A 13-Year-Old Boy with a History of Back Pain
February 7, 2018
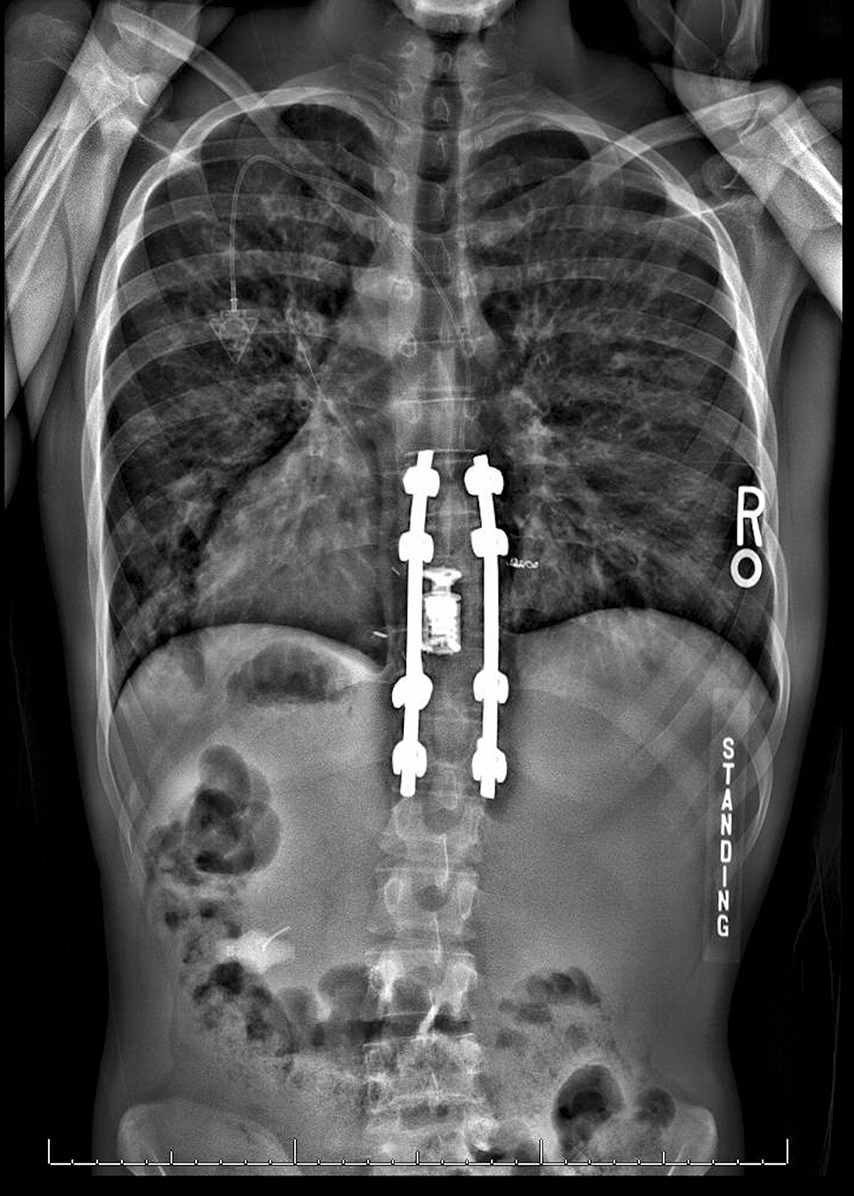
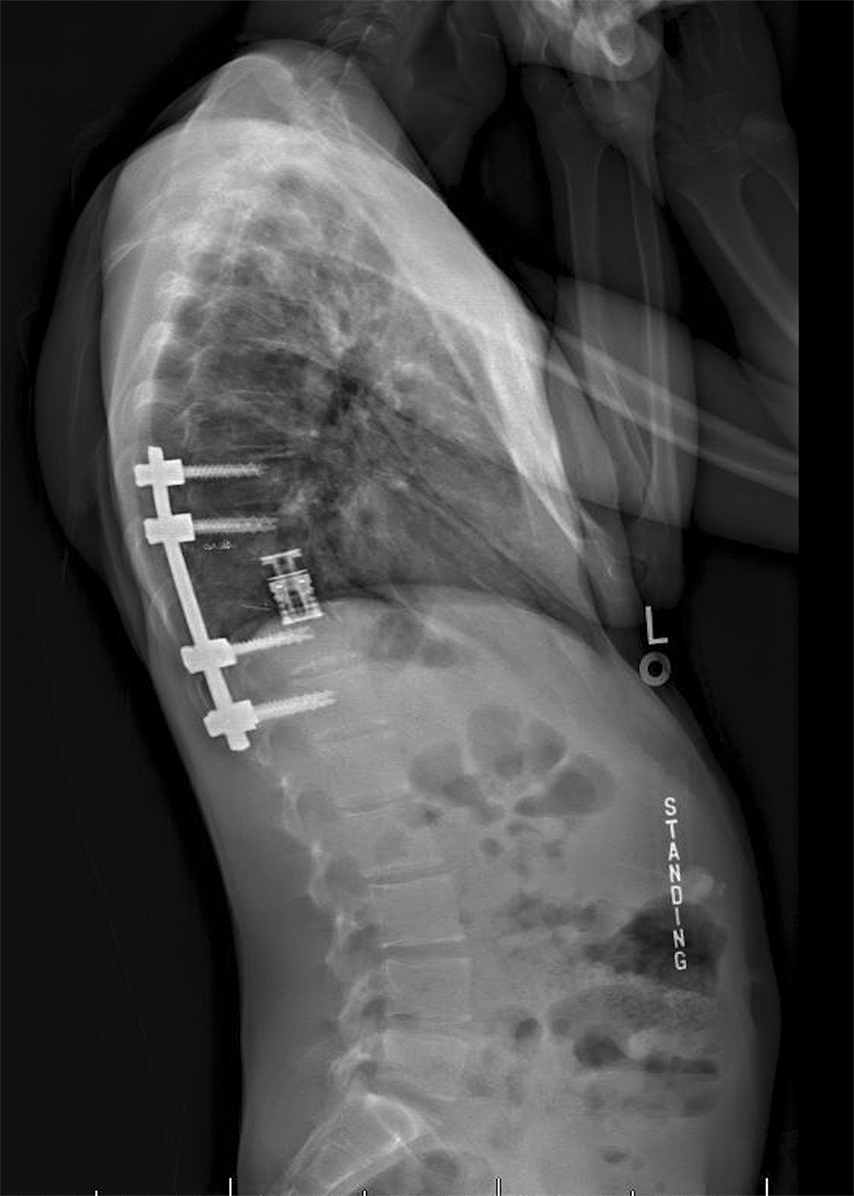
A 13-year-old boy presented with a 2-year history of mild back pain that did not interfere with daily activities. The neurologic examination was normal. Magnetic resonance imaging (MRI) (Figs. 1-A and 1-B) and computed tomography (CT) (Figs. 2-A and 2-B) showed features of an aggressive lesion at the T10 vertebra, with extraosseous extension and pathologic fracture.
The initial treatment was nonoperative because the tumor was stable and the patient had no substantial pain or neurologic symptoms. At a routine surveillance clinic visit, MRI showed expansion of the lesion with additional spinal canal compromise and cord compression (Figs. 3-A and 3-B).
We discussed the options of either no treatment and waiting for an adverse neurologic event or doing prophylactic surgical intervention with the patient and his family. They decided on surgery. The surgical plan included tumor embolization, stabilization, and a T10 vertebrectomy with spinal canal decompression, all done through a posterior approach.
