A Twenty-nine-Year-Old Woman with a Mass on the Left Hand
June 4, 2014
A twenty-nine-year-old woman with a history of Sjögren syndrome and psoriasis sought evaluation of a discolored mass on the ulnar side of the left hand. She had been aware of the mass for three months. She reported mild pain at the site of the mass. She also described generalized pain and numbness in the hand with typing and brushing her teeth. The physical examination revealed a slightly elevated, light blue-red mass measuring 2 cm in diameter, located at the junction of the glabrous and nonglabrous skin of the ulnar border of the hand, beginning 1 cm distal to the wrist crease (Fig. 1). The Phalen test was positive at twenty seconds. Two-point discrimination and median innervated intrinsic strength were normal. MRI revealed a T2 hyperintense, T1 hypointense subcutaneous mass of the hypothenar eminence. The mass was lobular and tubular in morphology with septations. It encased a main branch from the basilic vein and had the appearance of a feeding vessel. The transverse carpal ligament appeared thickened (Figs. 2-A and 2-B). Electrodiagnostic studies were consistent with carpal tunnel syndrome on the left side. The patient underwent left carpal tunnel release with no complications. Via a separate incision, the mass was incised. To our surprise, the mass was rather bland and unimpressive in appearance. The elevated skin and underlying soft tissue were completely excised and submitted for histologic evaluation.
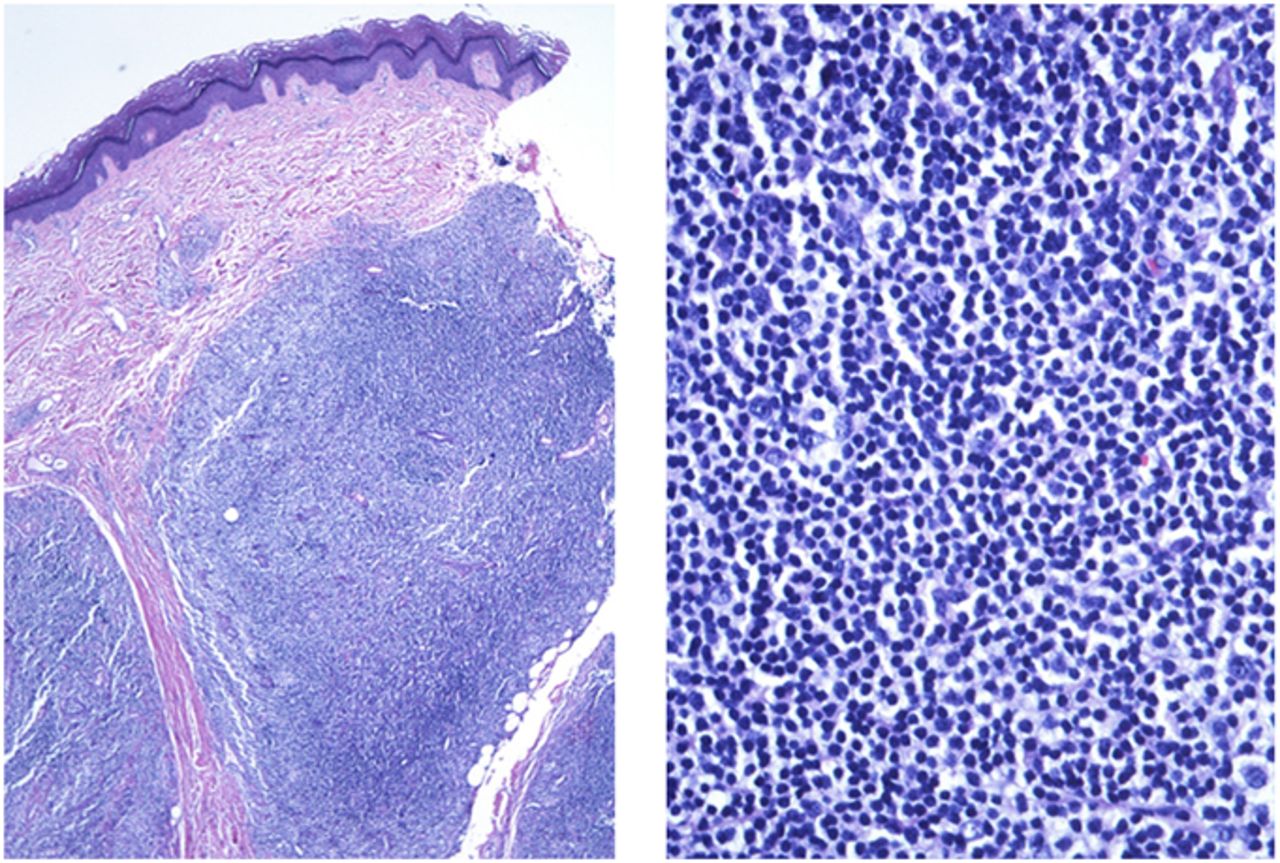
Pathologic analysis revealed dense and atypical lymphoid infiltrate in the deep dermis, consisting of predominantly small cells, the vast majority of which were CD20, CD79a positive (confirming a B-cell phenotype), and CD10 negative (Fig. 3). A few lymphoma cells stained for CD138, showing plasmacytic differentiation. B-cell rearrangement polymerase chain reaction studies showed a clonal peak. A diagnosis of primary cutaneous marginal zone B-cell lymphoma (PCMZL; Ann Arbor Stage 1E) was made. The patient reported decreased pain postoperatively and improvement in the symptoms related to carpal tunnel syndrome. She was referred to the oncology service for additional workup. Surveillance computed tomography (CT) scans of the chest, abdomen, and pelvis were obtained and were initially negative for additional lesions. However, at five months postoperatively, a mass in the soft palate was detected and resected; the pathology was positive for marginal zone B-cell lymphoma. As a result, the patient underwent four cycles of single-agent chemotherapy with rituximab. There has been no recurrence of disease or new lesions, and the patient remained asymptomatic at the nine-month follow-up.
