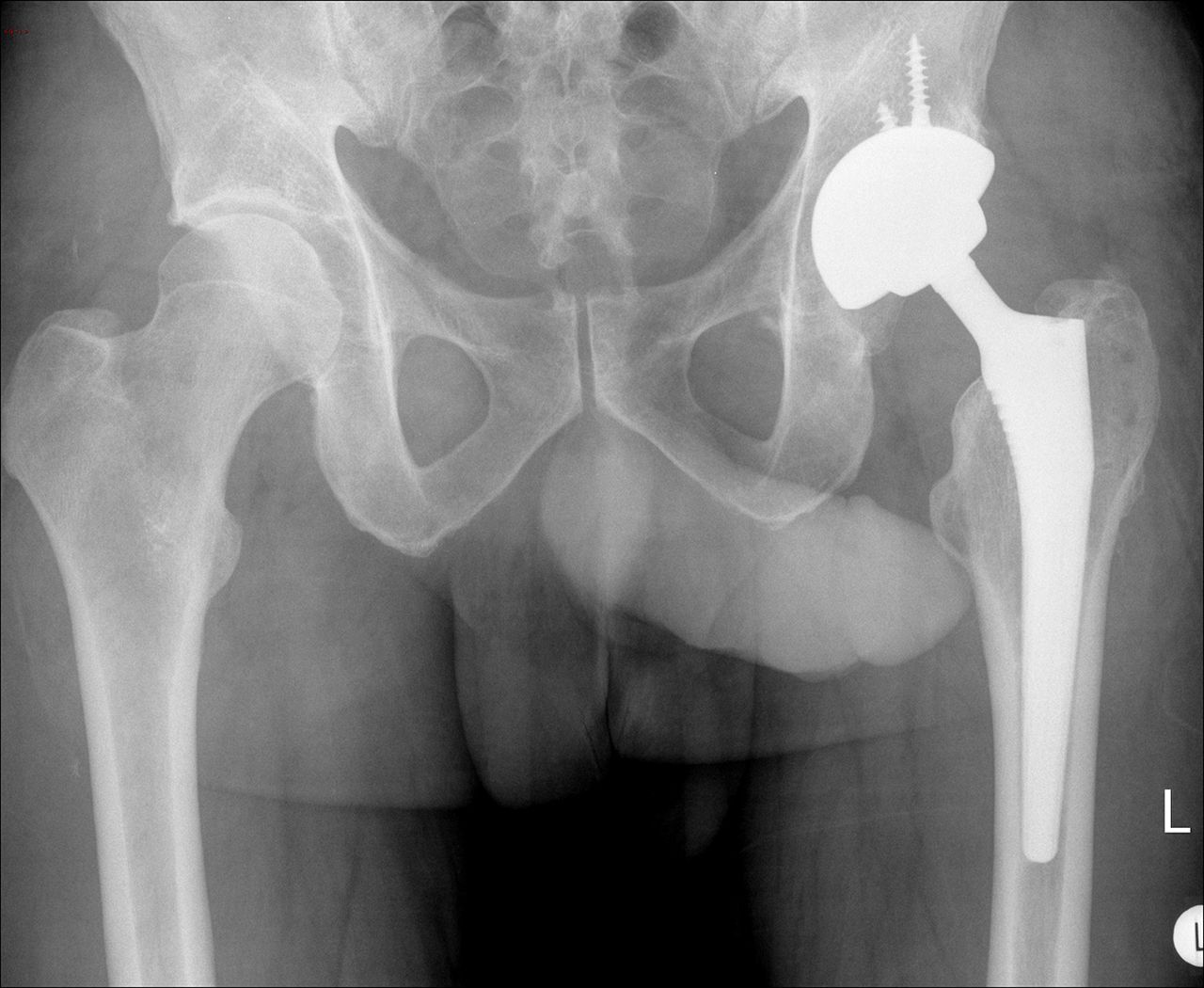
A 40-year-old man presented to the orthopaedic clinic with a 2-year history of increasing hip pain. He had a 10-year history of steroid therapy as treatment for systemic lupus erythematosus and polyarthropathy. A radiograph showed reduced joint space and subchondral sclerosis in the left hip joint (Fig. 1). Magnetic resonance imaging (MRI) was performed and showed findings consistent with osteonecrosis of the femoral head. Because conservative measures did not control the symptoms, he underwent uncemented metal-on-metal (MOM) hip replacement (Cormet resurfacing acetabular cup with MetaFix modular stem; Corin), with insertion of a large-diameter metal head (50 mm) (Fig. 2).
