A 26-Year-Old-Man with Spinal Injury Following a Car Accident
September 7, 2016
A 26-year-old man was involved in a high-speed motor vehicle collision resulting in an isolated spinal injury. Physical examination demonstrated no sensorimotor deficit; rectal examination showed normal tone. Notably, clonus was present bilaterally on reflex examination, indicating upper motor neuron involvement. The patient received a Foley catheter on admission and received intravenous morphine for pain. Computed tomography (CT) (Fig. 1) was made and MRI magnetic resonance imaging (MRI) (Figs. 2-A and 2-B) was acquired.
The CT scan demonstrated an L1 burst fracture (AO type A3.2) with a retropulsed fragment causing approximately 10% to 20% canal compromise (Fig. 1). There was 20% to 30% loss of height and minimal kyphotic collapse. The MRI (Figs. 2-A and 2-B) showed retropulsion of the osseous fragment at L1 (thick arrow) and compression of the conus medullaris anteriorly (thin arrow) with associated edema of the conus.
Initially, the plan was to treat the patient nonoperatively with a thoracolumbosacral orthosis. Despite bracing, the patient continued to have recalcitrant back pain as well as urinary retention following Foley catheter removal. In light of the clinical course, operative treatment was recommended. Within 96 hours of admission, the patient underwent L1 laminectomy with posterior spinal fusion from T12 to L2 utilizing pedicle screw instrumentation. Substantial swelling of the conus medullaris was seen intraoperatively. The dura was left intact following osseous decompression.
Postoperatively, the patient quickly regained the ability to void urine. On postoperative MRI to evaluate the decompression and extent of conus medullaris injury (Fig. 3), substantial residual edema was noted at the level of the conus. The patient was noted to have normal neurologic function and no issues with bowel, bladder, or sexual function at the 1-year follow-up. He returned to work with a 30-lb (14-kg) weight lifting and carrying restriction.
Proceed to Discussion >>Reference: Bhandutia AK, Winek NC, Tomycz ND, Altman DT. Traumatic conus medullaris syndrome: A case report and review of the literature. JBJS Case Connect. 2016 May 25;6(2):e38.
The conus medullaris comprises the termination of the spinal cord and transition to the nerve roots of the cauda equina; it contains the medially based caudal roots and the laterally based cephalad roots. Accordingly, the caudal nerve roots are more likely to be affected by disc or osseous compression. Substantial variation in the level of the conus, ranging from T11 to L3, has been validated in many patient populations, suggesting a difference in neurologic injury pattern even in patients with similar fractured vertebral levels.
A conus-level injury is typically a mixed upper and lower motor neuron injury. The mixed presentation creates difficulty in the diagnosis of conus medullaris syndrome (CMS), especially in comparison with cauda equina syndrome. The presence of an indwelling Foley catheter during trauma resuscitation on admission can also lead to a delay in diagnosis. Nonetheless, the common presentation in CMS involves various grades of several symptoms: saddle anesthesia, urinary retention, loss of bowel control, sexual dysfunction, and inconsistent bilateral lower-extremity weakness. Deep tendon reflexes, when elicited, depend on the predominance of upper versus lower motor neuron involvement. Furthermore, the bulbocavernosus reflex, mediated by the S2-S4 nerve roots, will not be reliably found in patients with a conus injury. Urinary retention occurs through interruption of the reflex arc to the bladder, resulting in a flaccid lower-motor-neuron-dominant bladder and an atonic anal sphincter, in addition to sexual dysfunction. Bladder dysfunction can range from mild to severe, with a mild deficit involving incomplete emptying of the bladder and the most severe stage involving retention and overflow incontinence. Sexual dysfunction can be graded in four stages ranging from erection insufficiency with an inability to perform intercourse through inability to achieve erection. Sensation at the lowest sacral dermatomes and the presence of an intact bulbocavernosus reflex are noted to be favorable prognostic indicators.
