A 51-year-old woman presented for evaluation of left thumb swelling. She reported having no acute injury or trauma. The swelling progressed over 2 weeks and was painless. The patient also reported recent bruising of the thumb. There was no history of wounds, drainage, fevers, chills, or other constitutional symptoms.
The medical history was notable for endometrioid ovarian carcinoma which had been treated with a total abdominal hysterectomy and chemotherapy. The postoperative course had been complicated by a cerebrovascular accident (CVA) that had caused moderate left hemiparesis with decreased sensation. Other medical problems included tetralogy of Fallot, cardiac arrhythmia that was treated with an implanted cardiac defibrillator, asthma, and gastroesophageal reflux disease. Prior to the cancer diagnosis, the patient had worked as a civilian contractor for the military. She was a nonsmoker who used a wheelchair for mobility after the CVA. Given the patient’s medical comorbidities, she was admitted for evaluation by the internal medicine team.
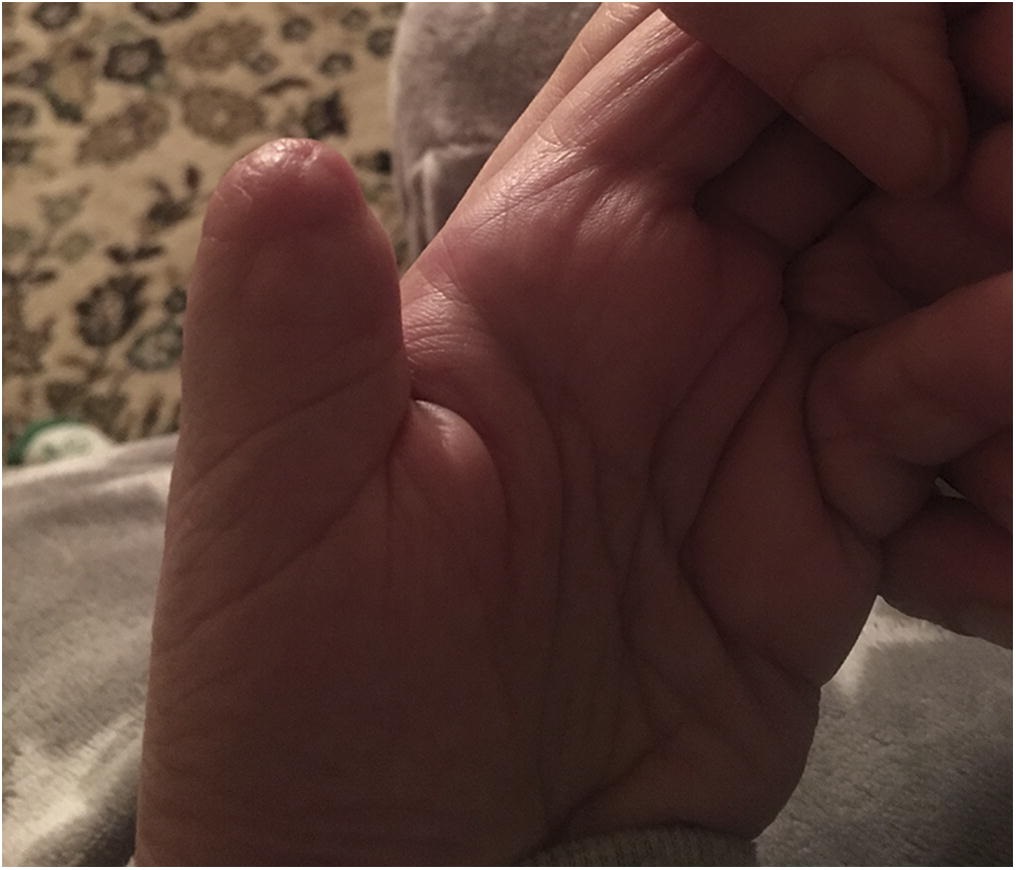
On examination, the thumb was swollen distally, with subungual and surrounding ecchymosis and erythema. The thumb was not tender over the distal phalanx or the nail plate. There were no open wounds, and there was no fluctuance (Fig. 1). Examination of the area proximal to the interphalangeal joint was normal. Sensation to light touch was diminished throughout the thumb, but comparable to the adjacent fingers. The thumb was warm and appeared well-perfused, with 2-second capillary refill at the pad.
Radiographs revealed an expansile lytic lesion in the distal phalanx of the thumb, with a tuft fracture and moderate swelling of the surrounding soft tissue (Fig. 2). Serologic studies were performed; the findings included a white blood-cell count of 13.11 K/μL (normal, 4.50 to 11.00 K/μL) with 64% neutrophils (normal, 40% to 70%), a C-reactive protein level of 2.9 mg/dL (normal, 0 to 1 mg/dL), and an erythrocyte sedimentation rate (ESR) of 38 mm/hr (normal, 0 to 20 mm/hr). Considering the patient’s immunocompromised state due to chemotherapy, blood cultures were obtained, and empiric antibiotic therapy was initiated, despite a low suspicion for infection. The orthopaedic surgery department was consulted; biopsy and amputation were discussed thoroughly with the patient. Given the already limited use of the left hand as a result of the previous CVA and the desire to avoid future procedures, the patient and surgeon elected to proceed with amputation. Magnetic resonance imaging (MRI) was acquired preoperatively for surgical planning to evaluate marrow changes or soft-tissue extension proximal to the interphalangeal joint. Findings were limited to the distal phalanx, which was consistent with the clinical examination.
