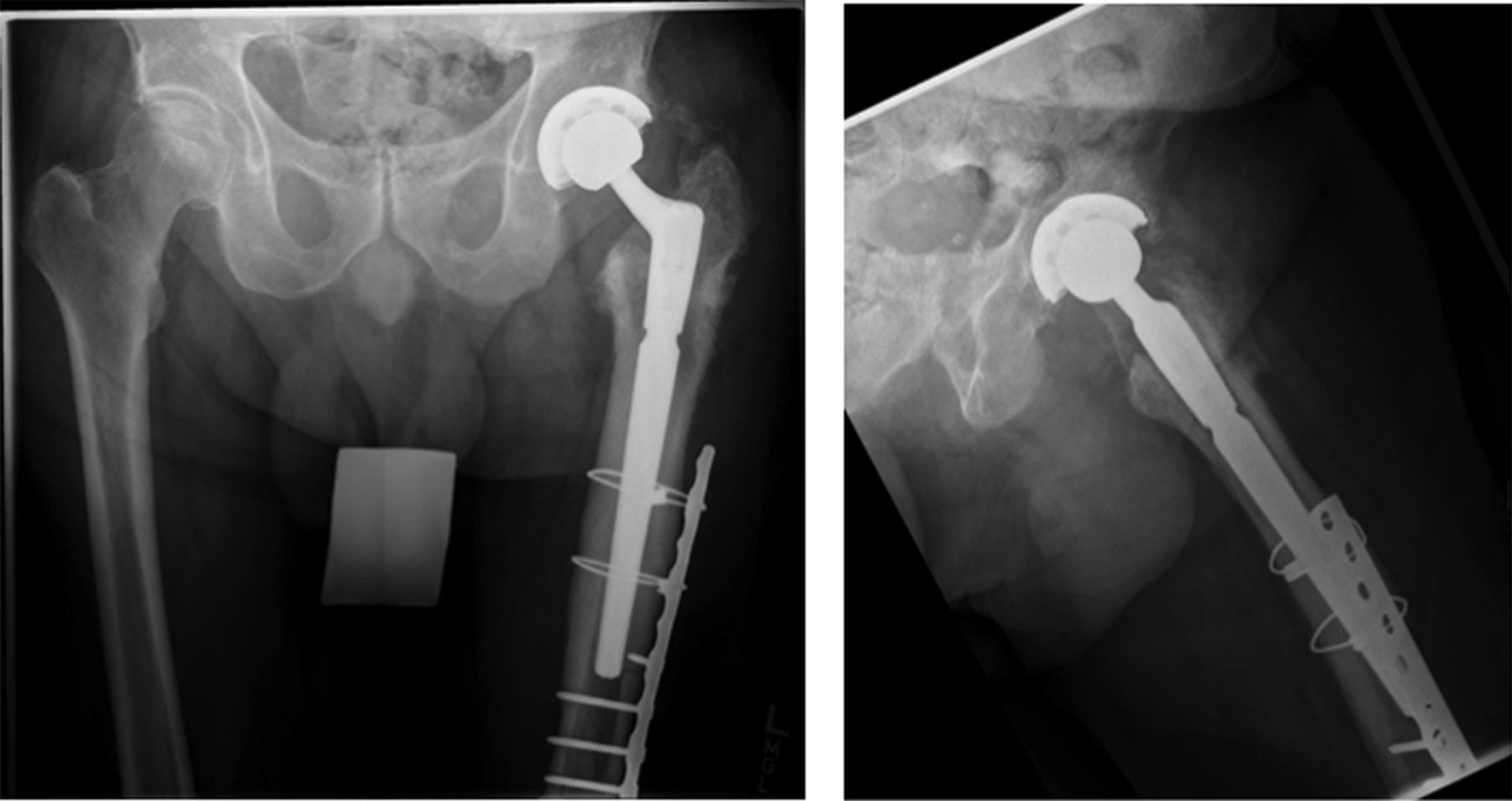
A seventy-seven-year-old white man with a history of sarcoidosis, primary biliary sclerosis, and chronic renal insufficiency, as well as a family history of hyperparathyroid disease, presented to our clinic with left hip pain. Two years prior to presentation, he had undergone left total hip arthroplasty for posttraumatic osteoarthritis at an outside facility. He had been involved in a motor vehicle accident two years prior to that surgery. No fracture or dislocation had been noted at the time of the accident, but he had experienced increasing left hip pain after the event, and there had been rapidly progressive radiographic changes. Preoperative radiographs (Fig. 1) had shown osteonecrosis of the femoral head with segmental collapse and secondary osteoarthritis. A cementless total hip arthroplasty was implanted with satisfactory initial fixation with use of a Stryker Accolade size-3 femoral stem, a 58-mm Trident cup, a 36-mm cobalt-chromium femoral head, and a highly cross-linked X3 polyethylene liner. The patient reported complete resolution of the preoperative symptoms. Radiographs at six months postsurgery had shown normal bone morphology and no evidence of subsidence (Fig. 2). Over the next twelve months, he remained asymptomatic.