MRI is the study of choice to evaluate the spinal cord injury and compression, the posterior ligamentous complex, and the presence of traumatic disc herniation or epidural hematoma. In comparison with CT imaging, which is optimal for osseous evaluation, MRI can predict the neuraxial injury level, which has been shown to correlate with patient outcomes. Remarkably, a misclassification rate of 33% was reported when injury was categorized by vertebral level instead of MRI-based neuraxial level.
Recovery is dependent on patient age, injury magnitude, compression, and neuraxial injury level. A notable retrospective review by Harrop et al. evaluated 95 patients with spinal injury from T4 to S5 and stratified patients according to neurologic level of injury; 93% of patients with CMS demonstrated improvement of at least one ASIA (American Spinal Injury Association) grade compared with 22% of patients with a more cranial level of injury. No discussion was included regarding operative versus nonoperative management. The authors concluded that a more complete recovery was likely the result of a greater proportion of lower motor neurons at the level of the conus, referred to as nerve root escape. Nerve root escape is noted to play a key role in the variability of presentation of conus injury. The study highlighted the importance of utilizing the neuraxial level for injury classification.
The literature is inconsistent with respect to the role of neural compression in conus medullaris injury. Some authors believe that the initial injury is responsible for the neurologic deficit, with operative treatment recommended only if the fracture pattern calls for stabilization or if a progressive neurologic deficit is present. In contrast, other authors found an association between >50% canal compromise and a neurologic deficit, and they noted better recovery with operative treatment. It is likely that imaging may represent a static picture of a dynamic pathology within the spinal canal. Boerger et al. conducted a systematic review of thoracolumbar fractures associated with a neurologic deficit and failed to note an advantage of operative decompression over nonoperative management in terms of neurologic outcomes. Limitations of all studies performed to date include an uncontrolled retrospective study design and a lack of injury classification based on neuraxial level.
We are aware of no controlled studies that provide evidence regarding the natural history of neurologic recovery following nonoperative treatment of conus medullaris injury. The financial pressure to decrease the length of stay, finality of surgical treatment, and patient expectations make surgical intervention an attractive option despite a lack of evidence of the superiority of operative intervention. It is admittedly difficult and unethical to withhold potentially beneficial surgical treatment in order to conduct prospective controlled studies. While little evidence exists regarding the necessity of decompression in a neurologically stable patient, we favor decompression in patients with neural compression or a progressive neurologic deficit.
Decompression can be performed utilizing an anterior or a posterior approach. Uncontrolled studies have shown good results in patients who had undergone either approach. Bradford and McBride compared these decompression approaches and noted a significant (p = 0.004) difference in recovery rate in favor of anterior decompression (70% versus 12% for posterior decompression) in a subset of patients with an apparent conus medullaris injury (based on vertebral level).
Clohisy et al. evaluated the timing of surgery in relation to the 48-hour time point in patients with a conus injury and noted a trend (p = 0.1) toward a difference in bowel and bladder recovery in favor of early anterior decompression (recovery in 4 of 11 patients compared with zero of six who underwent late decompression). Another series evaluated late decompression (at greater than 3 months) and found improvement in approximately 50% of patients with a conus medullaris injury, although patients were stratified by vertebral level and the presence of bladder dysfunction. Recommendations regarding operative treatment and its timing can only be inferred from the literature pertaining to acute cauda equina syndrome, which largely recommends decompression within 48 hours from presentation and indicates resulting positive effects on sensory, motor, rectal, and urinary dysfunction compared with intervention after 48 hours. However, in comparison with the literature regarding spinal cord injury and cauda equina syndrome, the literature describing CMS is sparse.
The current knowledge base poorly classifies conus-level injuries, and outcomes are consequently difficult to ascertain in this population. Sparse data are available with regard to the natural history of conus medullaris injury treated nonoperatively. Further studies should utilize the neuraxial level of involvement in assessing neurologic outcomes. Higher-level evidence is needed regarding the optimal treatment of traumatic CMS.
Reference: Bhandutia AK, Winek NC, Tomycz ND, Altman DT. Traumatic conus medullaris syndrome: A case report and review of the literature. JBJS Case Connect. 2016 May 25;6(2):e38.
What is the diagnosis?
