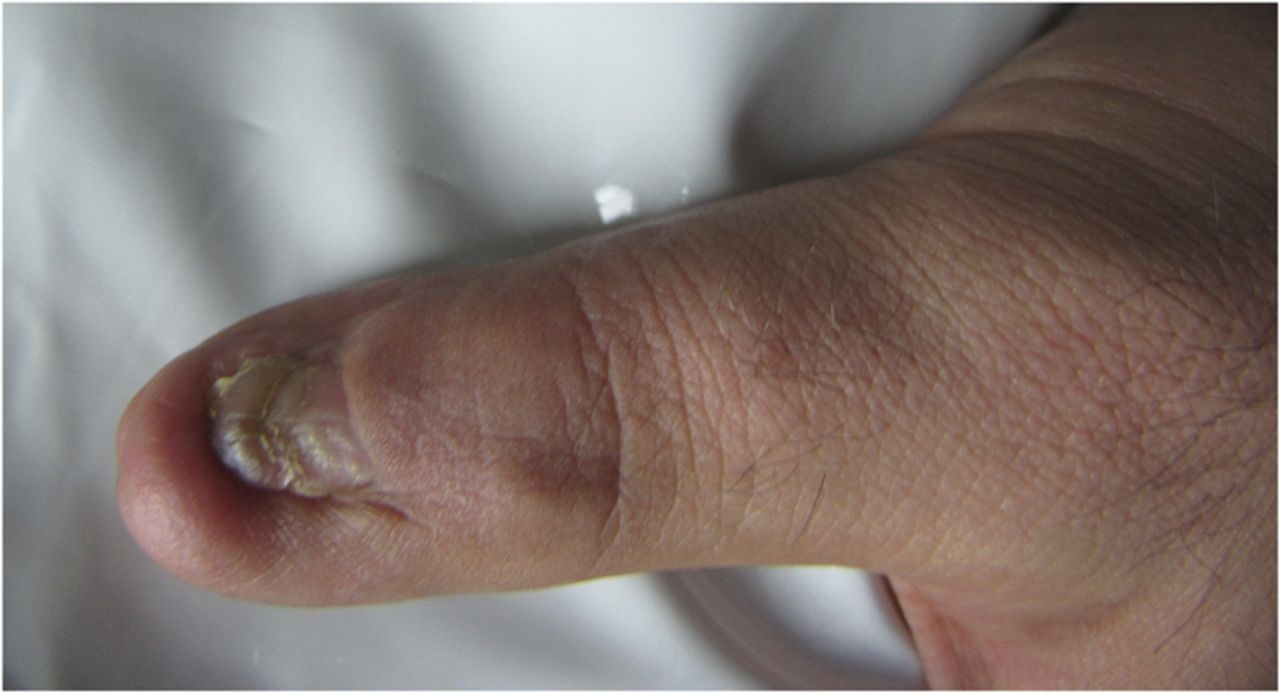
A 28-year-old man presented with pain in the distal phalanx of the left thumb. Symptoms initially manifested as itching and intermittent swelling that had begun 3 months previously. Over time, this had changed to increasing pain. Physical examination findings included tenderness in the distal phalanx and painful range of motion in the interphalangeal joint. The skin of the affected area was slightly erythematous with induration. There was no history of trauma and there were no constitutional symptoms.
Radiographs revealed a lytic lesion with a honeycomb appearance in the distal phalanx, without remarkable cortical expansion or periosteal reaction (Fig. 1). A radionuclide whole-body bone scan showed increased uptake in the distal phalanx but was otherwise normal (Fig. 2). There was high signal intensity of the distal phalanx on the T2-weighted magnetic resonance imaging (MRI) and hypointense signal abnormality on the T1-weighted MRI without soft-tissue involvement (Figs. 3-A and 3-B). The chest radiograph and chest computed tomography scan were normal.
An open incisional biopsy was performed through a dorsomedial approach. The results of the biopsy are shown in Figure 4.
The combination of the morphology evident on the hematoxylin and eosin-stained slide with the positive immunohistochemical stain for CD99 was interpreted as Ewing sarcoma (ES).
