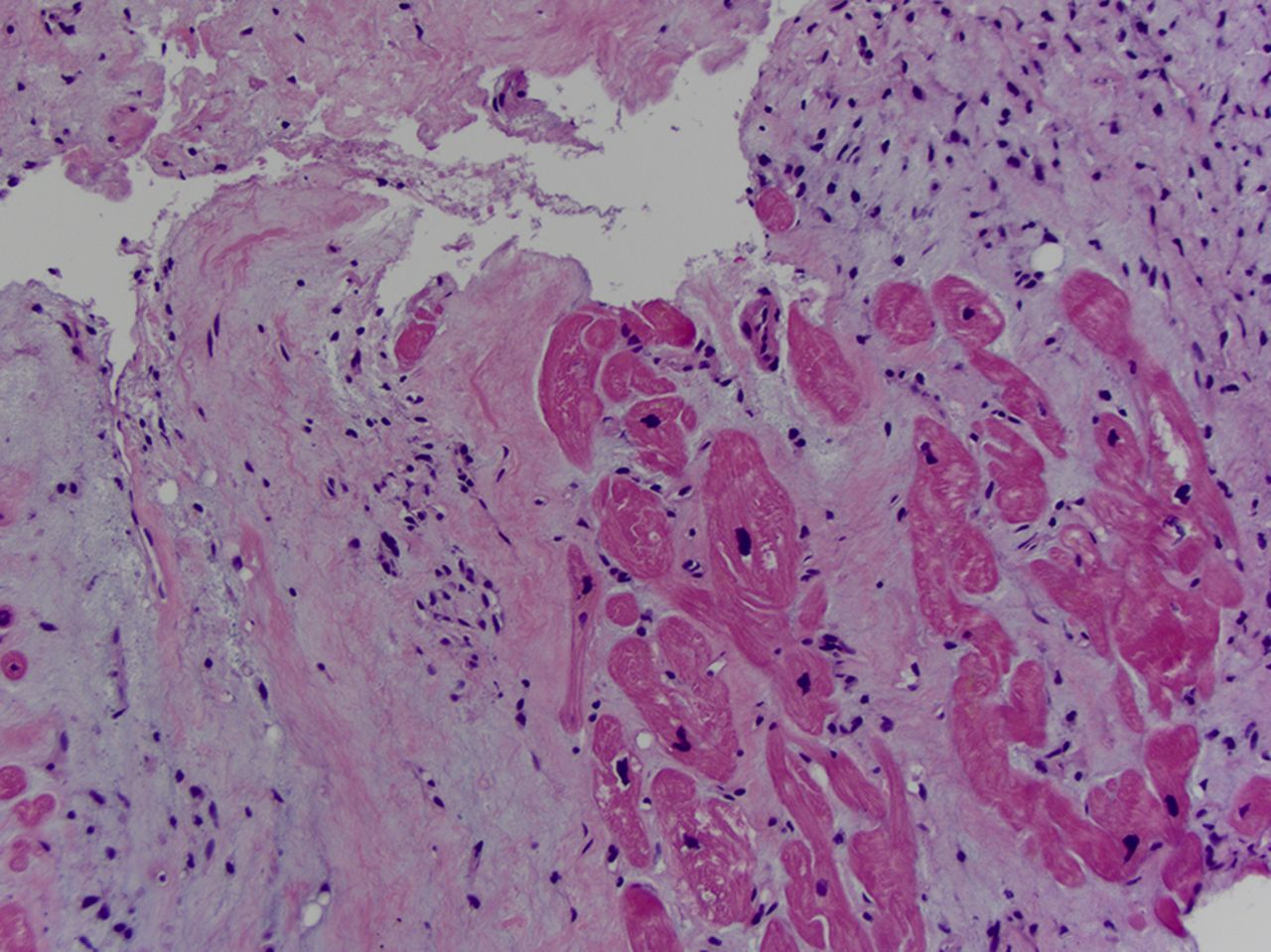
Final histopathological results (Figs. 3 and 4) of the intraoperative biopsy samples confirmed the diagnosis of low-grade myxoid liposarcoma with no evidence of round-cell differentiation or tumor necrosis. Cytogenetic analysis identified an FUS-DDIT3 genetic rearrangement, confirming the diagnosis of myxoid liposarcoma.
