A 52-Year-Old Man with Thigh Pain Following an Accident
February 21, 2018
A 52-year-old man was seen in the office with the chief symptom of 1 year of left thigh pain, which had begun after a motor-vehicle accident. He noted the sensation of a “pop” in the thigh at the time of the accident. Five years earlier, the patient had undergone a total hip arthroplasty of the affected limb. After the total hip arthroplasty and prior to the accident, he had returned to work as a law enforcement officer and had participated in recreational sports. After the accident, he had noted vague left thigh pain with ambulation, which had been worsening over time.
Compared with the preinjury radiographs that showed calcar atrophy without subsidence or pedestal formation, indicating osseointegration, radiographs made in the office after the accident demonstrated subsidence of the implant, as well as an abnormality along the implant itself (Figs. 1-A and 1-B). Mild osteolysis also was noted. Laboratory investigation revealed an erythrocyte sedimentation rate of 17 mm/hr (normal, 0-15 mm/hr) and a C-reactive protein level of 3.1 mg/L (normal, 0-5 mg/L).
Given the clinical and imaging findings, revision surgery was recommended. An extended trochanteric osteotomy was required. At 2 years after the surgery, the patient was radiographically healed with well-fixed implants (Fig. 1-C), was walking without pain, and was participating in athletics.
Based on the imaging findings and the appearance of the implant, our diagnosis was delamination at the interface between the PEEK coating and the CoCr core of the implant. The delamination was believed to have led to loosening of the stem and thigh pain.
The patient’s implant was an Epoch femoral stem (Zimmer), composed of a CoCr core surrounded by a layer of radiolucent PEEK polymer, and a surface ingrowth coating of titanium fiber metal. The tip of the Epoch stem is part of the inner CoCr core, and it has a diameter larger than the fiber metal-PEEK coating, thus preventing removal of the inner-core stem from the proximal end of the femur and requiring an extended trochanteric osteotomy.
Upon implant removal after the accident at 63.3 months in vivo, the femoral stem was sent to an institutional review board-approved retrieval center for analysis. Investigation revealed that approximately 50% (by length) of the original composite material was still bonded to the inner core. The proximal aspect of the ingrowth surface remained on the stem and appeared calcified and well distributed and showed evidence of bone ingrowth into the fiber mesh (Fig. 2). The distal portion of the implant showed damage patterns consistent with single-event contact and motion-induced burnishing.
A number of “islands” of adherent PEEK remained, although the CoCr core was predominantly devoid of PEEK polymer material. The burnished appearance ran the length of the exposed CoCr core on the lateral aspect of the stem, and was present in 1 to 2-cm regions on the anterior, posterior, and medial aspects of the stem.
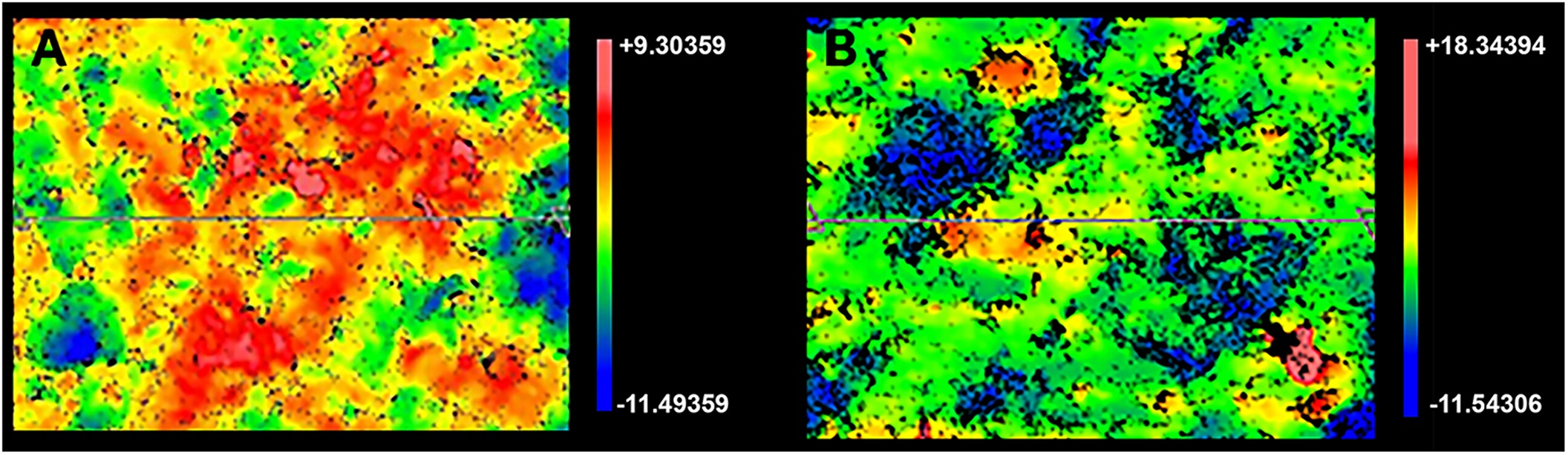
A portion of the PEEK-titanium composite was cut from the remaining surface for imaging of the PEEK-CoCr interface. The CoCr substrate demonstrated an as-manufactured matte finish, with a roughness average of approximately 2.4 μm. The opposing PEEK surface had a matte finish with a roughness average of approximately 1.7 μm (Fig. 3). These values suggest that the PEEK material interfaced closely with the CoCr core, but the 2 were not perfectly interdigitated.