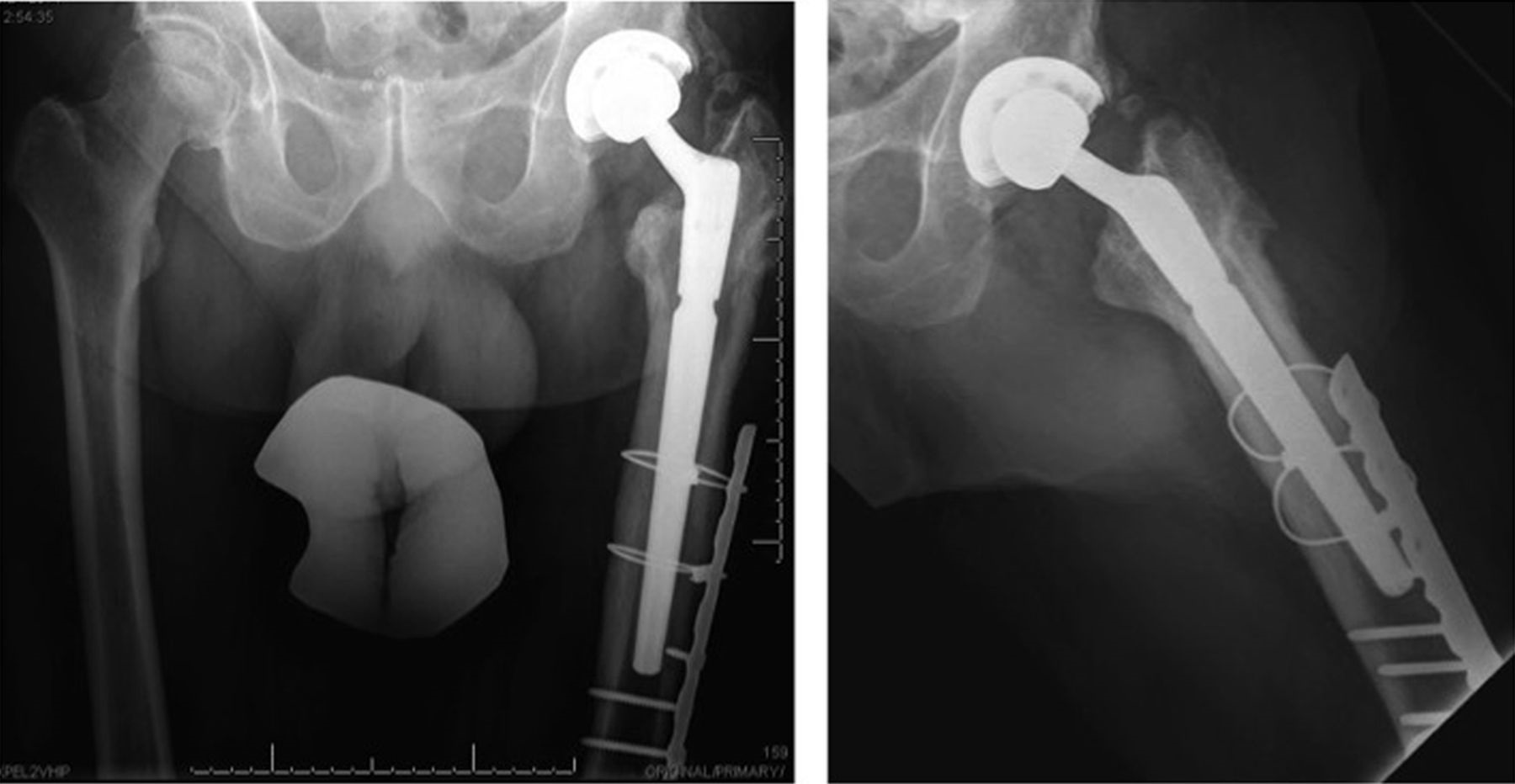
Eighteen months after the original procedure, the patient had insidious onset of pain in the left hip. Around that time, he also noticed a mass on the proximal aspect of the right tibia. He was referred to our clinic; radiographs of the left hip demonstrated femoral component subsidence with cortical thickening, periostitis, and expansion of the greater trochanteric region (Fig. 3). Radiographs of the right tibia showed an expanded mixed lytic and sclerotic lesion of the anterior tibial cortex extending from the proximal articular surface to the midshaft (Fig. 4). On physical examination, he had a 10-cm × 3-cm firm, nontender mass over the proximal tibial crest. Magnetic resonance imaging (MRI) of the left femur was consistent with osteitis and adjacent soft-tissue inflammation. A technetium-99m bone scan on the same day showed focal areas of increased activity in the proximal half of the left femur and the right tibia (Fig. 5). Aspiration of the hip provided no white blood cells or organisms on Gram stain, and the fourteen-day extended culture had no growth. Laboratory markers were normal, including white blood-cell count (9.5 × 103 cells/μL), C-reactive protein level (5 mg/L), and erythrocyte sedimentation rate (11 mm/h). Because the infection workup was negative, the patient was referred to an endocrinologist for additional evaluation.
Additional laboratory studies were recommended. A complete metabolic panel, including alkaline phosphatase, liver function enzymes, parathyroid hormone, calcium, phosphate, thyroid stimulating hormone, vitamin D panel, and urine calcium levels, was done. The creatinine was elevated at 1.6 mg/dL; otherwise, there were no substantial abnormalities. Of note, although the alkaline phosphatase level was normal, it had previously been elevated. A dual x-ray absorptiometry scan showed a T-score of −2, signifying osteopenia.