Burst fracture of L1
Hemangioma
L1-L2 disc herniation
Epidural hematoma
Osteoblastoma


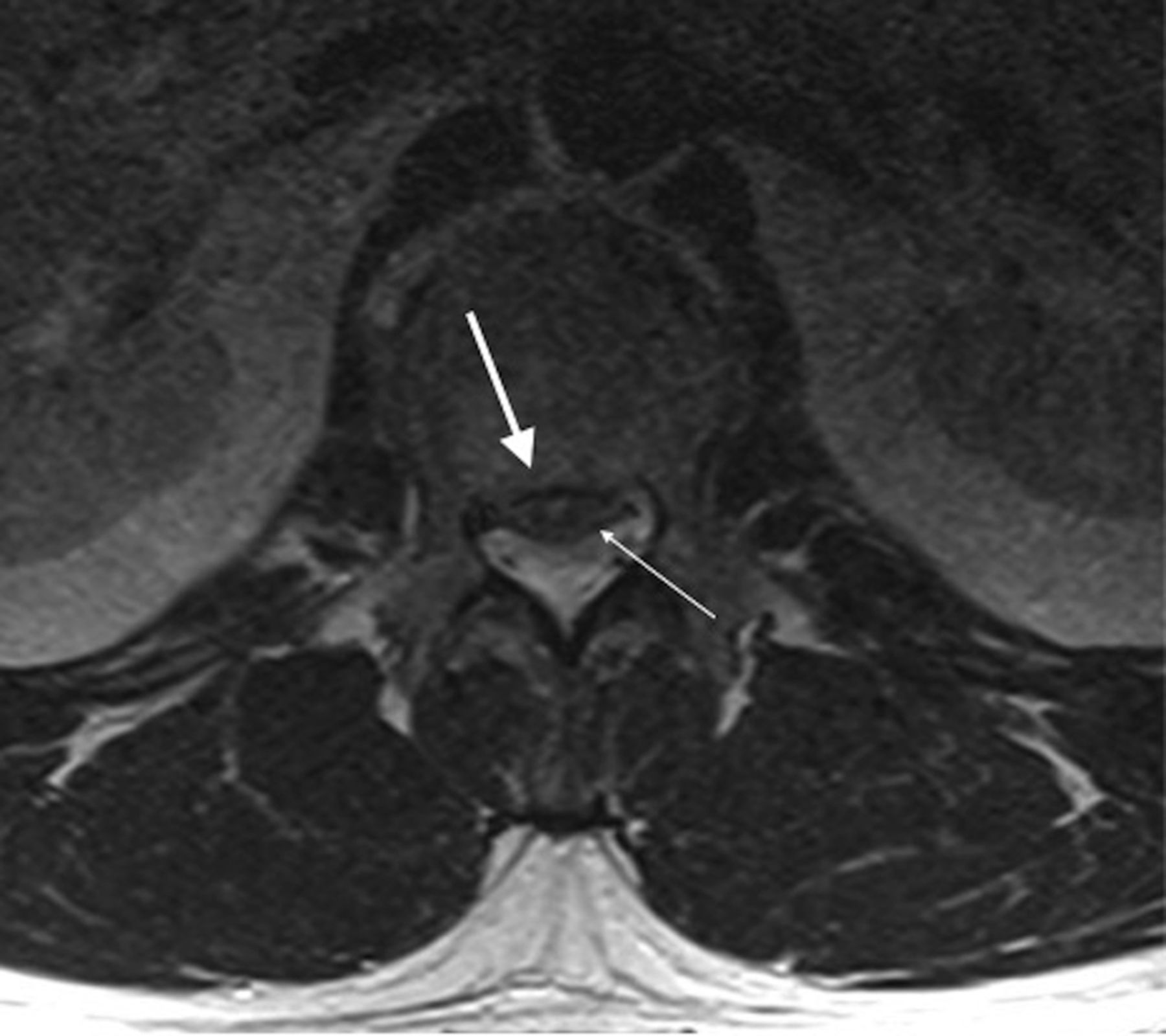

 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B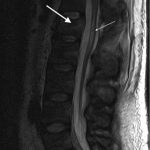 Fig. 3
Fig. 3