The high-grade intracompartmental tumor with no evidence of metastasis was considered to be stage IIA in accordance with the Enneking surgical staging system. The patient underwent 4 courses of neoadjuvant chemotherapy with vincristine, ifosfamide, doxorubicin, and etoposide (VIDE protocol). The classical surgical approach for disease of the distal part of the thumb is amputation. However, to preserve functional and cosmetic qualities of the thumb, as desired by the patient, a salvage procedure was considered and approved at our hospital’s tumor board meeting.
Surgery was performed under general anesthesia, with application of a tourniquet to the proximal part of the arm. With an extension of the previous incision, a dorsal skin flap that included the nail bed was elevated, and the distal phalanx was excised with the biopsy tract; the surgical margin was confirmed to be tumor-free via frozen section. Reconstruction was done with a fresh-frozen allograft counterpart (obtained from our hospital bone bank) that was fused to the first phalanx with 2 pins. Histological examination of the excised tumor specimen showed a 100% positive chemotherapy effect. Postoperative radiographs (Fig. 5) show the allograft, and a photograph (Fig. 6) shows the appearance of the thumb 3 months after surgery.
Chemotherapy was resumed 2 weeks after the operation; the pins were removed after 6 weeks. The patient was followed every 3 months. Two years after surgery, there was no local recurrence, no distant metastasis, and no resorption of the allograft (Fig. 7). To the best of our knowledge, this novel procedure has not been reported previously in the treatment of ES at this site. The patient was healthy and had no pain or inflammation of the thumb.
Proceed to Discussion >>Reference: Jamshidi K, Mazhar FN, Moghimi J. Ewing sarcoma of the distal part of the thumb: allograft reconstruction to preserve function: a case report. JBJS Case Connect. 2013 Sep;3(3):e88.
ES was first described as a malignant tumor originating from the bone with the potential to invade soft tissue. Although there are debates, many now believe that ES arises from mesenchymal stem cells and can also occur extraosseously. ES and primitive neuroectodermal tumor (PNET) often have the t(11;22)(q24;q12) chromosomal translocation. Usually, this type of tumor is seen during the first or second decade of life, most often in the long bones and pelvis. ES of the hand is a very rare condition; we believe that only 17 cases have been reported since 1955. The most commonly affected bones are the metacarpals; tumor occurrence at the phalanges is quite rare.
According to a recently published study on ES of the finger, there is a male predisposition (69%), and the average age of patients is 18.5 years, ranging from 5 months to 51 years. The thumb (28%) and the middle finger (28%) were the most commonly affected sites. Pain and swelling of the affected fingers were the main symptoms at diagnosis. Itching, as mentioned by our patient, is an unusual presentation. In a review of patients with ES, Euler et al. noted that patients initially were in good health and there were no reports of fever or weight loss. In addition to ES, the radiographic differential diagnosis of a lytic lesion of the distal phalanx includes chronic infection, intraosseous epidermoid cyst, chondroma, intraosseous ganglion, intraosseous glomus tumor bone cyst, giant-cell tumor, and metastatic lesion. Radiographs from our patient showed a nonexpansile honeycomb lytic lesion that, along with inflammatory features, made osteomyelitis or chronic infection more probable. In our case, osteomyelitis and a vascular tumor (e.g., glomus tumor) were high on the differential diagnosis list; pathologic examination led to the final, correct diagnosis of ES.
For ES of the finger, different surgical treatment modalities have been applied based on tumor location and surgical staging. Most of the literature has emphasized the benefit of tumor resection as the most important stage in the management of ES of the finger because of the accessibility of the hand. Because ES is susceptible to chemotherapy, preoperative or postoperative chemotherapy is an integral part of the treatment plan. The regimen may be adjusted based on histological response to neoadjuvant therapy.
In order to avoid a hand deformation, Kinsella et al. suggested the combination of chemotherapy with radiation therapy without surgery, although the long-term results remain uncertain. Conversely, reconstruction of the distal aspect of the thumb has been reported by Adani et al. They used the entire nail and the distal phalanx of the great toe for reconstruction; however, they did not address the morbidity of the donor site. In our patient, we chose reconstruction, but we wanted to avoid compromising any other body parts.
