A 16-Year-Old Boy with Pain in the Right Shoulder
March 15, 2017
A 16-year-old male Major League Baseball (MLB) prospect playing on a high school baseball team with no noteworthy medical history or previous trauma presented with pain in the right throwing shoulder at the time of the initial evaluation. The patient was restricted from throwing and underwent therapy to improve range of motion and throwing mechanics. Despite these treatments, he reported persistent pain in the posterior aspect of the shoulder when attempting to throw, as well as the inability to throw a baseball more than 90 ft (27 m) without experiencing a pain level of 9 of 10. He did not report any feeling of shoulder instability or past dislocations. On physical examination and in comparison with the contralateral side, he had an internal rotation deficit of 35° in the affected shoulder with otherwise normal range of motion, and strength was 5 of 5 in all planes of motion. Provocative tests for instability were all negative. The right upper extremity was neurovascularly intact.
Radiographs of the right shoulder demonstrated no osseous abnormality. The glenohumeral joint space was well preserved, and the humeral head was well reduced in the glenoid fossa (Fig. 1). Magnetic resonance imaging (MRI) of the right shoulder showed a 1.7 × 1.9-cm lesion with associated subchondral bone irregularity of the central and posterior margins of the glenoid (Fig. 2). The lesion encompassed approximately 40% of the glenoid articular surface.
The patient was diagnosed with osteochondritis dissecans (OCD). The patient was instructed to immediately cease all throwing activities. At this time, physical therapy was prescribed, concentrating on posterior capsular stretching. A progressive throwing program was initiated after shoulder mechanics and range of motion had been addressed. This 21-stage throwing program consists of a progressive increase in duration, distance, and velocity of throwing; the athlete advances from each stage based on any symptoms.
The patient returned to our office with improvement in symptoms and range of motion, and a follow-up MRI arthrogram was ordered to evaluate the glenoid lesion. The arthrogram, which was performed 8 months after the initiation of nonoperative treatment, showed an interval decrease in edema and irregularity within the lesion of the central and posterior margins of the glenoid, suggesting a healed OCD lesion (Fig. 3). No discrete chondral defect was noted in the glenoid or humeral articular surfaces. He was able to return to play after completion of the throwing program, and was drafted in the first round of the 2015 MLB draft. As of the 2016 season, he has been on the starting lineup of a U.S. Minor League Single-A club. At the 2-year follow-up, the patient reported no symptoms with throwing and has maintained range of motion in the shoulder.
Proceed to Discussion >>Reference: Grau LC, Jose J, Sama AJ, Baraga, MG. Osteochondritis dissecans of the glenoid in a Major League Baseball prospect: a case report. JBJS Case Connect. 2016 Dec 28;6(4):e100.
Koike et al. described the case of a 27-year-old professional baseball player with glenohumeral internal rotation deficit (GIRD) and a painful throwing shoulder who had an unstable, large 1.2 × 1.5-cm OCD lesion of the posterosuperior aspect of the glenoid, which was found on MRI. The authors reported that the patient had a trial of physical therapy that was unsuccessful at improving the pain and the catching symptoms. Follow-up diagnostic arthroscopy confirmed a 1.2 × 1.5-cm loose flap of articular cartilage in the 7:00 to 11:00 position of the glenoid, as well as an intra-articular loose body. The flap was debrided, the loose body was excised, and microfracture was performed in the area of the glenoid, which was devoid of all cartilage. At the time of follow-up, the patient had substantial improvement in pain and range of motion, and he was able to return to play. The authors proposed that repetitive microtrauma and shear forces on the posterosuperior aspect of the glenoid from the overhead-throwing motion, especially in the late cocking phase, were likely exacerbated by GIRD and predisposed the patient to developing the lesion.