On the day prior to the surgery, we performed a transarterial embolization (with Gelfoam [Cook Medical] and microcoils) of the right T9 and left T10 intercostal arteries. For the surgery, we used a posterior approach from T8 to T12; 4 pedicle screws were placed above and below the tumor, and a stabilizing rod was positioned on the right. The tenth rib on the left side was isolated, and a 2-cm segment was removed lateral to the T10 transverse process. The rib head was then detached from the lateral body of T10 and the transverse process in preparation for the anterior portion of the procedure. As we began the laminectomy, the posterior elements began to bleed profusely. At that time, because we were concerned that the embolization had not been adequate and we might not be able to control the bleeding through the costotransversectomy approach, we decided to convert the approach to a combined thoracotomy with a posterior approach. Fortunately, the tumor did not bleed much in the anterior body, where the embolization appeared to have been successful. The only bleeding that occurred was with the removal of the posterior elements. The entire T10 vertebral body was removed, leaving only a thin cortical shell on the right side. An expandable cage was inserted anteriorly between T9 and T11. A second stabilizing rod was added, and a fusion was accomplished using the resected rib as a bone graft to bridge the defect. The estimated blood loss was 950 cc. The histology of the lesion is shown in Figure 4.
The imaging features and histopathology are diagnostic of a vertebral hemangioma (VH).
At the first follow-up appointment, the patient was asymptomatic. At the most recent follow-up visit, 12 months after the surgery, he continued to do well, with no clinical or radiographic signs of recurrence (Figs. 5-A and 5-B).
Proceed to Discussion >>Reference: Gajaseni P, Labianca L, Lacerda I, Weinstein S. A child with a rare extraosseous extension and pathologic fracture from a vertebral hemangioma: a case report. JBJS Case Connect. 2017 Oct-Dec;7(4):e86.
A hemangioma is a hamartomatous proliferation of vascular tissue of endothelial origin. Most VHs are asymptomatic and do not require treatment. Some, however, may become aggressive and compress the spinal cord or nerve roots. These lesions must be treated aggressively. Laredo et al. proposed a 6-factor scoring system for compressive VHs, which was based, in part, on the imaging findings. These factors are location from T3 to T9, involvement of the entire vertebral body, involvement of the neural arch (pedicles), an expanded and poorly defined cortex, irregular trabeculation (honeycomb appearance), and soft-tissue swelling. A score with ≥3 of these factors suggests a compressive lesion that requires early treatment to avoid neurologic impairment. Laredo et al. and Friedman reported that this aggressive variant of VH shows a low T1-weighted MRI signal and a high T2-weighted MRI signal, whereas asymptomatic VH shows high signal on both T1 and T2-weighted MRI because of predominantly fatty stroma,. To the best of our knowledge, there are 7 previously reported cases of children with aggressive VH. Most of the patients were girls around the age of 13 years; the VH occurred between T3 and T9 and involved the spinal canal, causing neurologic deficits.
In aggressive VHs with extraosseous extension that causes spinal cord compression, total excision, including a tumor-free margin, is indicated. Decompression and vertebrectomy are the mainstays of treatment. Vertebroplasty and radiation therapy are adjunctive to surgery to obliterate the remaining tumor,. Because of a limited number of case reports, there is no scientific data to support the most appropriate treatment for aggressive VH. The surgical approach is determined by the location of the tumor and the site of compression. Costotransversectomy is an option for single-staged excision and circumferential fusion, particularly in patients who are poor candidates for transthoracic approaches. Chandra et al. reported a case series with costotransversectomy to achieve circumferential fusion for thoracic spinal pathologies (including 2 VHs). The mean spinal canal compromise was 59%, and the mean loss of vertebral height was 55% in this series. Improvement in functional status was gained by 76% of the patients. However, pneumonitis and pneumothorax were major complications.
With our patient, our original intention was to do the entire procedure through a posterior approach with an extrapleural costotransversectomy. However, because of substantial bleeding from the posterior elements, which made us question the effectiveness of the preoperative embolization, we chose to convert this to a combined anterior and posterior approach for a corpectomy and a fusion.
Because of the high vascularity of hemangiomas, copious intraoperative bleeding may lead to morbidity and mortality in the postoperative period, secondary to cardiopulmonary complications, as well as massive blood transfusions. Preoperative transarterial embolization of vessels feeding the hemangioma has been shown to decrease the intraoperative blood loss and the associated morbidity. Various substances have been used for embolization, including liquid embolic agents (e.g., Onyx; Micro Therapeutics), sclerosing agents (e.g., ethanol), particulate embolic agents (e.g., polyvinyl ethanol), and mechanical occlusion devices (e.g., coils). Transarterial embolization was associated with good neurologic recovery and no recurrence in 1 long-term follow-up. Robinson et al. described 51 cases in a systematic review and found that blood loss with embolization treatment (980 ± 683 mL) was lower than in the nonembolized control group (1,629 ± 946 mL).