Upon follow-up in the outpatient clinic 6 weeks later, the patient reported swelling at the site of the surgical wound. There was no pain, and he had full range of motion of the hip. The swelling was soft and fluctuant, and the overlying skin was normal. Anteroposterior and lateral radiographs of the hip were unremarkable. An ultrasound showed fluid in the subcutaneous tissues and in the hip joint. Subsequent metal artifact reduction sequence (MARS) MRI showed a large fluid collection overlying the proximal aspect of the left femur (Fig. 3 and Fig. 4). It measured approximately 11 × 10 × 4.5 cm and spread to both sides of the tensor fasciae latae muscle. No soft-tissue mass was identified. The serum cobalt and chromium ion levels were 1.355 and 2.391 ppb, respectively (normal upper limits: cobalt, 7 ppb; chromium, 7 ppb).
An aspiration and arthrogram of the hip joint under local anesthesia showed fluid tracking from the hip joint into the subcutaneous tissues around the distal part of the wound. The serum white blood-cell count was 7.8 cells/μL with 4.7 neutrophils/μL and 0.8 eosinophils/μL. The C-reactive protein (CRP) level was <5 mg/dL, and the erythrocyte sedimentation rate (ESR) was 4 mm/hr (both in the normal range). The hip aspirate showed no growth on the culture specimen. At this time, it was felt than there could have been a small hernia in the muscles due to incomplete closure of the subcutaneous layers at the time of the initial surgery.
To rule out metal allergy, dermatologists performed skin patch testing. Results after 96 hours showed a mildly positive reaction to nickel, although there was a question as to whether this was in fact a reaction to the clothes that were over this particular patch. The patient had an equivocal reaction to cobalt and a negative reaction to chromium. The swelling over the surgical scar failed to resolve, and he reported occasional “squeaking” in the hip, but he had pain-free full range of motion. Additional MARS MRI showed a large fluid collection (9.8 × 6.5 cm) overlying the hip joint and extending into the subcutaneous planes. We decided to perform revision hip surgery.
During the revision surgery, a large mass (12.5 × 10 cm) was identified under the subcutaneous tissues, pouching out through a defect in the fascia. The mass was completely isolated and filled with straw-colored fluid; 400 mL of fluid was aspirated. The acetabular cup and femoral component were found to be solidly fixed with osseous ingrowth. There was no gross evidence of metallosis, and there was little evidence of wear at the head/trunnion interface. The metal articular surfaces on both sides were grossly pristine.
The cup was removed, and a 60-mm uncemented cup (Exceed acetabular porous-coated shell; Biomet) was inserted with a ceramic liner (BIOLOX delta; Biomet). A 36-mm ceramic head with metal sleeve (titanium alloy Ti-6Al-4V) was then placed, and the MetaFix modular stem was well fixed.
Histological analysis of the tissues is shown in Fig. 5 and Fig. 6.
In the context of an MOM prosthesis, the cystic soft-tissue mass was interpreted as a pseudotumor in which the histology showed features typical of aseptic lymphocyte-dominant vasculitis-associated lesion (ALVAL).
Postoperatively, the patient recovered without complication. He underwent rehabilitation with physiotherapists and rapidly returned to his normal activities. The patient has undergone annual follow-ups since surgery, and he has remained symptom-free. The University of California Los Angeles (UCLA) and Oxford scores were 4 and 42, respectively, before the revision; 4 and 25, respectively, at the time of the first-year review; 6 and 14, respectively, at the time of the second-year review; 6 and 13, respectively, at the time of the third-year review; and 6 and 12, respectively, at the time of the fourth-year review. An anteroposterior radiograph of the pelvis 4 years after the revision surgery showed that the uncemented cup with a ceramic liner and a MetaFix modular stem were well-fitted (Fig. 7).
Proceed to Discussion >>Reference: Khawaja S, Holt G, Khan A. Aseptic lymphocyte-dominated vasculitis-associated lesion as early as six weeks after total hip replacement: a case report. JBJS Case Connect. 2017 Feb 08; 7(1):e8.
Recently, there has been a great deal of discussion regarding the use and failure of MOM hip implants. One complication is the development of ALVAL. It has been hypothesized that metal ions are slowly released from the prosthetic bearing surfaces as byproducts of normal wear, and that these metal ions then combine with native proteins to form haptens that elicit a type-IV hypersensitivity response. The trigger to this process appears to be an increased local concentration of metal ions; this increased concentration can initiate an excessive reaction in certain patients. Such a destructive process may, in some patients, lead to osteolysis and prosthetic loosening, or to a solid or cystic mass (pseudotumor). A pseudotumor can cause swelling around the affected hip as well as pain in the groin, which can lead to the inability to bear weight on the affected side.