A fishmouth incision was made over the interphalangeal joint of the thumb. The extensor pollicis longus tendon, the flexor pollicis longus tendon, and the collateral ligaments were incised. Neurectomies were performed. The thumb was amputated at the interphalangeal joint. The destructive lesion in the distal phalanx had associated serous fluid. There was obvious destruction of the normal cancellous bone. Multiple intraoperative culture specimens were obtained, and the amputated thumb was sent for formal pathologic examination. No purulence was encountered. Histology from the amputation specimen is shown in Figure 3. One of the intraoperative culture samples revealed “very light hyphal elements” with Calcofluor White Stain. No fungi, bacteria, or mycobacteria were recovered from the intraoperative culture specimens. The fungal elements noted on Gram stain were assumed to be a contaminant, but considering the patient’s immunocompromised state, a short course of antifungal therapy was completed.
The pathology report identified the lytic lesion as a high-grade adenocarcinoma, consistent with the known endometrioid ovarian carcinoma (Fig. 3). The specimen was 30% positive for estrogen receptors and negative for progesterone receptors. The patient was diagnosed with metastatic adenocarcinoma consistent with ovarian origin.
The initial postoperative course was uncomplicated. The patient was transferred to a rehabilitation facility, and the chemotherapy regimen was continued. The thumb pain resolved, and the wound healed uneventfully (Fig. 4). A whole-body bone scan was performed, and no additional osseous metastases were identified.
The patient did well until 3 months after surgery, when she noted left shoulder pain in the absence of trauma or injury. Radiographs revealed multiple metastatic lesions in the left humeral shaft. The prognosis remains poor.
Proceed to Discussion >>Reference: Falk DP, Scully R, Moss D, Shaffer M. Pathologic tuft fracture in a thumb: a rare presentation of metastatic endometrioid ovarian carcinoma. A case report and review of the literature. JBJS Case Connect. 2017 Jul 26;7(3):e50.
Osseous metastases to the hand are exceedingly rare; they have an estimated incidence of 0.1% of all metastatic osseous malignancies. When they occur, these tumors most commonly involve the distal phalanx of the middle finger or thumb, and frequently originate from a primary lung tumor. Although Turan et al. described a single case of endometrioid ovarian carcinoma metastasis more than 25 years ago, that case involved the proximal, middle, and distal phalanges of the small finger. A comprehensive review of the literature suggests that our case is the first report of metastatic endometrioid carcinoma to affect the thumb.
Metastatic lesions of the hand are generally diagnosed in patients with a known cancer history, but can be the presenting sign of malignancy in 10% to 30% of cases. These tumors closely resemble infectious or inflammatory processes since they can present with pain, tenderness, and erythema. Serologic studies can further cloud the evaluation because elevated inflammatory markers and leukocytosis are commonly seen with both infectious and malignant bone disease. Features that raise suspicion for malignancy include rapid growth, pain that is worse at night, and the presence of constitutional symptoms such as fever, chills, or weight loss. A fixed mass or a mass deep to the subcutaneous tissue is also concerning for malignancy. Although imaging is critical in the diagnostic evaluation, plain film radiographs may not reveal lesions until 30% to 75% of trabecular bone has been destroyed. Skeletal scintigraphy is often used in the assessment of bone metastasis because an abnormality can be detected with only a 5% to 10% change in normal bone structure. However, supportive imaging with computed tomography (CT) or MRI is recommended, given that the tracer from scintigraphy can also accumulate in bone subjected to trauma or infection. Ultimately, open biopsy is the gold standard for diagnosis. Although these tumors are rare, it is essential to consider malignancy in patients presenting with symptoms classically associated with infection in order to promptly initiate treatment and optimize patient outcomes.
Metastatic lesions of the hand are most commonly caused by primary lung cancers, with an estimated incidence of 34% to 44% of all metastatic hand malignancies. Given this association with lung cancer, it has been suggested that malignant cells reach the hand via hematogenous spread. Tumor cells from the lungs have direct access to systemic circulation, and are thus less likely to be filtered by the capillaries of the liver or lungs compared with malignant cells derived from other sites.