It was decided that the tumor was not amenable to resection and the patient was to be referred to the radiation oncology department for possible radiation therapy, but he died prior to the beginning of any therapy.
Proceed to Discussion >>Reference: Farmer RP, Schowinsky JT, Lindeque BGP. Myxoid liposarcoma of the thigh with metastasis to the left ventricle of the heart: A case report. JBJS Case Connect. 2015 Oct 28;5(4):e91.
Liposarcomas are the second most common soft-tissue sarcoma, with the myxoid subtype being among the most common subtypes. Prior to the World Health Organization (WHO) classification of 2013, myxoid liposarcoma included subtypes designated as myxoid and round-cell. The 2013 classification combined these two subtypes, as it has long been thought that they are not two distinct diseases but represent a spectrum of the same disease process, with low-grade myxoid liposarcomas containing ≤5% round cells and high-grade tumors containing >5% round cells.
As with most neoplastic diseases, it is very important to obtain biopsy tissue of myxoid liposarcoma lesions as histologic grading has prognostic implications. Histologically low-grade myxoid liposarcomas have a low risk of metastasis and a five-year survival rate of 90%, whereas high-grade tumors with a >5% round-cell component have a 60% five-year survival rate. The extent of necrosis is also strongly associated with the survival rate, with one study reporting tumors with >5% necrosis being associated with a ten-year survival rate of 0%.
Cytogenetically, myxoid liposarcoma is characterized by a reciprocal translocation of t(12:16) (q13:p11), which leads to the fusion of a translational regulator, TLS, and a transcription factor associated with cell cycle growth and arrest, CHOP. The TLS-CHOP fusion protein, also referred to as FUS-DDIT3, that is encoded by the translocation is a powerful transforming oncogene that appears to halt terminal differentiation of the cell and instead induces proliferation.
In contrast to most other sarcomas, myxoid liposarcoma has a predilection for metastases to other soft-tissue sites, especially fat-bearing areas such as the retroperitoneum, abdominal cavity, axilla, and contralateral limb. As far as we know, the present case report describes only the thirty-first reported case of metastasis of this tumor to the heart, and most previously reported patients have had widespread metastatic disease. Primary cardiac liposarcoma lesions are even rarer, representing only 1% of primary malignant cardiac tumors.
The prevalence of secondary malignant lesions of the heart has been reported to be almost forty times higher than the incidence of primary cardiac malignancies. The neoplastic lesions most likely to metastasize to the heart, in order of frequency, are melanoma, breast carcinoma, lung carcinoma, and lymphoma. Sarcomas have an estimated cardiac metastatic prevalence of roughly 0.6% as determined from an autopsy study of individuals with neoplastic disease. Based on the reported frequency of cardiac metastases compared with primary sarcomas, we interpret the present case as most likely a metastatic liposarcoma rather than a second primary tumor.
Current treatment for myxoid liposarcoma is local resection of the tumor with either adjuvant or neoadjuvant therapy using empiric chemotherapeutic agents, typically ifosfamide and doxorubicin, although other agents have been used with some success. Radiation therapy has also been shown to decrease the bulk of tumors and has been successfully used in palliation of cardiac metastases.
Reference: Farmer RP, Schowinsky JT, Lindeque BGP. Myxoid liposarcoma of the thigh with metastasis to the left ventricle of the heart: A case report. JBJS Case Connect. 2015 Oct 28;5(4):e91.
What is the diagnosis?