After ruling out metabolic disease, our presumptive diagnosis was Paget disease of bone. One month prior to surgery, the patient was started on a renal adjusted dose of zoledronic acid (Reclast) (3 mg intravenous infusion annually).
The patient was taken to the operating room twenty-six months after the original surgery for femoral stem revision and bone biopsy. Intraoperatively, the femoral component was loose and easily removed. No substantial bone defect was encountered, and grafting was not required. Our goal was to bypass the area of diseased bone to obtain diaphyseal fixation on healthy bone with use of an uncemented grit-blasted modular revision prosthesis. Reaming of the canal was extremely difficult because of the sclerotic nature of the femur. This led to a breach of the anterior femoral cortex, which necessitated reinforcement with a cable-plate construct after bypassing the defect with the stem (Fig. 6). We used the Stryker Restoration Modular total hip system with a 19-mm × 150-mm conical femoral stem, a 21-mm conical body, and a 36-mm cobalt-chrome femoral head. We replaced the acetabular liner with highly cross-linked X3 polyethylene. We used a Synthes large-fragment twelve-hole plate fixed with 4.5-mm cortical screws and stainless steel cables. This construct bypassed the diseased bone and stabilized the fracture. Bone biopsies of the left femur were sent to pathology. Microscopic examination revealed fragments of mixed-phase woven and lamellar bone, consistent with Paget disease.
