In September 2010, an 81-year-old woman presented to the outpatient orthopaedic clinic with several weeks of left knee pain. The patient previously had had a left total knee replacement in 1996 (revised in 1999), a left hip replacement in 1999, and a right hip replacement in 2001. Both hip replacements had included extensively coated femoral components. She had a history of osteoporosis and had been on alendronate therapy (70 mg weekly) from May 2006 to May 2010. She had transitioned to ibandronate therapy (150 mg monthly) for the 4 months prior to presentation to us.
Because the knee prosthesis was 11 years old at the time of initial evaluation, it was suspected that the pain was caused by polyethylene wear. When the patient was seen for follow-up in December 2010, she reported continued knee pain as well as occasional soreness in the thigh. Work-up was negative for polyethylene wear and aseptic loosening, but radiographs revealed cortical thickening, beaking, and a horizontal fracture line near the tip of the left femoral prosthesis (Fig. 1). While beaking on the right lateral cortex near the tip of the prosthesis was also found, increased uptake was not seen on the right on bone scans and there were no symptoms on this side. The patient was started on protected ambulation with a walker with anticipated follow-up in 2 months.
In March 2011, the patient had a fall from standing height. She stated that she had been walking in a restaurant and suddenly felt the left leg “give out.” A radiograph revealed that the fracture had occurred at the location of the previous cortical reaction (Fig. 2-A).
Based on the radiographic appearance and the patient’s history of osteoporosis and long-term bisphosphonate use, the findings were interpreted as a periprosthetic fracture likely related to bisphosphonate use.
The fracture was fixed with use of a 4.5-mm locking plate secured by multiple cables, locked screws proximally, and nonlocked screws distally (Fig. 2-B). Because the right side had remained asymptomatic with only radiographic findings of a cortical reaction, the patient was instructed to avoid vigorous activity and to report any subsequent pain on the right side. Bisphosphonates were discontinued, and at the ten-week follow-up, the patient was doing well with full weight-bearing on the left side; she remained pain-free on the right side.
Proceed to Discussion >>Reference: Chen F, Bhattacharyya T. Periprosthetic fracture of the femur along the long-term bisphosphonate use: a case report. JBJS Case Connect. 2012 Apr-Jun;2(2):e21.
The rising incidence of subtrochanteric fractures is concerning given the growing usage and increasing duration of bisphosphonate therapy in the elderly population. The current hypothesis for the cause of this atypical fracture includes a combination of the effects of suppressed bone turnover and repetitive stress. In most individuals, the site of maximal stress occurs in the subtrochanteric region. Patients are often on bisphosphonate therapy for 5 to 10 years prior to their fractures. They may experience prodromal pain in the groin or thigh for several months, and, suddenly, they may experience an insufficiency fracture following low-energy trauma, often a fall from standing height.
The dynamics change, however, when patients receive a femoral implant. Proximally, the femur experiences stress shielding, and, distally, the femur experiences stress concentration on the lateral cortex, especially in the case of a well-fixed, extensively coated femoral component. This region presents a high-stress transition zone between the relatively stiff femur proximally and the osteopenic femur distally. Previous case series of atypical femoral fractures have included some periprosthetic fractures.
To our knowledge, this is the first case of a periprosthetic fracture reported in a patient with long-term bisphosphonate use in whom bilateral femoral implants were present and bilateral cortical reactions at the implant tips were observed. The bilateral radiographic features and the sudden low-energy event are characteristic of atypical femoral fractures in these patients. We believe that our case represents an example of the systemic process seen with long-term use of bisphosphonates. As the stresses are pushed distally on the femur, the same interference with bone turnover that results in atypical femoral fractures may cause a more periprosthetic fracture distal to an ingrown fully coated femoral prosthesis.
While intramedullary nailing is the preferred method of treatment in atypical femoral fractures, the presence of a femoral prosthesis necessitates the use of a spanning plate construct. In our case, the proximal lateral cortex was markedly thin, and a combination of locked screws and cables was necessary to obtain adequate fixation.
As per the ASBMR Task Force recommendations, the contralateral femur must be evaluated when a complete atypical fracture presents, and prophylactic fixation is recommended when incomplete fractures are accompanied by pain. For those with incomplete fractures or stress reactions, bisphosphonates should be discontinued; the indication for prophylactic fixation is the presence of pain. Because our patient had a stress reaction without pain, the asymptomatic side was managed with vigorous activity avoidance, and she was instructed to report any subsequent pain.