Metastatic osteogenic sarcoma
Primary myofibrosarcoma of the heart
Metastatic myxoid liposarcoma
Primary mesothelioma
Primary myosarcoma

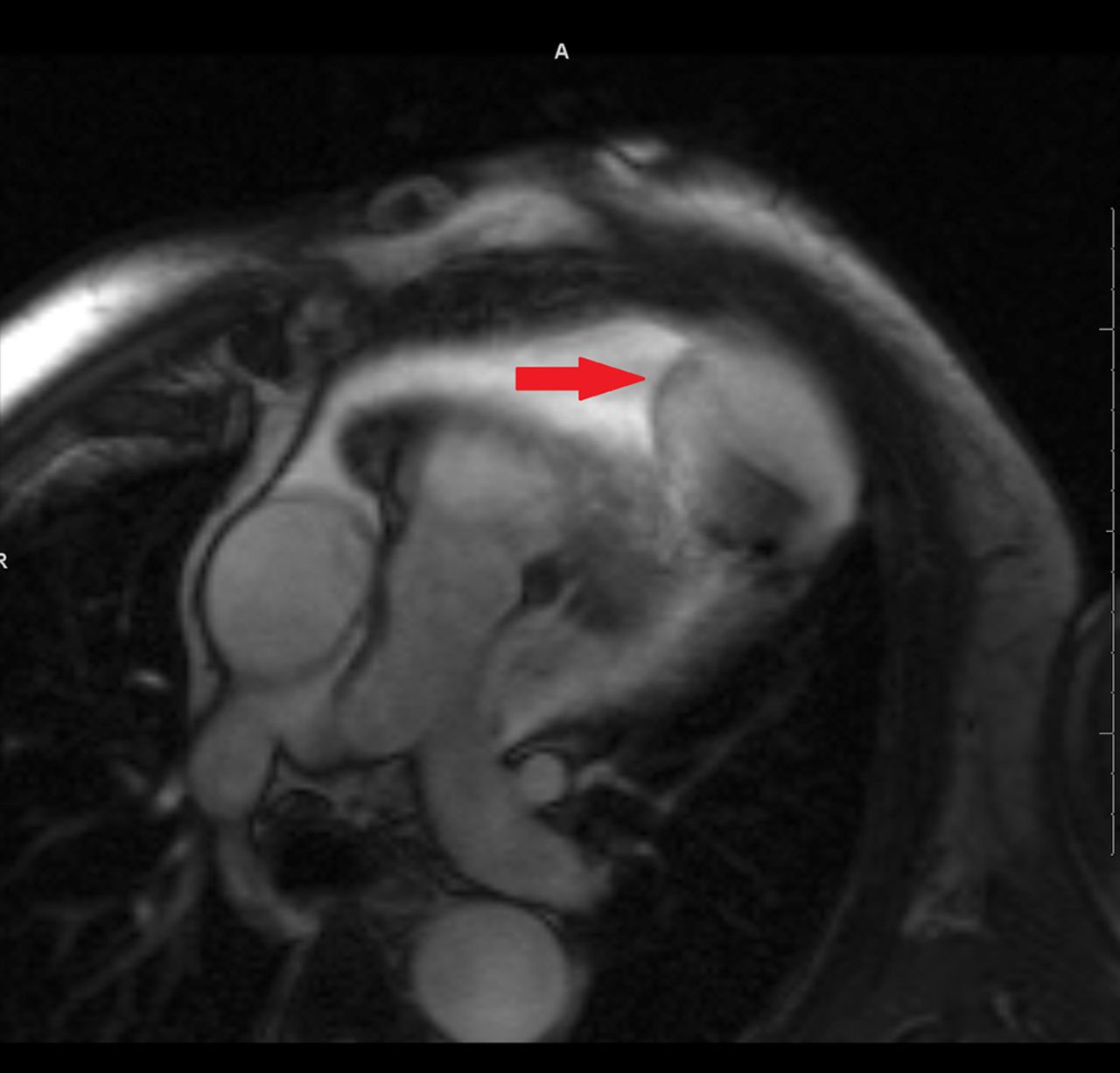