In an attempt to revascularize subchondral bone and promote healing of a loose chondral flap, drilling of the subchondral bone arthroscopically has been reported as a surgical treatment option. Edmonds and Heyworth reported a case of OCD of the glenoid in a 15-year-old softball player with an associated tear of the posterior part of the labrum, as seen on MRI. Nonoperative treatment with physical therapy was unsuccessful, and arthroscopic evaluation revealed an unstable, large chondral flap, which corresponded to the lesion seen on MRI. After drilling of the subchondral bone where the cartilage was detached, the lesion was arthroscopically anchored down with the suture anchors that were used to repair the posterior part of the labrum. The authors reported that the patient had improvement of pain at the time of follow-up and was ultimately able to return to play at the collegiate level.
Other cases of OCD lesions involving the glenoid have also shown satisfactory results at the time of follow-up after arthroscopic debridement of unstable cartilage flaps with microfracture of subchondral bone; these cases have given insight into the etiology of these lesions. Gogus and Ozturk reported the case of a patient with a 0.5 × 0.5 × 1-cm lesion of the glenoid with sclerotic borders and a subchondral cyst, which was found on MRI; physical therapy had failed to relieve mechanical symptoms and pain in this patient. Diagnostic arthroscopy revealed complete loss of cartilage over the affected area, with a sclerotic rim circumscribing the lesion, as well as loose bodies in the joint. The authors proposed that repetitive trauma to the affected area leads to shearing of articular cartilage, which allows synovial fluid to become trapped between subchondral bone and cartilage, and the formation of subchondral cysts, which prevents healing and promotes cartilage detachment. Moreover, they suggested that trauma to the subchondral bone causes devascularization and necrosis, which then leads to bone reabsorption and detachment of the associated cartilage.
Our patient’s mechanism of injury is similar to that described by Koike et al.: both patients had an internal rotation deficit. Stretching of the anterior capsule and tightening of the posterior capsule has been proposed as a mechanism for posterosuperior migration of the humeral head on the glenoid fossa. These adaptive yet pathological changes in the shoulder may place greater than normal shear forces on the cartilage and subchondral bone of the posterior part of the glenoid. In the previously reported cases of OCD of the glenoid in throwing athletes, the lesions have occurred in the posterosuperior aspect of the glenoid fossa. Whether necrosis of the subchondral bone leads to detachment from the overlying cartilage when dead bone is reabsorbed, shear stress on cartilage leads to creation of a flap, or a combination of these factors occurs has not been determined.
Our case is unique in that this patient was successfully treated with physical therapy, while those reported in the literature had subsequent surgery. In all of the aforementioned cases, patients have had near-complete or complete detachment of the cartilage flap. Physical therapy may have been unsuccessful in these cases because synovial fluid between the subchondral bone and the cartilage flap, or detachment, prevents healing of the lesion, as was suggested by Nishinaka et al. In our patient, the apparently stable lesion was in a position favorable for healing, and an MRI arthrogram showed no contrast between the cartilage and subchondral bone. Discontinuation of play and physical therapy focusing on addressing our patient’s GIRD likely helped improve the posterosuperior migration of the humeral head on the glenoid, and subsequently decreased shear forces enough to allow for healing of the lesion.
This case provides insight into the etiology of OCD of the glenoid in overhead-throwing athletes. Our experience suggests that initial nonoperative treatment is reasonable in an overhead-throwing athlete with a stable lesion and GIRD, regardless of patient age or chronicity of symptoms, as long as the patient is followed closely radiographically and for changes in symptoms. The lesion healed in our patient, and he was able to return to play at a high level. We believe that if the inciting repetitive trauma of throwing is removed and the shoulder mechanics are improved with physical therapy, a favorable outcome is possible in the setting of a stable lesion, even in elite athletes. We suggest that stable lesions in overhead-throwing athletes initially be treated nonoperatively by discontinuing throwing and undergoing physical therapy to improve shoulder mechanics, especially GIRD. We elected for a follow-up MRI arthrogram prior to return to play to evaluate for healing after the patient had improvement of symptoms and the GIRD had been addressed because, to our knowledge, no prior studies have described successful nonoperative management. Imaging and clinical findings should be correlated when making a final treatment decision.
Reference: Grau LC, Jose J, Sama AJ, Baraga, MG. Osteochondritis dissecans of the glenoid in a Major League Baseball prospect: a case report. JBJS Case Connect. 2016 Dec 28;6(4):e100.