Embolization is not the only factor contributing to reduction in bleeding. Kobayashi et al. reported on variables affecting intraoperative blood loss after embolization. The most important factor was the aggressiveness of the surgical procedure (p < 0.001). The meta-analysis by Robinson et al. strongly recommended embolization prior to surgery for aggressive VH. In addition to embolization, other important factors included surgical technique, anesthesia, and patient clotting parameters.
Our case points out the limitations of preoperative embolization. We presume that the excessive posterior-element bleeding in our patient was because the embolization had failed to access the vessels that supplied the tumor posteriorly. Early revascularization caused by the rapid enzymatic degradation of embolization agents also may be a factor. Other preoperative embolization techniques (e.g., triple-level embolization) may reduce intraoperative blood loss more effectively than single-level (at the level of the tumor) embolization for spinal tumors.
In conclusion, aggressive VHs are rare in children. This case report of an aggressive form of VH that caused pathologic fracture and spinal cord compression by the tumor emphasizes the importance of preoperative planning and having an appropriate back-up plan when preoperative embolization has not produced the desired effect.
Reference: Gajaseni P, Labianca L, Lacerda I, Weinstein S. A child with a rare extraosseous extension and pathologic fracture from a vertebral hemangioma: a case report. JBJS Case Connect. 2017 Oct-Dec;7(4):e86.