At four weeks postoperatively, the patient was walking with minimal discomfort with use of a cane for balance. Three months after surgery, he was making good progress with physical therapy and had returned to baseline ambulatory status. At the two-year follow-up, there was no evidence of implant loosening, subsidence, or fracture on radiographs (Fig. 7). There was also no radiographic progression of the tibial or the femoral lesions, and he remained pain-free. He has continued zoledronic acid therapy as long-term treatment for Paget disease.
Proceed to Discussion >>Reference: Amundsen S, Koenig K, Goodwin D, Memoli V. Failure of primary total hip arthroplasty secondary to new onset of Paget disease: a case report. JBJS Case Connect. 2015 Jan-Mar;5(1):e19.
To our knowledge, there are no other published reports documenting the diagnosis of Paget disease of bone causing component subsidence and loosening after total hip arthroplasty. As with any revision arthroplasty procedure, an appropriate workup is critical prior to returning to the operating room. The workup should include radiographs and additional imaging such as computed tomography, a bone scan, or MRI to determine loosening of the implant, bone destruction, or neoplastic processes. Infection markers, including complete blood-cell count with differential, erythrocyte sedimentation rate, and high-sensitivity C-reactive protein, should be obtained, as well as aspiration of the joint (when indicated); the fluid should be sent for Gram stain, culture, and cell count.
We were concerned about our ability to definitively confirm the diagnosis of Paget disease by intraoperative microscopy or with a preoperative biopsy. Therefore, we sought to solidify the diagnosis as much as possible and attempted to rule out neoplasm prior to surgery. A combination of bone scan findings, MRI findings, and the radiographic character of the tibial lesion were evidence enough to make our multidisciplinary team comfortable with proceeding to the operating room. We recommend good communication with the pathology service to ensure that proper samples are obtained for confirmation of the diagnosis during surgery.
In cases of suspected Paget disease, an endocrinology referral should be made to rule out metabolic bone disease. The diagnosis of Paget disease of bone should be discussed with the patient when making a decision to operate. Bisphosphonate treatment may be initiated prior to surgery in order to maximize the chance of obtaining appropriate fixation. The effect on osteointegration or long-term implant stability from the dose of zoledronic acid that our patient received is unknown. Bisphosphonates have been shown to increase the cellular response in both mature and healing bone, and zoledronic acid has demonstrated enhanced bone growth into porous implants in animal models. Additional studies on this subject are needed.
Suspected Paget disease of bone also necessitates careful preoperative planning as well as proper implant and equipment availability. With our patient, we discussed the possibilities of long cemented stems, cylindrical fully porous-coated stems, or modular revision stems with conical grit-blasted diaphyseal fixation. Given the possibility of progressive Paget bone remodeling and possible bone loss, we felt that bypassing the lesion with diaphyseal fixation in healthy bone was paramount. We decided against cemented fixation based on the low likelihood of good cancellous bone for cement interdigitation in the revision setting, as well as the possibility of continued remodeling due to Paget disease that might leave portions of the construct unsupported and eventually fracture the cement mantle. Considering the two remaining options, we felt that the femoral canal deformity and secondary sclerotic change would be more amenable to a conical stem rather than a cylindrical stem. We also felt that the ability to independently match the proximal and distal stem geometry to the available bone would be an advantage in this case. We had cortical strut graft and cancellous bone graft available in the event of bone loss, but were more concerned about the possibility of sclerotic changes in the femoral canal. We were able to bypass the Paget disease with our stem fixation and obtained good fixation in healthy bone with a stable construct after plating and cabling the femoral breach.
In conclusion, Paget disease of bone, while rare, may be responsible for the loosening of arthroplasty components. An appropriate workup prior to surgery is necessary to rule out other conditions and to formulate an appropriate operative plan if revision surgery is undertaken.
Reference: Amundsen S, Koenig K, Goodwin D, Memoli V. Failure of primary total hip arthroplasty secondary to new onset of Paget disease: a case report. JBJS Case Connect. 2015 Jan-Mar;5(1):e19.