The atypical subtrochanteric hip changes and fractures experienced by long-term bisphosphonate users may be the result of a combination of the systemic bone suppression coupled with the biomechanics of the femur. Our case provides an interesting situation, where the altered biomechanics of femoral implants led to changes in the fracture location, although there were consistencies in the radiographic findings and presenting symptoms. This case reinforces the biomechanical hypothesis and highlights the need for arthroplasty surgeons to consider stress fracture as a cause of thigh pain after total hip replacement, particularly in patients on bisphosphonate therapy.
Reference: Chen F, Bhattacharyya T. Periprosthetic fracture of the femur along the long-term bisphosphonate use: a case report. JBJS Case Connect. 2012 Apr-Jun;2(2):e21.
What is the diagnosis?
Periprosthetic fracture likely related to bisphosphonate use
Periprosthetic fracture likely related to polyethylene wear debris
Paget disease with fracture
Adverse local tissue reaction
Traumatic fracture associated with osteoporosis

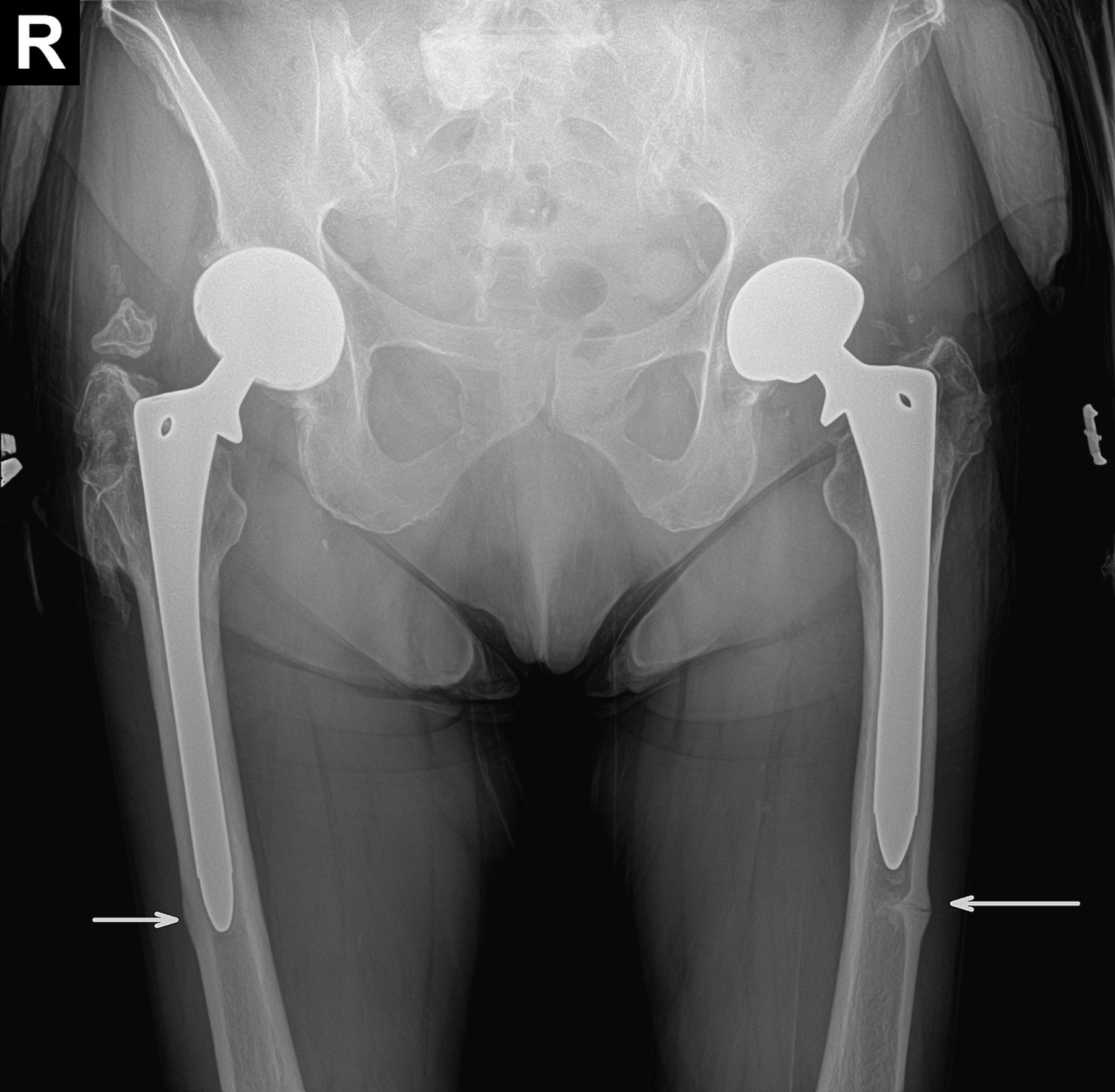

 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B