What is the diagnosis?
Osteocartilaginous loose body
Osteochondritis dissecans
Bizarre parosteal osteochondromatous proliferation (Nora lesion)
Osteochondroma
Enchondroma


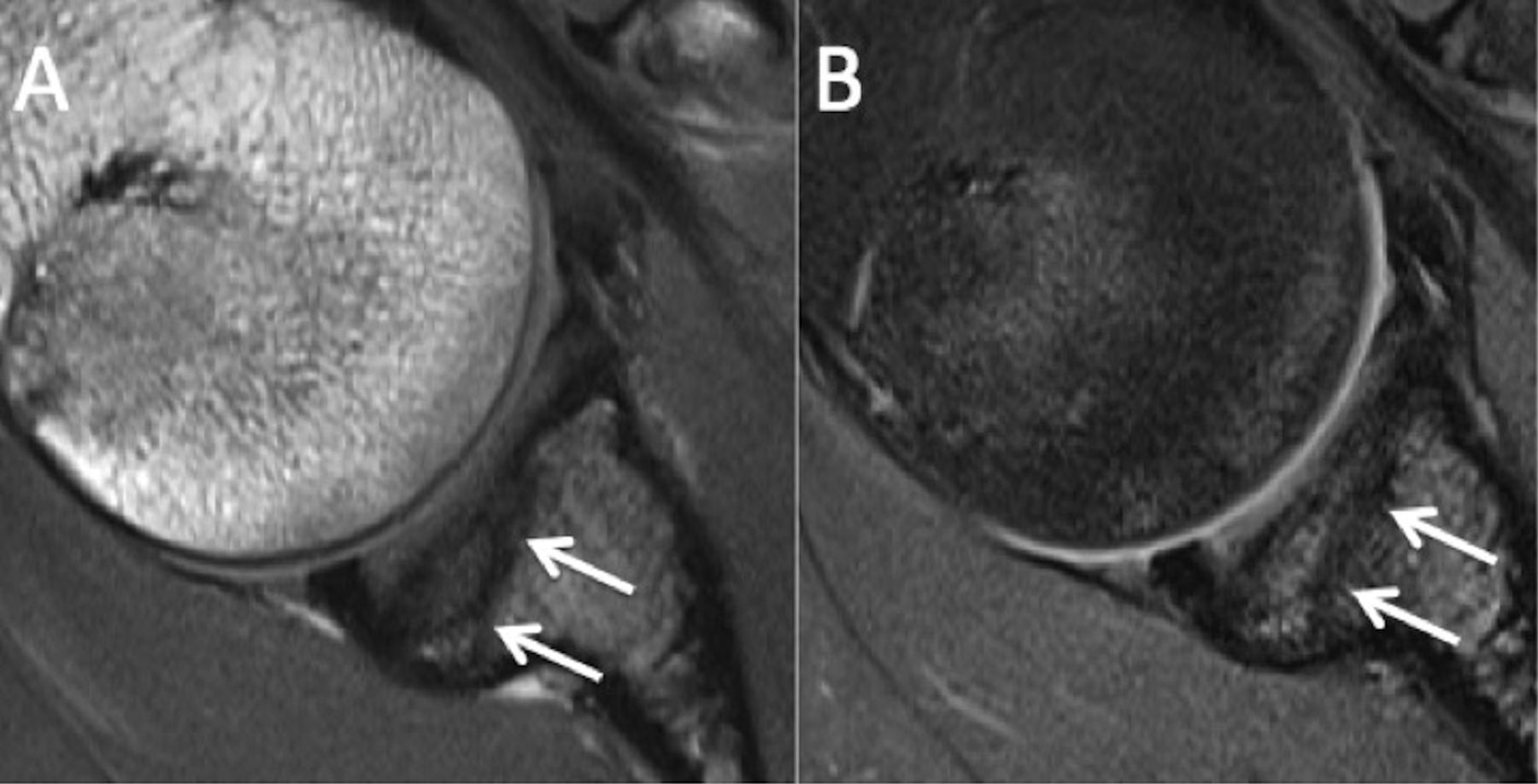
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3