What is the diagnosis?
Particle-induced osteolysis
Multifocal osteomyelitis
Aseptic lymphocyte-dominant vasculitis associated lesion associated with head and neck corrosion
Paget disease
Hyperparathyroidism


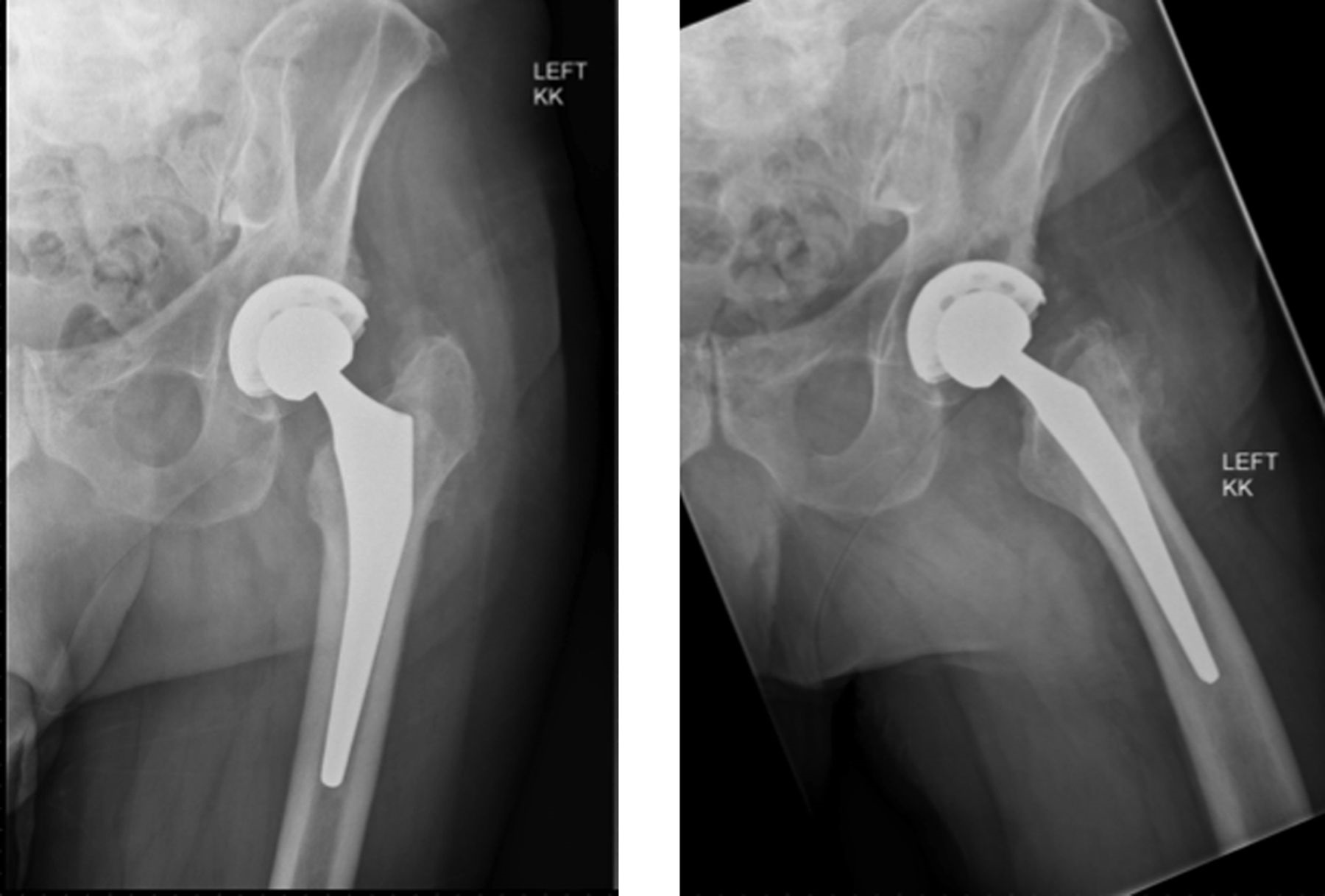