Because of the thumb’s importance in the function of the hand and to achieve the mentioned goals, we performed allograft reconstruction. The tumor of the distal phalanx was replaced by its allograft counterpart and arthrodesed to revive maximum possible function. Fortunately, the absence of severe adjacent soft-tissue involvement was an important factor here. Although our case has only had short-term follow-up thus far, the patient’s satisfaction suggests that the described surgical approach is a good method for managing ES of the thumb.
In summary, despite its rarity in the phalanges, ES should be considered in the differential diagnosis of lesions at this location. Immediate treatment can provide a better prognosis. Currently, the most favorable treatment regimen for ES of the phalanx is surgery and chemotherapy, with the addition of neoadjuvant therapy as necessary for preserving function.
Reference: Jamshidi K, Mazhar FN, Moghimi J. Ewing sarcoma of the distal part of the thumb: allograft reconstruction to preserve function: a case report. JBJS Case Connect. 2013 Sep;3(3):e88.
What is the diagnosis?
Langerhans cell histiocytosis (eosinophilic granuloma)
Osteomyelitis
Giant cell tumor of bone
Ewing sarcoma
Synovial sarcoma

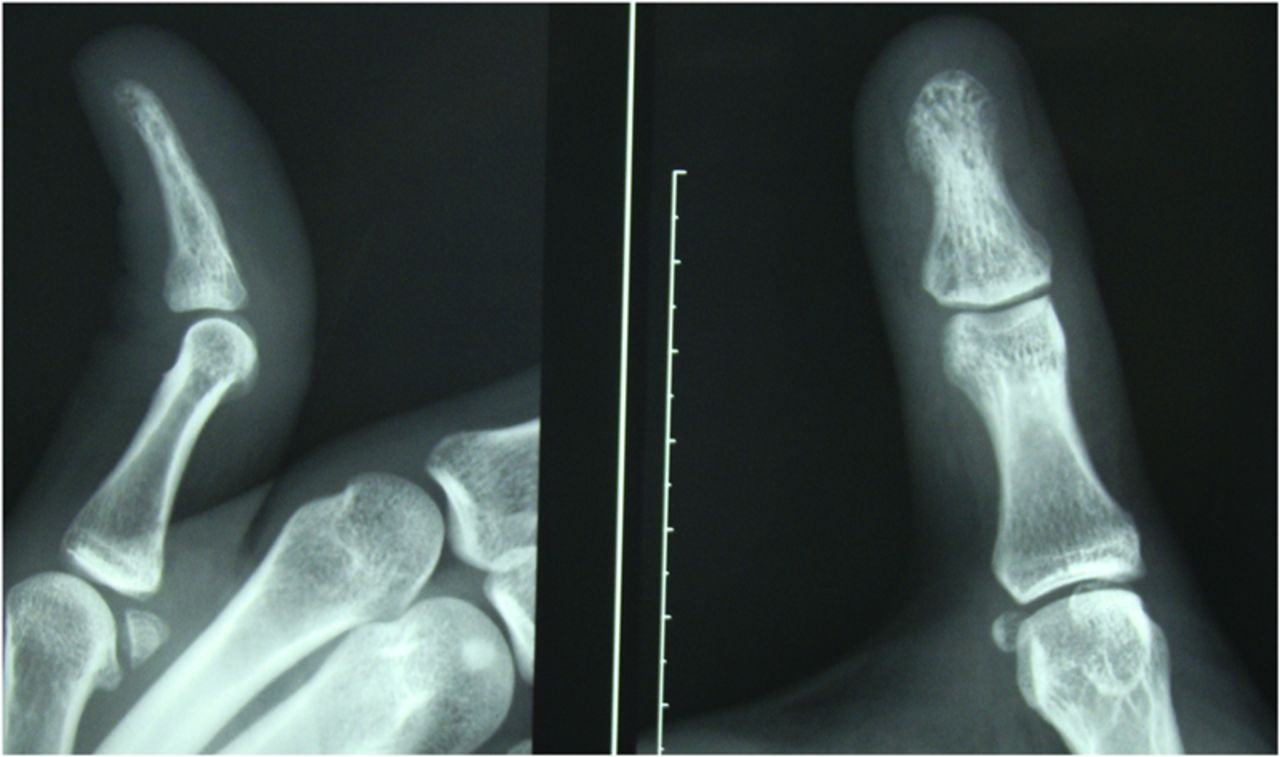
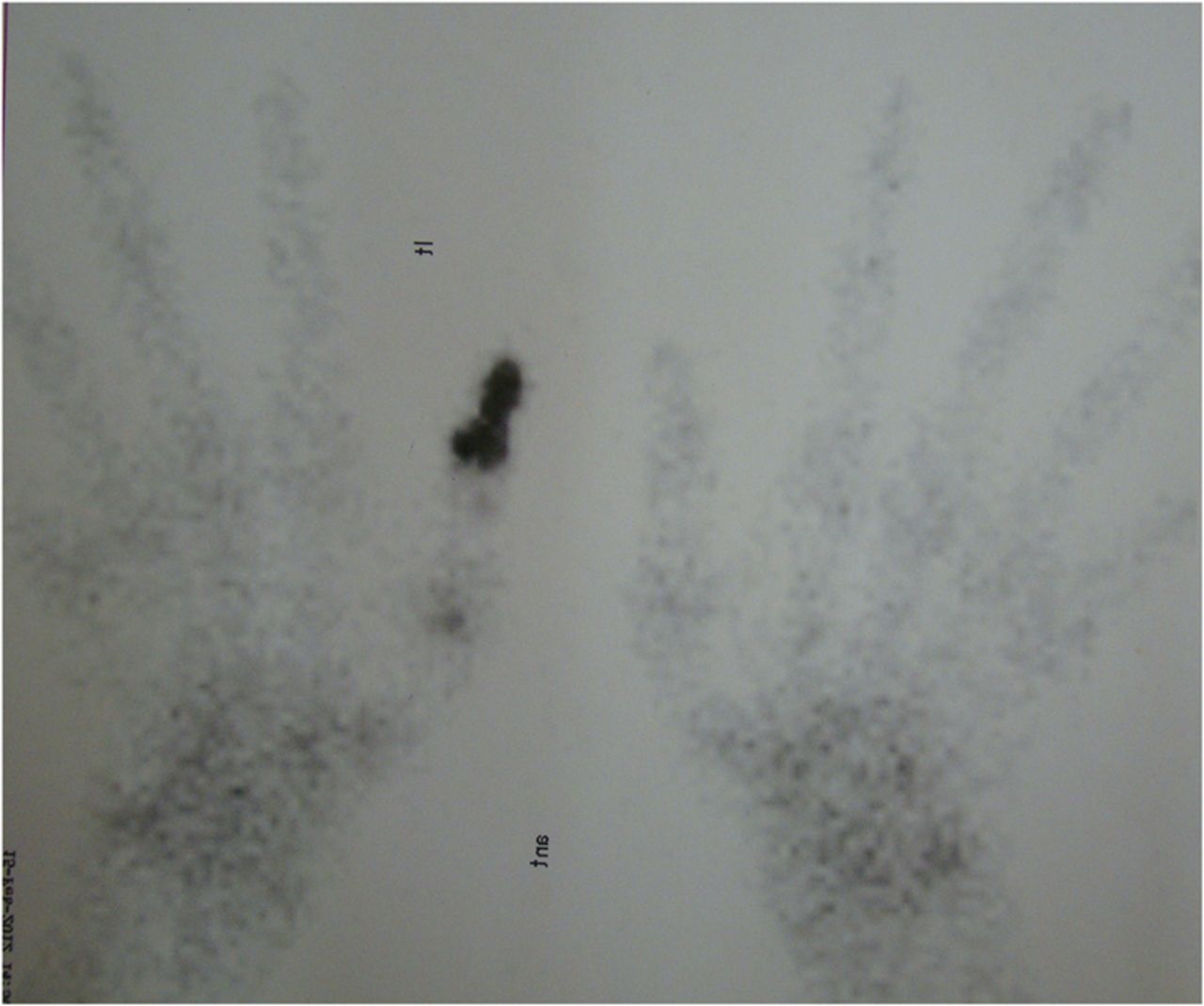
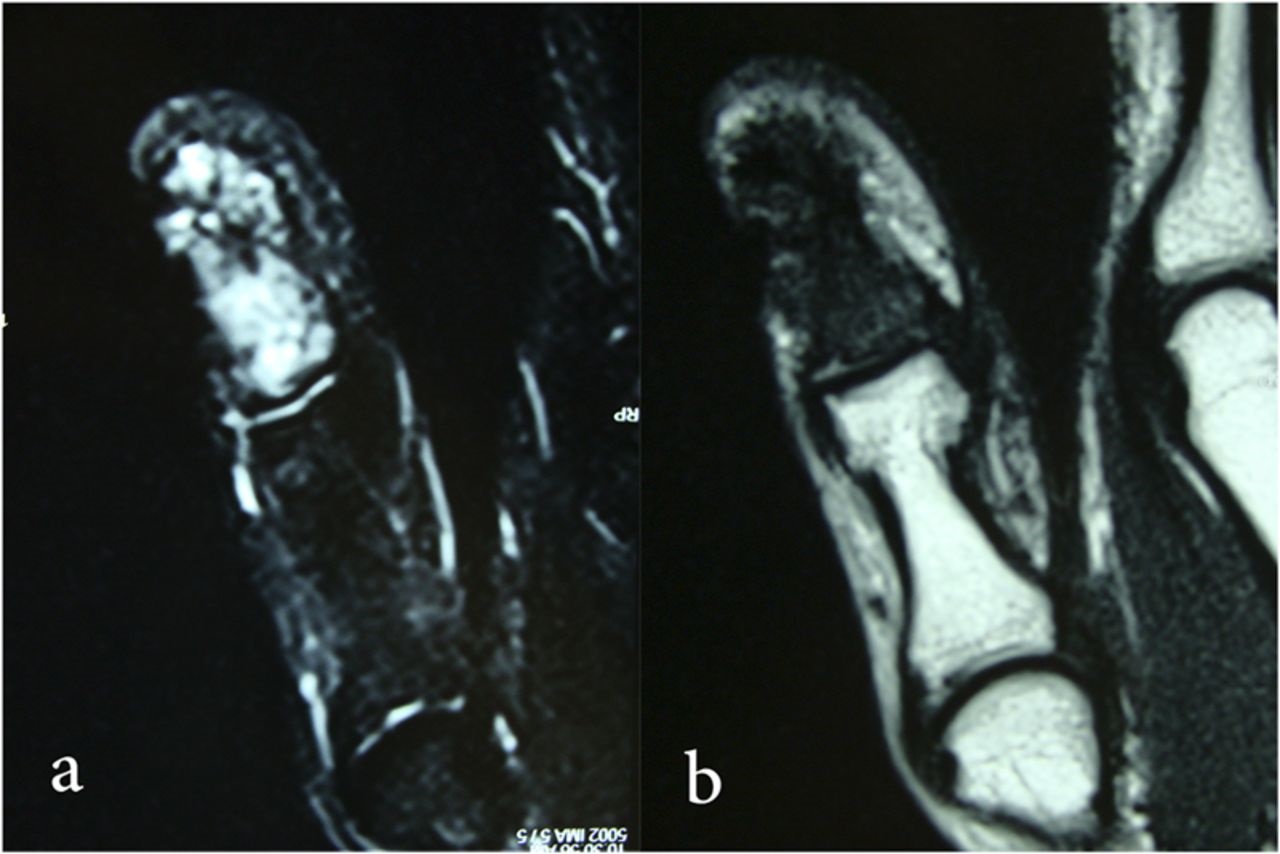

 Fig. 1
Fig. 1 Fig. 2
Fig. 2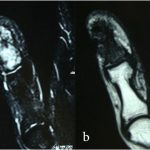 Fig. 3
Fig. 3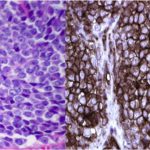 Fig. 4
Fig. 4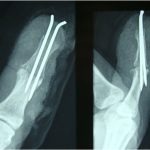 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7