What is the diagnosis?
Telangiectatic osteosarcoma
Vertebral hemangioma
Aneurysmal bone cyst
Chondroblastoma with secondary aneurysmal bone cyst
Epithelioid hemangioendothelioma

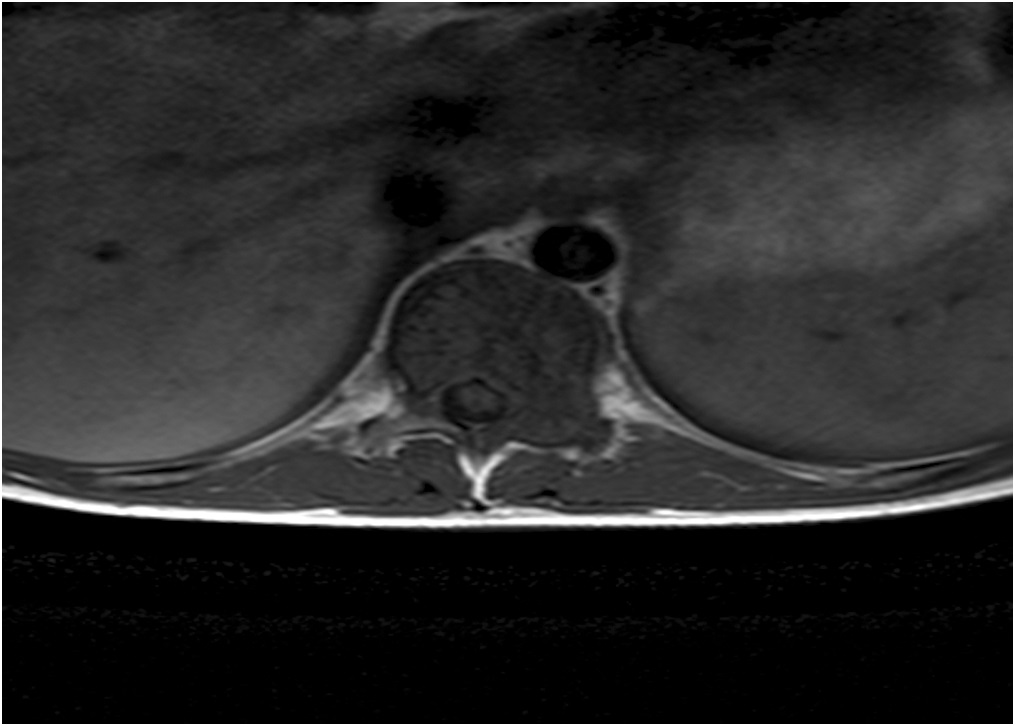

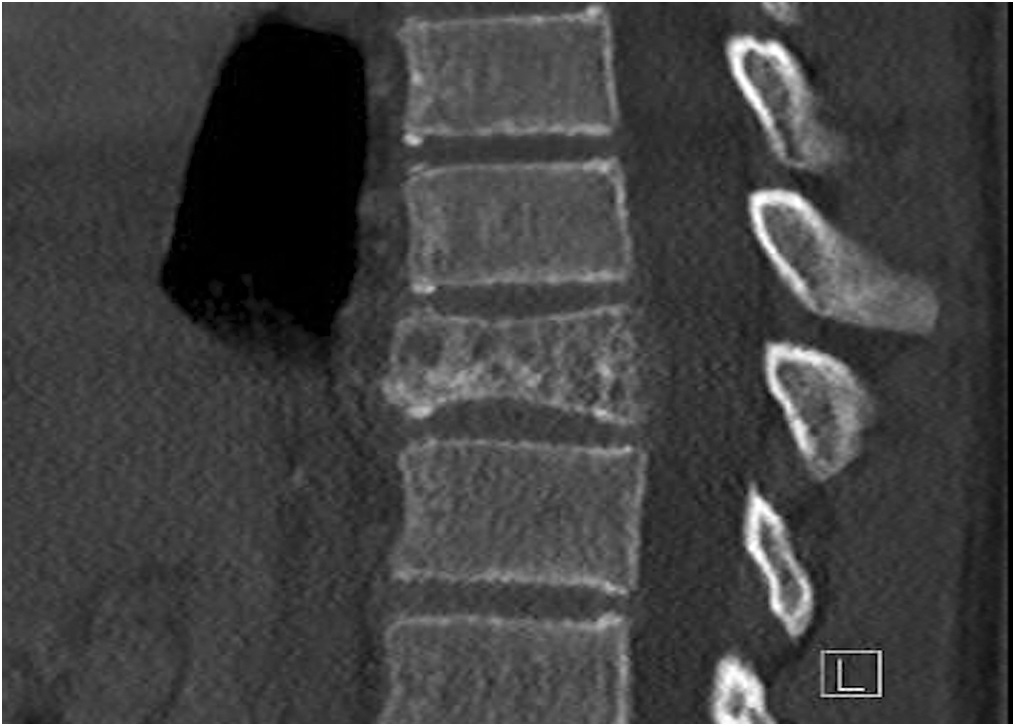
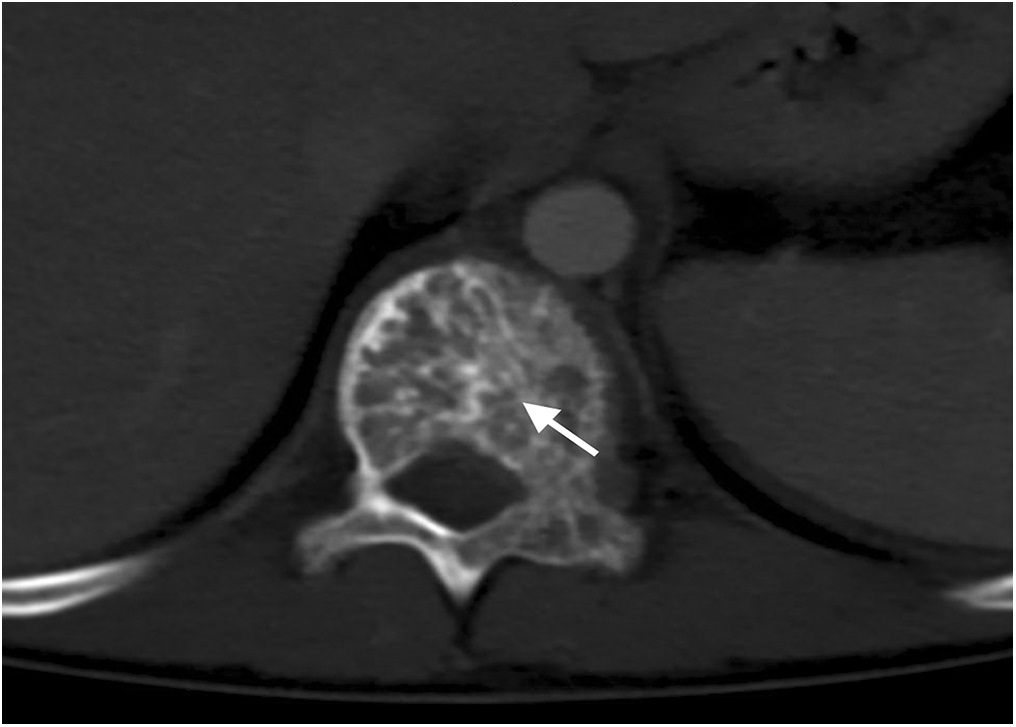

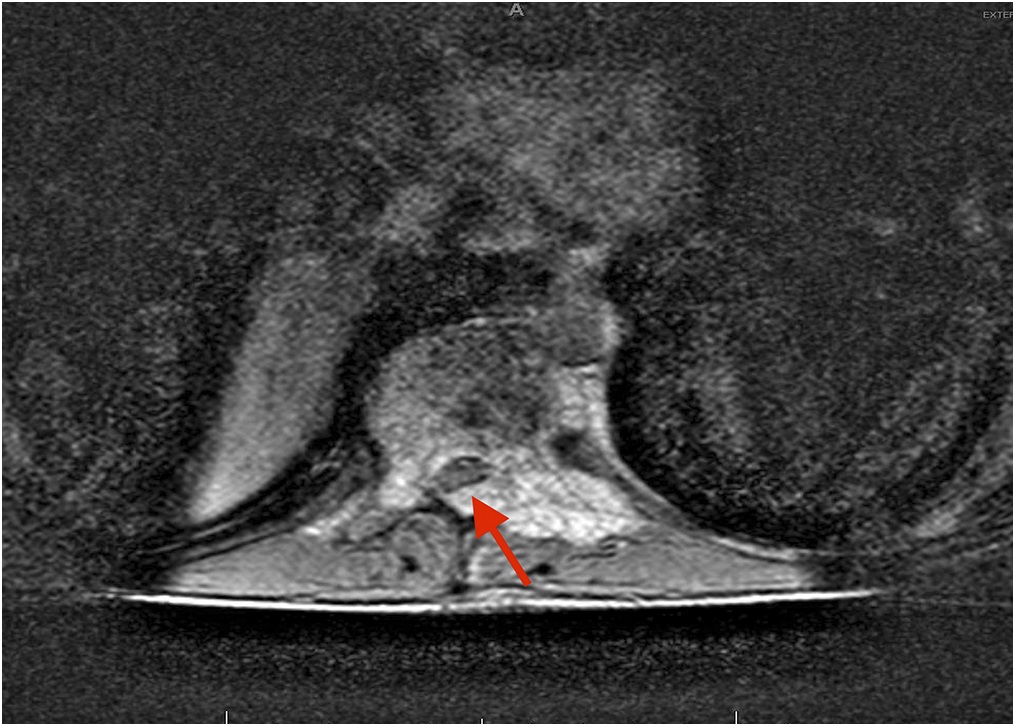

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B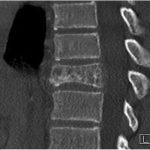 Fig. 2-A
Fig. 2-A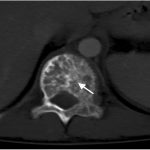 Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A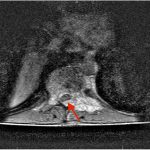 Fig. 3-B
Fig. 3-B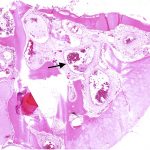 Fig. 4
Fig. 4 Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B