Proceed to Discussion >>Reference: Bartelstein MK, Van Citters DW, Weiser MC, Moucha CS. Failure of polyaryletheretherketone-cobalt-chromium composite femoral stem due to coating separation and subsidence: a case report. JBJS Case Connect. 2017 Oct-Dec;7(4):e83.
This case demonstrates a rare mode of failure of this extensively porous-coated composite femoral stem; to our knowledge, this mode of failure is not well documented in the literature.
In several studies, patients with the Epoch stem demonstrated less bone loss than those with more rigid, noncomposite stems, as anticipated by its designers. It also has demonstrated a strong track record in several studies, detailing short-term and midterm success regarding stability and longevity. A retrospective study demonstrated secure implant fixation and maintenance of periprosthetic bone on radiographs at the 10-year follow-up. Other reports have demonstrated improvement in Harris hip scores without signs of implant migration at the time of follow-up,. Finally, a prospective, randomized study comparing the Epoch stem with a traditional fully porous-coated diaphyseal-engaging stem demonstrated excellent primary fixation of the Epoch stem, with fewer sclerotic lines compared with the traditional stem (p < 0.002).
PEEK, at body temperature, is below its glass transition temperature, where changes in the static and fatigue properties are negligible. Thus, in our patient, it is unlikely that the PEEK-titanium composite fractured in vivo during normal use. We hypothesize that the energy imparted on the stem during the motor-vehicle accident caused a disruption of the interface between the PEEK layer and the CoCr core of the Epoch implant. If the distal aspect of the stem had better fixation than the proximal aspect, collapse of the implant into the metaphysis would be possible with fracture of the PEEK layer.
Following impact-related subsidence of the implant, pistoning of the femoral stem inside the distally fixed PEEK results in motion between the polymer and the metal. PEEK in this form is not designed to be an articulating surface, and if it moves relative to the rough cobalt substrate, it might be subject to high wear rates and resulting particle generation. To cause osteolysis, these particles would need to migrate out of the PEEK-CoCr interface and into the surrounding bone. Since the PEEK was no longer bonded to the substrate, it is possible that submicron-sized wear particles could be transported distally along the stem and deposited in the medullary cavity.
To our knowledge, there are no other reports in the literature of noninfectious delamination of the PEEK from the CoCr core. One report details 2 cases of loosening due to delamination at this interface, but in the context of chronic infection. In that report, the fiber-mesh layer demonstrated excellent osseous ingrowth at the time of revision, and the PEEK had delaminated from the CoCr core. High-resolution microscopy of the explanted stem showed evidence of relative motion with the PEEK material, indicative of debonding of the PEEK-metal interface. Saltzman et al. hypothesized that infection caused an alteration of the local environment as well as debris formation, leading to delamination, which is a different mechanism from the high-energy impact event with our patient.
The Food and Drug Administration’s Manufacturer and User Device Experience (MAUDE) database was consulted for any reported evidence of Epoch stem failure that required implant revision with a mechanism of failure similar to that described in this case report. Three such occurrences were identified; 2 of the 3 involved the PEEK layer debonding from the CoCr core in the setting of periprosthetic infection. The third report was extremely vague, but noted that the PEEK layer had debonded from the CoCr core in the setting of an unspecified injury, requiring revision of the stem.
