A 58-Year-Old Woman with Progressive Extremity Weakness
June 6, 2018
A fifty-eight-year-old woman was evaluated in April 2012 for progressive upper and lower-extremity weakness. She was diagnosed with a retropharyngeal abscess from C2 to C4 with an epidural component extending from the tip of the C2 vertebral body down to the C2-C3 disc space. In addition, the C6-C7 disc appeared to be involved distally, although there was no epidural component found at this level. She underwent an emergency debridement, discectomy, and partial corpectomy at C2 and C6-C7, with fusion using iliac crest bone graft, and was placed in a halo vest. Two days later, she underwent C1 to C7 anterior-posterior cervical decompression and fusion with local bone graft (Figs. 1, 2, and 3). The subaxial spine was stabilized with 3.5 × 12-mm lateral mass screws, a 3.5 × 16-mm isthmic screw placed at C2, and 3.5 × 30-mm partially threaded lateral mass screws in C1 using the Harms technique. The infection resolved, and she had an unremarkable postoperative clinical course and was lost to follow-up after six months.
Two years after the posterior stabilization, the patient presented to the emergency department with a four-day history of slurred speech, tongue weakness, and tongue deviation to the left side. A full neurologic workup was performed. Magnetic resonance imaging (MRI) of the brain was negative for acute infarction, metastatic disease, or a mass effect. A computed tomographic (CT) scan of the head and cervical spine is shown in Figs. 4 and 5. She presented with no other acute neurologic symptoms, weakness, or paresthesias.
Imaging studies were interpreted as showing cranial migration of bilateral C1 lateral mass screws with erosion of the left screw through the lateral mass of the atlas and impingement of the hypoglossal canal on the left. These findings corresponded with her clinical presentation of focal denervation of the genioglossus muscle.
She was taken back to the operating room and underwent removal of the C1 screws with extension of the posterior fusion to the occiput. Three months postoperatively, the patient had improved clinically with resolution of the preoperative dysphagia and dysarthria. She reported better control of her tongue but still had partial left deviation with full tongue protrusion.
Proceed to Discussion >>Reference: Hollern D, Shafi K, Miller A, Woods B, Heller J, Vaccaro A. C1 lateral mass screw migration causing a delayed unilateral hypoglossal nerve lesion: a case report. JBJS Case Connect. 2016 Jan-Mar;6(1):e15.
Iatrogenic neurologic sequelae following posterior cervical instrumentation have been well documented in the literature, with injuries to the cranial nerves being a rare occurrence. The most common cranial nerve injuries following cervical spine surgery are of the facial and glossopharyngeal nerves. The hypoglossal nerve exits the hypoglossal canal adjacent and lateral to the foramen magnum and travels dorsal to the internal carotid artery, passing just lateral to the ventral midportion of the C1 lateral mass, prior to innervating the genioglossus muscle. Injuries to this nerve result in denervation of the muscle and ipsilateral deviation of the tongue, and patients may also present with dysphagia, dysarthria, and hypersalivation. Hypoglossal nerve palsy has been reported in association with a variety of circumstances, including trauma, brain-stem malformations, perioperative airway management, infection, rheumatoid arthritis, and cervical traction as well as following cervical spine surgery.
Hypoglossal nerve palsy has been reported following both anterior and posterior cervical procedures. The rate of hypoglossal nerve palsy is much higher during procedures that require substantial soft-tissue dissection in the anterior triangle of the neck. Open carotid artery procedures have a particularly high rate of hypoglossal nerve injury, with deficits observed in 8.6% of patients in one series. Hypoglossal nerve palsy following cervical spine surgery is very rare, with only a few case reports documenting this complication. Sengupta et al. described a hypoglossal nerve injury as a result of anterior cervical corpectomy and fusion from C2 to C5 for tuberculosis. The palsy presented in the acute postoperative period and was thought to be from traction neurapraxia. At eighteen months of follow-up, the patient still had denervation of the genioglossus resulting in ipsilateral deviation but with minimal functional deficit. Saunders et al. described a hypoglossal palsy as an isolated complication following an anterior cervical corpectomy for treatment of cervical myelopathy. The palsy was reported in the postoperative period with ipsilateral deviation of the tongue. The timeline of that hypoglossal nerve palsy and its functional implications for the patient were not documented. Bicortical fixation of the C1 lateral mass places the hypoglossal nerve at risk because of its ventral location on the axis. This has been demonstrated following transarticular fixation with violation of the anterior cortex of the C1 lateral mass. Jeanneret et al. noted a hypoglossal palsy that presented forty-eight hours following treatment of an odontoid fracture using transarticular screw fixation. The patient was found to have violation of the C1 ventral cortex, underwent revision with a short screw, and had complete resolution of the hypoglossal palsy at three months of follow-up. Another patient, reported by Grob et al., developed a hypoglossal paresis, again thought to be attributable to excessive screw length, which resolved on revision to a shorter screw. Hong et al. reported the case of a sixty-seven-year-old man who sustained a Type-2 dens fracture that failed to fuse following initial treatment in a halo vest for four months. He had no preoperative neurologic deficits and was subsequently treated with a Harms fusion. Postoperatively, he was found to have dysphagia and left-sided tongue deviation. Imaging confirmed accurate placement of the C1 screws bilaterally; however, the left C1 screw was bicortical and was found to be abutting the internal carotid artery. The patient required prolonged nasogastric tube feeding postoperatively but had complete resolution of the hypoglossal palsy at eight weeks of follow-up. No further surgery was performed on that patient. Propst et al. reported a case in which a patient with a retropharyngeal abscess presented with a hypoglossal nerve palsy, which subsequently resolved following surgical debridement and antibiotics. It should be noted that our patient did have a remote history of retropharyngeal abscess; however, the temporal course of her palsy corresponded with screw migration and nerve impingement. Her infection had been treated and had resolved by the time she presented with the cranial nerve lesion.