Regardless of the primary malignancy, the distribution of metastatic hand tumors appears to be linked to hand dominance. Although the exact mechanism is unknown, 2 theories have been postulated to explain this association. The first suggests that an increase in blood flow to the dominant hand facilitates metastatic spread, given the presumption that metastasis to the hand occurs via the hematogenous route. The second hypothesis is based on the concept that the dominant hand is more likely to experience trauma because of its increased use. Release of prostaglandins following injury may facilitate tumor-cell migration and adhesion to bone. Similarly, repeated trauma may impair the resilience of nearby tissue, creating an environment in which tumor cells could invade and proliferate. A history of trauma in patients with metastatic lesions of the hand has been described previously, and was associated with dog bites, pricks from rose thorns, and crush injuries.
Although metastatic hand lesions are particularly uncommon, the skeleton as a whole is the third most frequent site of metastatic involvement from any primary tumor, following the lungs and liver. Within the skeletal system, the distribution of metastasis appears to be influenced by the predominant type of bone marrow at different anatomic locations. Metastatic bone lesions most commonly occur in the axial skeleton, which is rich in red marrow. The vertebral bodies are the most commonly involved site, followed by the sacrum and the pelvis. Much less frequently, malignancies can metastasize to the appendicular skeleton, which is rich in fatty marrow and poor in red marrow. This difference is likely attributed to the greater vascularity of red marrow relative to fatty marrow, as the increased blood supply can facilitate tumor-cell migration.
Among women, the most common primary tumor to metastasize to bone is breast cancer, followed by lung, kidney, and thyroid cancers. Bone metastasis from epithelial gynecologic malignancies, as in our patient, is rare. In clinical studies, the incidence of skeletal metastases from epithelial ovarian cancer is estimated to be between 0.7% to 3.3%, with the most common locations including the vertebral bodies, the ribs, the clavicle, the skull, and the femur.
We know of only 1 prior case of endometrioid ovarian carcinoma that metastasized to the hand. Turan et al. described the case of a 43-year-old woman who presented with tenderness and swelling of the right little finger. She was initially diagnosed with a nondisplaced fracture based on plain radiographs, although the diagnosis was changed to osteomyelitis when radiographs at the 6-week follow-up revealed complete resorption of the middle phalanx in the setting of an elevated ESR. However, angiography demonstrated pathologic vessels encasing the entire little finger. She was later found to have endometrioid ovarian carcinoma, and died from a pulmonary embolism shortly after an oophorectomy.
This case report emphasizes that metastatic bone lesions can mimic both trauma and infection. Given the similarities in presentation, it is essential to consider a broad array of diagnoses in patients presenting with painful, swollen, or bruised fingers to avoid diagnostic pitfalls and to treat patients both promptly and appropriately.
Reference: Falk DP, Scully R, Moss D, Shaffer M. Pathologic tuft fracture in a thumb: a rare presentation of metastatic endometrioid ovarian carcinoma. A case report and review of the literature. JBJS Case Connect. 2017 Jul 26;7(3):e50.
What is the diagnosis?
Fungal osteomyelitis
Metastatic adenocarcinoma consistent with ovarian origin
Granulomatous inflammation, suggestive of sarcoidosis
Inflamed epidermal inclusion cyst
Synovial sarcoma



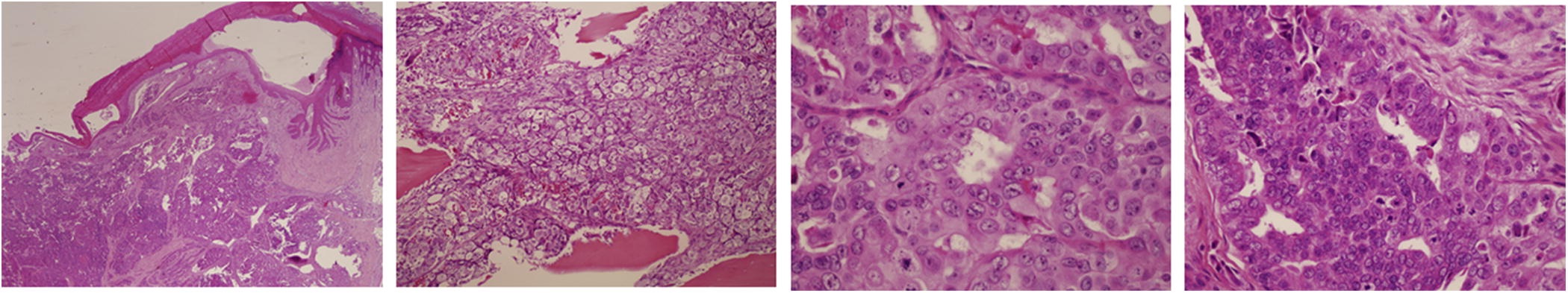
 Fig. 1
Fig. 1 Fig. 2
Fig. 2![Fig. 3 Fig. 3 Histology of the amputation specimen (hematoxylin and eosin, ×4 [2 left images] and ×20 [2 right images]).](https://quiz.jbjs.org/wp-content/uploads/2017/11/iqnov17-1_fig3-150x150.jpeg) Fig. 3
Fig. 3 Fig. 4
Fig. 4