Because the clinical diagnosis of ALVAL can be difficult, histological examination of the periprosthetic soft tissues is of paramount importance in making the diagnosis; dense perivascular infiltration of lymphocytes is a key feature.
When ALVAL is suspected in symptomatic patients who have undergone total hip replacement surgery, radiographs often contribute little to the investigation. MRI is both sensitive and specific in detecting ALVAL and tissue damage in patients with MOM hip implants. MRI can be used as a screening tool to guide surgeons toward appropriate revision surgery. Nawabi et al. reported that the use of MRI showed sensitivity and specificity of 94% and 87%, respectively, for detecting ALVAL, and 90% and 86%, respectively, for quantifying intraoperative tissue damage. However, because metallic implants can cause artifacts on MRI, MAR sequences are recommended to identify evidence of ALVAL.
This case report demonstrates that abnormalities associated with ALVAL can develop early in the postoperative period. Our patient reported swelling at the surgical site within 6 weeks after surgery. MOM bearings continue to be used worldwide, and we feel that it is important for the orthopaedic community to be aware that patients may develop ALVAL shortly after surgery, even when good implant positioning has been demonstrated and there are normal levels of metal ions.
ALVAL can cause osteolysis and destruction of the abductor muscles and the short external rotator muscles of the hip, which can lead to difficult revision surgery and poor rehabilitation results. Early detection and management of ALVAL can minimize these complications and provide better functional outcome.
Reference: Khawaja S, Holt G, Khan A. Aseptic lymphocyte-dominated vasculitis-associated lesion as early as six weeks after total hip replacement: a case report. JBJS Case Connect. 2017 Feb 08; 7(1):e8.