In conclusion, this report details an uncommon mode of failure for the Epoch stem, and highlights features that may be responsible for pain and loosening in patients with this femoral component. These features are important to recognize and understand in a patient with this type of implant.
Reference: Bartelstein MK, Van Citters DW, Weiser MC, Moucha CS. Failure of polyaryletheretherketone-cobalt-chromium composite femoral stem due to coating separation and subsidence: a case report. JBJS Case Connect. 2017 Oct-Dec;7(4):e83.
What is the diagnosis?
Osteolysis induced by particles of polyaryletheretherketone (PEEK)
Periprosthetic infection
Periprosthetic fracture
Paget disease associated with aseptic loosening
Delamination of the PEEK coating from the inner cobalt-chromium (CoCr) of the femoral stem

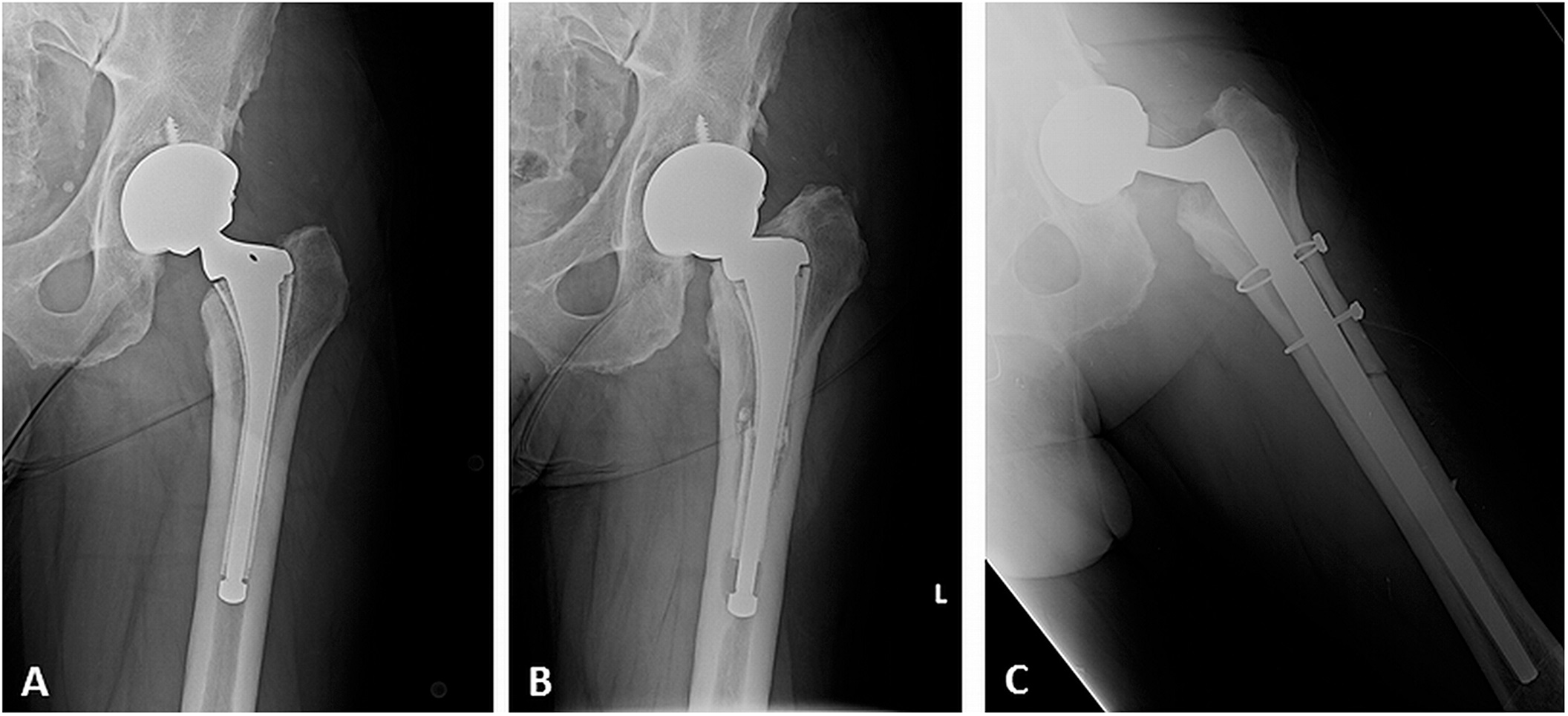
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3