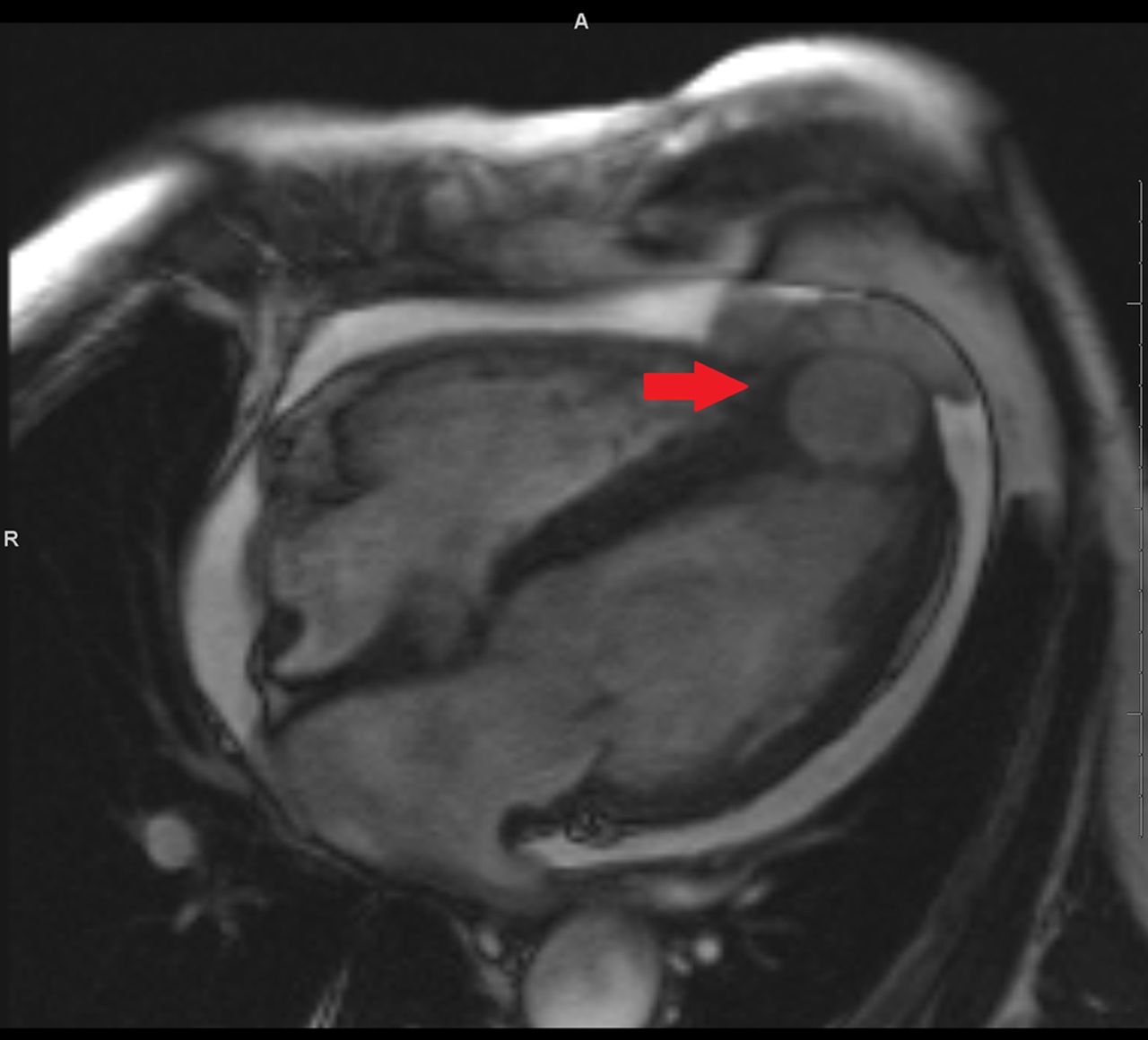
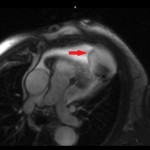 Fig. 1
Fig. 1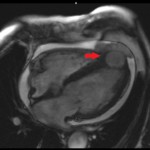 Fig. 2
Fig. 2 Fig. 3
Fig. 3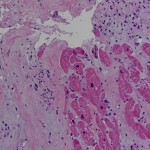 Fig. 4
Fig. 4