What is the diagnosis?
Periprosthetic infection
Echinococcal cyst
Inflammatory pseudotumor (aseptic lymphocyte-dominant vasculitis-associated lesion)
Particle-induced bone resorption (osteolysis)
Synovial (ganglion) cyst


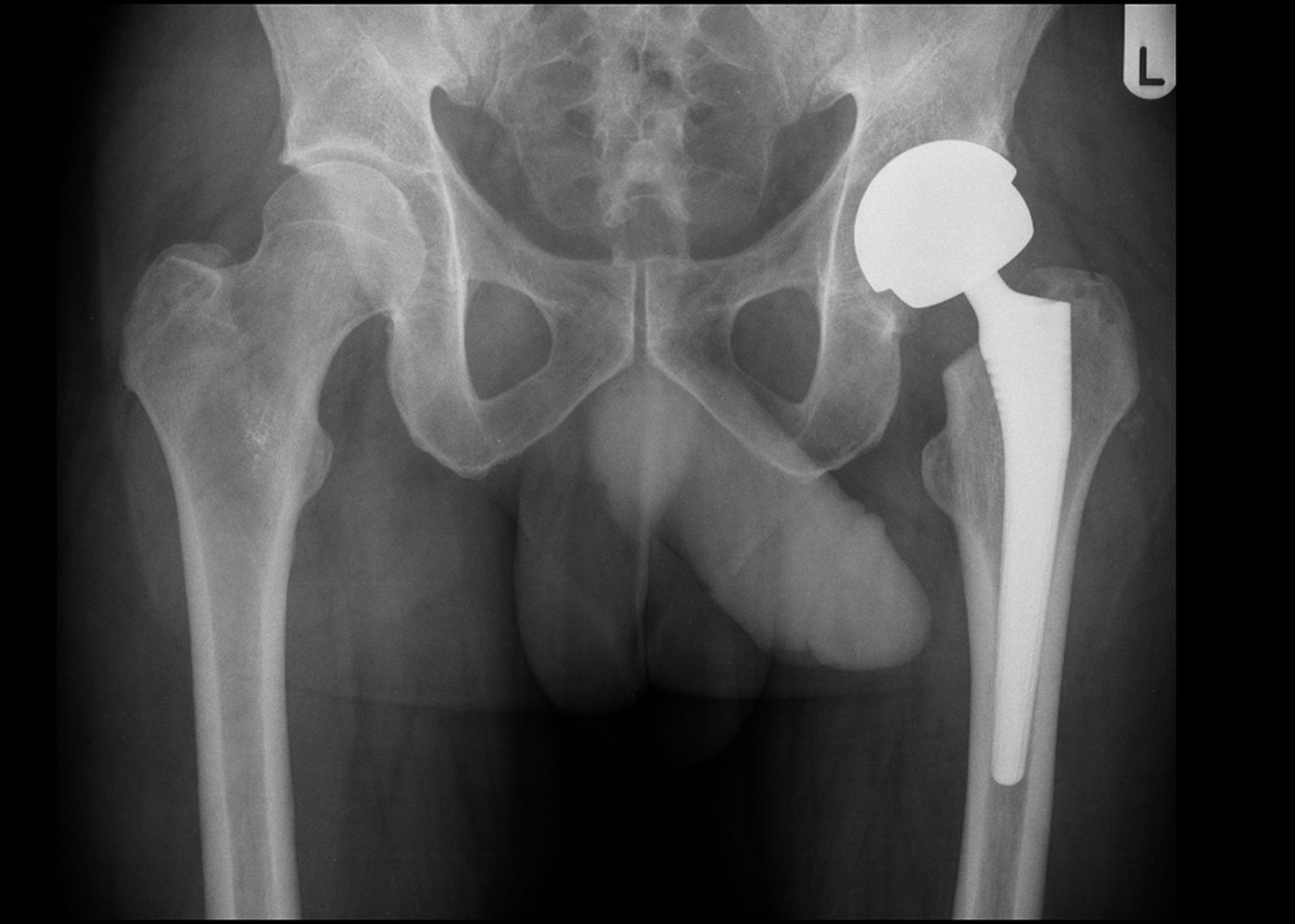

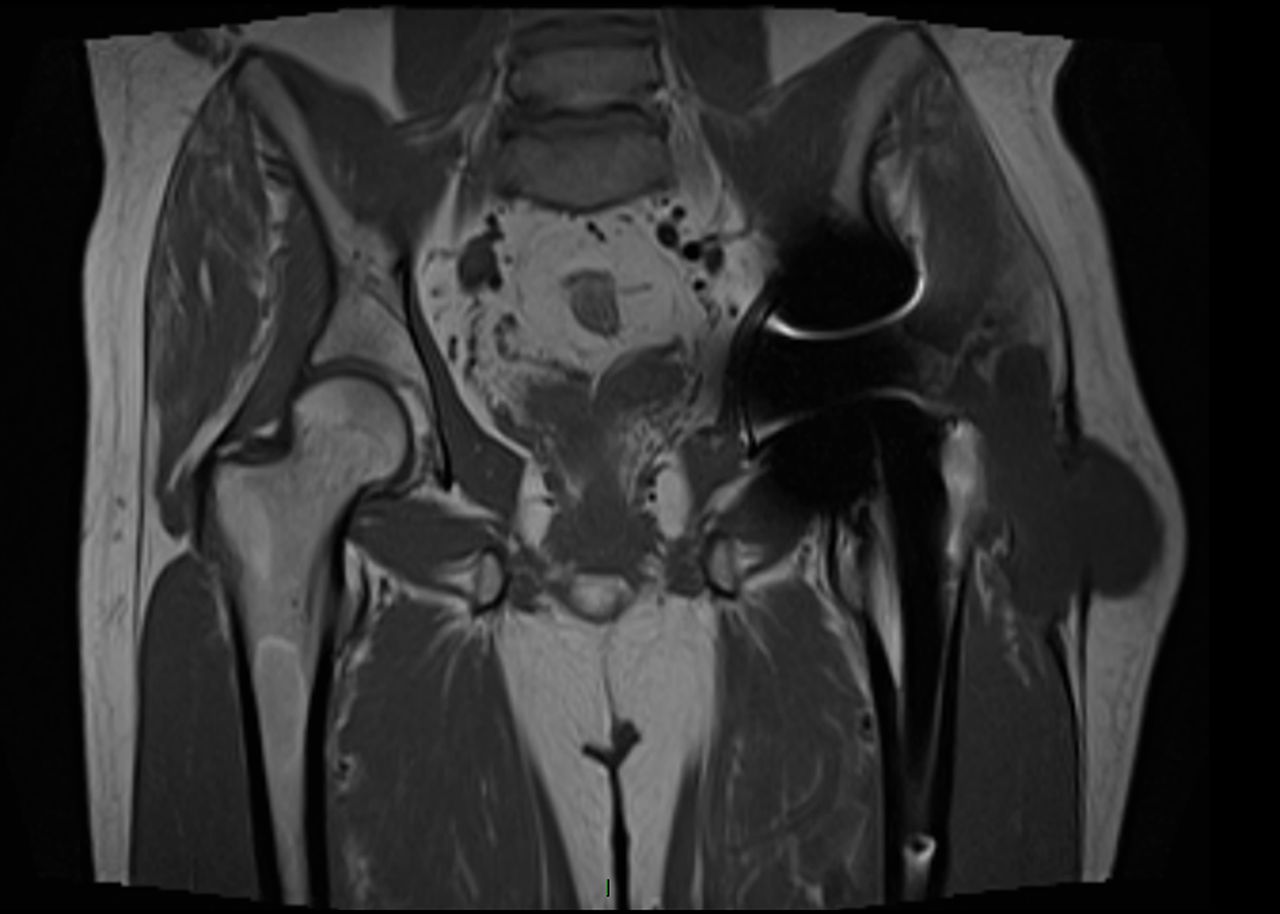
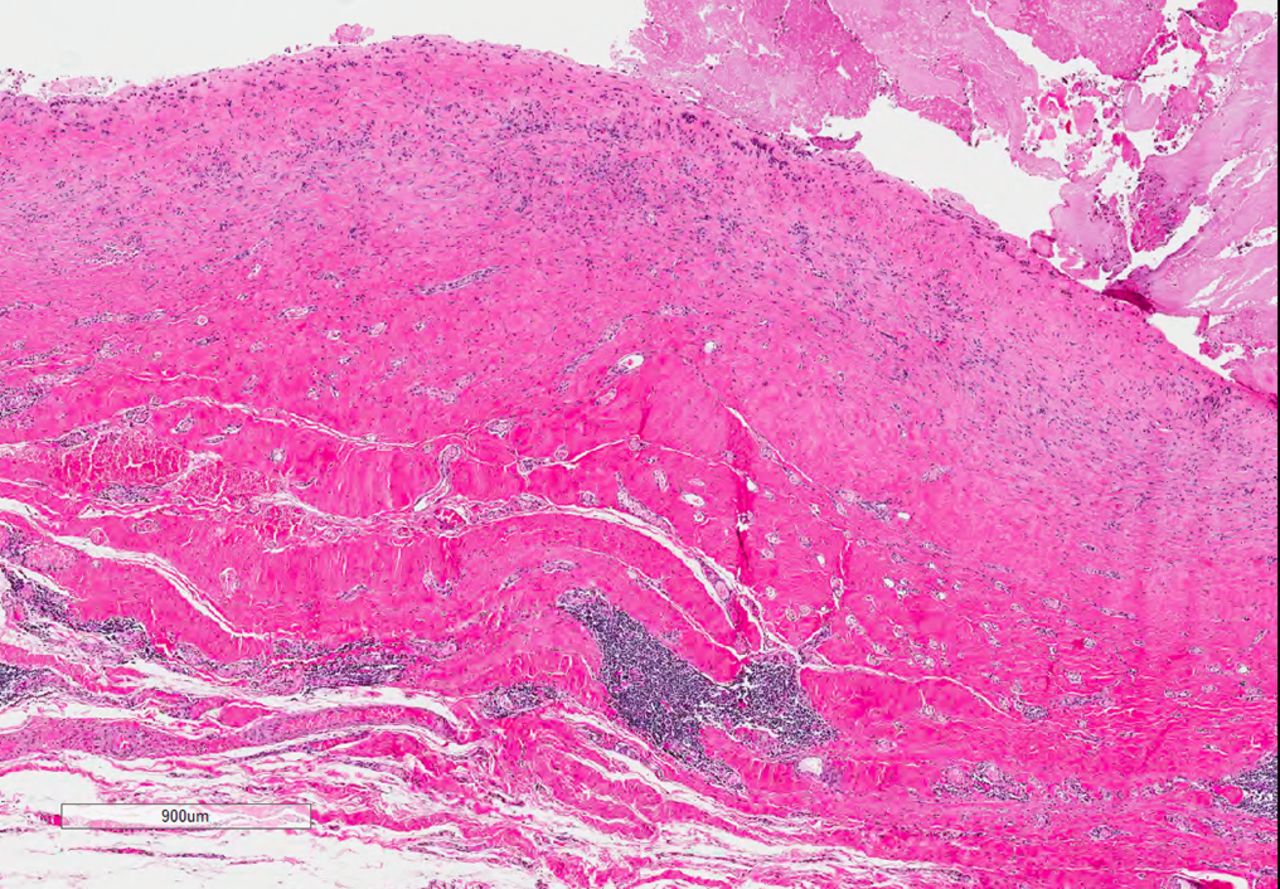
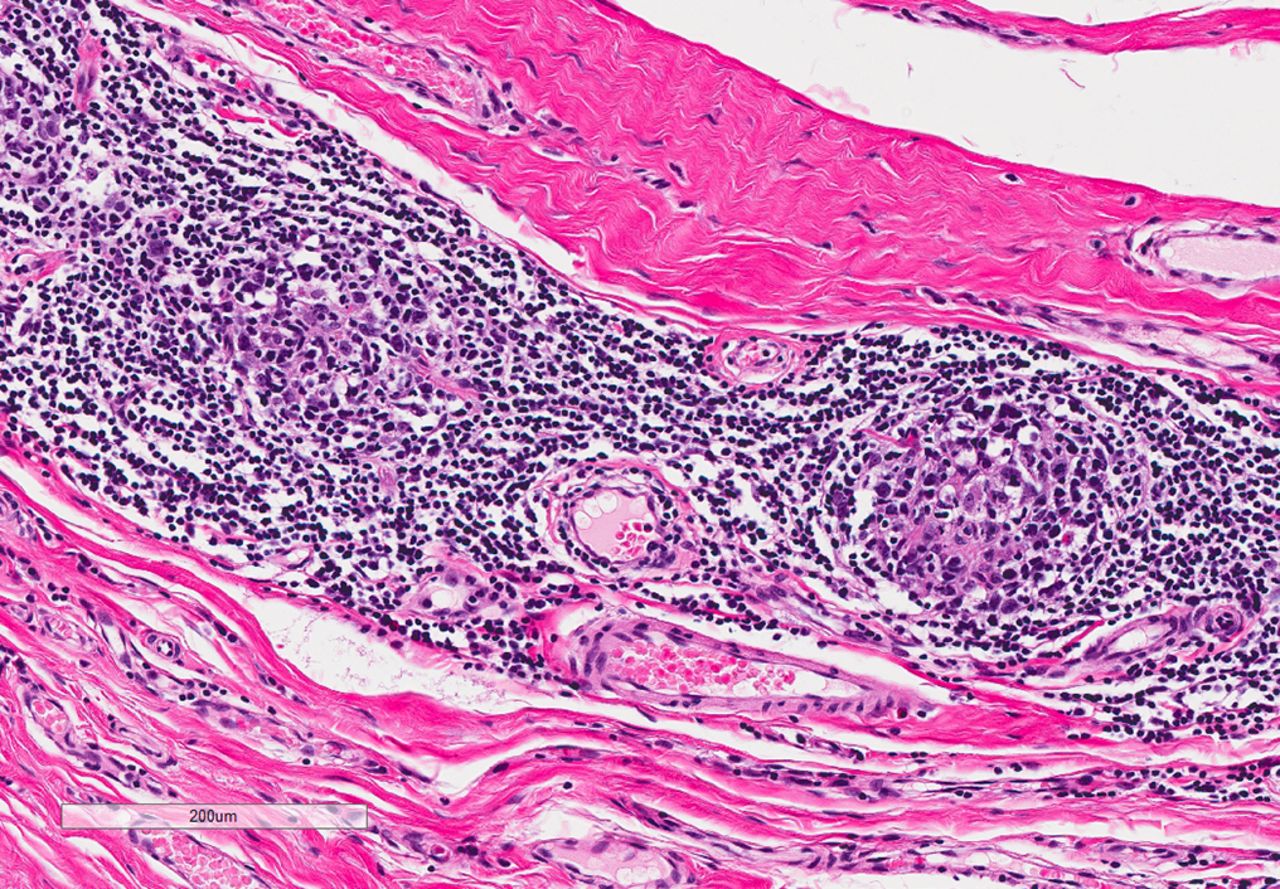
 Fig. 1
Fig. 1 Fig. 2
Fig. 2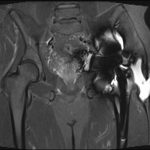 Fig. 3
Fig. 3 Fig. 4
Fig. 4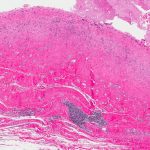 Fig. 5
Fig. 5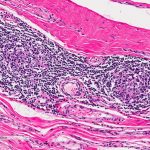 Fig. 6
Fig. 6 Fig. 7
Fig. 7