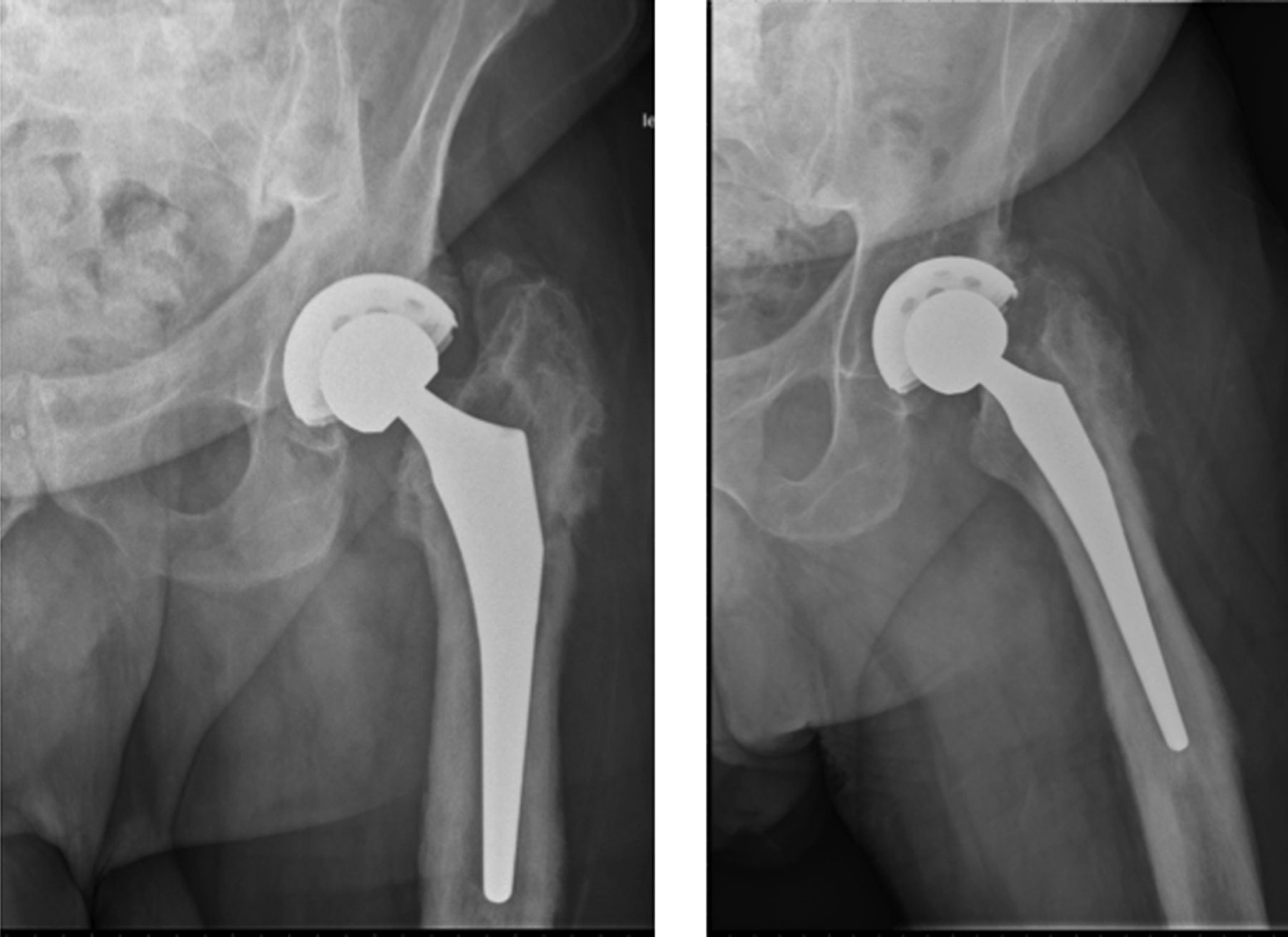

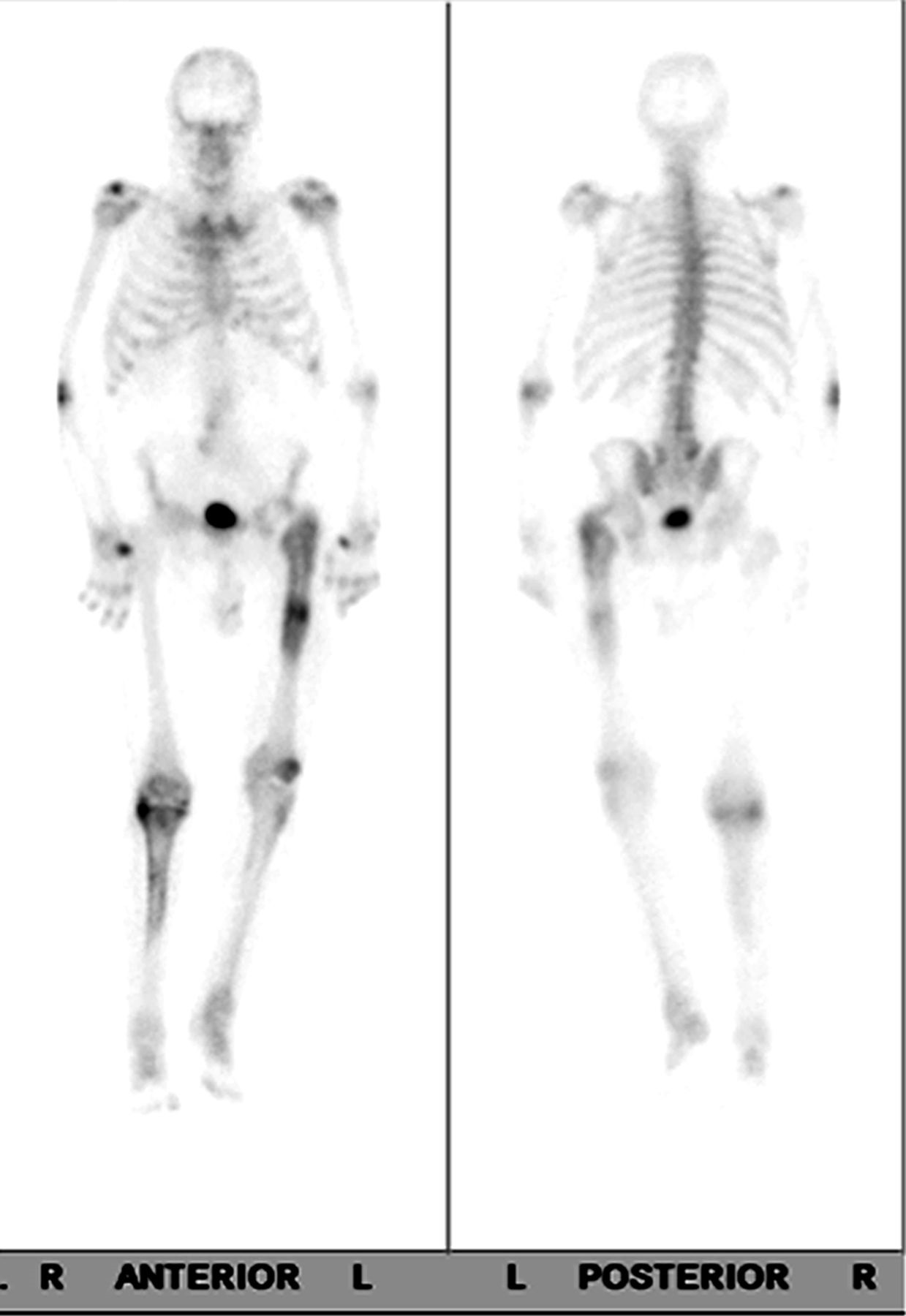
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7