The patient in the present case demonstrated a delayed presentation of hypoglossal nerve palsy nearly two years following posterior cervical stabilization using C1 lateral mass screws. The accuracy of screw placement was confirmed intraoperatively using fluoroscopy and postoperatively with both MRI and CT scanning. The patient was noted intraoperatively to be osteoporotic. Her condition improved and was following an unremarkable clinical course until her return to the emergency room two years postoperatively with progressive dysphagia. We hypothesize that her osteoporosis, along with settling of the fusion mass, facilitated the cranial migration of the C1 screw through the lateral mass on the left, compressing the hypoglossal nerve at the hypoglossal foramen. This resulted in the dysphagia, tongue weakness, and tongue deviation experienced by this patient. Following removal of the C1 screws and extension of the fusion to the occiput, her dysarthria and dysphagia improved, but she still experienced some tongue deviation with full protrusion.
Delayed cranial neuropathy is an extremely rare complication of posterior cervical stabilization; however, bone mineral density, screw length, and screw angulation can be important factors in the development of this complication. Most of the few hypoglossal nerve palsies documented in the literature following transarticular or C1 lateral mass instrumentation occurred in the acute perioperative period and were due to violation of the ventral cortex of C1. This is the first report of which we are aware of a hypoglossal nerve palsy occurring in a delayed fashion and secondary to cutout of a C1 screw resulting in cephalad migration and impingent on the nerve lateral to the foramen magnum. Surgeons should be aware of this potential complication in patients who have poor bone quality and require lateral mass fixation in the C1 vertebra.
Reference: Hollern D, Shafi K, Miller A, Woods B, Heller J, Vaccaro A. C1 lateral mass screw migration causing a delayed unilateral hypoglossal nerve lesion: a case report. JBJS Case Connect. 2016 Jan-Mar;6(1):e15.
What is the diagnosis?
Retropharyngeal abscess with hypoglossal nerve palsy
Erosion of the left C1 screw through the lateral mass of the atlas
Aberrant path of left vertebral artery
Probable nerve sheath tumor (schwannoma) of hypoglossal nerve
Hypoglossal nerve palsy due to a broken 3.5-mm screw at C2




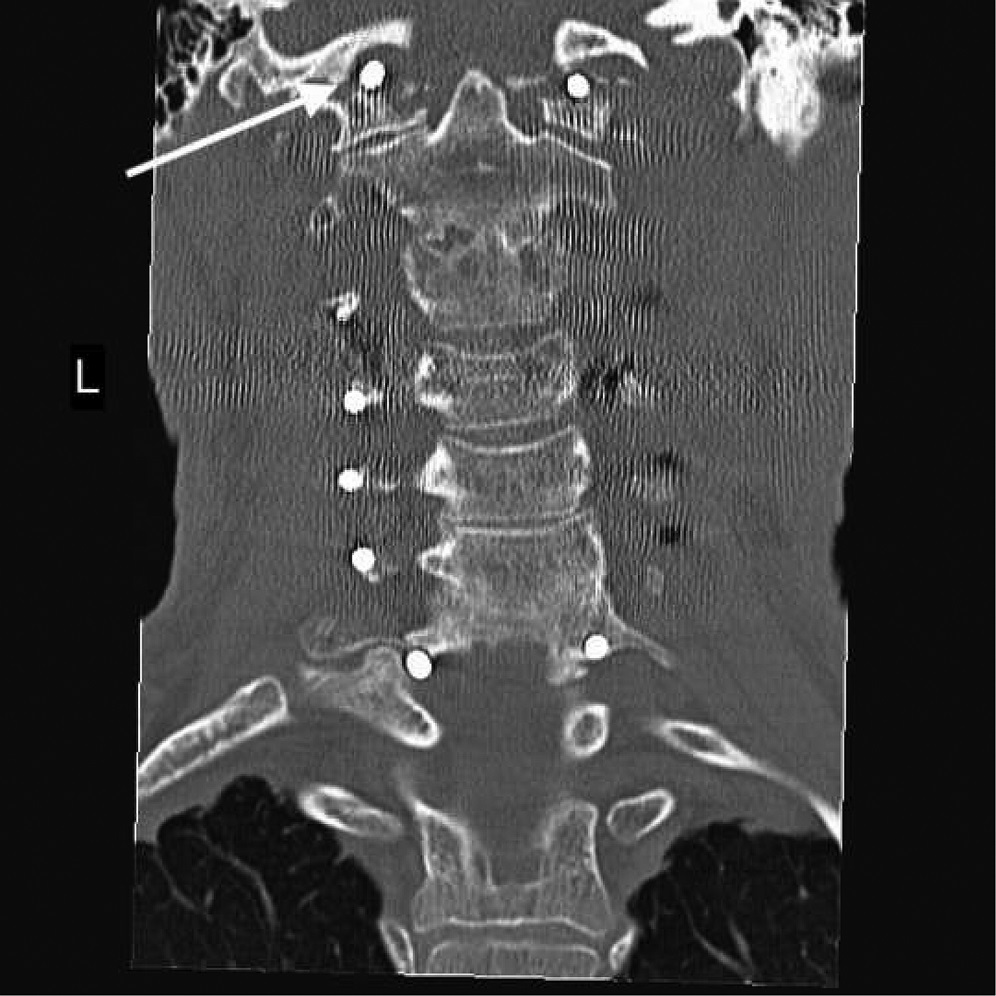

 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5