Proceed to Discussion >>Reference: Yu AL, Omman R, Song AJ, Light TR. Cutaneous B-cell lymphoma presenting as a hand mass: a case report. JBJS Case Connector. 2014 Jan 08;4(1):e2
To our knowledge, cutaneous B-cell lymphoma (CBCL) in the hand has not been previously reported. Two cases of cutaneous T-cell lymphoma (CTCL) occurring in the hand have been published. One of these cases was exophytic in appearance, while the other was ulcerative. Our patient presented with a small, slightly elevated discolored mass distorting the skin. Although CTCL is more common than CBCL (71% versus 29%, respectively), like CBCL, CTCL rarely presents in the upper extremity (11.3% versus 11.9%, respectively). CBCLs are further categorized into three groups: primary cutaneous follicle center lymphoma; primary cutaneous large B-cell lymphoma, leg type; and PCMZL. It was determined that our patient had the PCMZL form of CBCL. PCMZL represents 25% of all CBCL cases; it may present with red or violaceous papular or nodular lesions on the trunk or arms, with the majority of cases presenting with multiple lesions. Histopathology of PCMZL reveals nodular or diffuse lymphoid infiltrate separated from the epidermis by an infiltrate-free grenz zone with small to medium-sized cells, representing marginal zone B-cells with plasmacytic differentiation. Plasmacytic cells are usually monoclonal. PCMZLs infiltrate the dermis, but spare the epidermis. Tumor cells typically express CD19, CD20, CD22, CD79a, and/or BCL2, but are negative for BCL6 and CD10. Clonal immunoglobulin heavy chain (IgH) rearrangements are seen in 80% of marginal zone lymphomas. Cutaneous marginal zone lymphomas express IgG, IgA, and IgE, as opposed to other extranodal mucosa-associated lymphoid tissue (MALT) lymphomas, which express IgM. Interestingly, Sjögren syndrome is more commonly associated with MALT lymphomas. Also, there is an association of PCMZLs with Borrelia burgdorferi infection, mainly in European countries where clinical and histologic regression has been observed with treatment of the infection. Extracutaneous disease develops in 8.5%. The overall and disease-specific five-year survival rates are 94% and 98%, respectively. While cutaneous lesions are often diagnosed clinically or histopathologically, imaging can be useful for pretreatment planning. Radiographs of cutaneous lymphomas are often noncontributory, but may show a soft-tissue mass without matrix mineralization. Radiographs can also rule out underlying bone involvement. CT imaging is not commonly performed on superficial soft-tissue lesions. Sonography and Doppler imaging can differentiate a solid from a cystic or vascular lesion. MRI provides the greatest soft-tissue contrast of all imaging modalities. While solid neoplasms are generally hyperintense on T2-weighted images, lymphomas can be intermediate to hyperintense, reflecting a high cellularity. Ultimately, MRI of extranodal lymphoma is nonspecific and is often isointense to muscle on T1-weighted images with diffuse enhancement. Larger or more aggressive lesions may show central necrosis. Treatment for a solitary or small number of lesions is complete surgical excision or radiation therapy. More diffuse disease can be treated with rituximab, radioimmunotherapy, or spot external beam radiation therapy.
Reference: Yu AL, Omman R, Song AJ, Light TR. Cutaneous B-cell lymphoma presenting as a hand mass: a case report. JBJS Case Connector. 2014 Jan 08;4(1):e2
B-cell lymphoma
Giant cell tumor
Glomus tumor
Hemangioma
Arteriovenous malformation

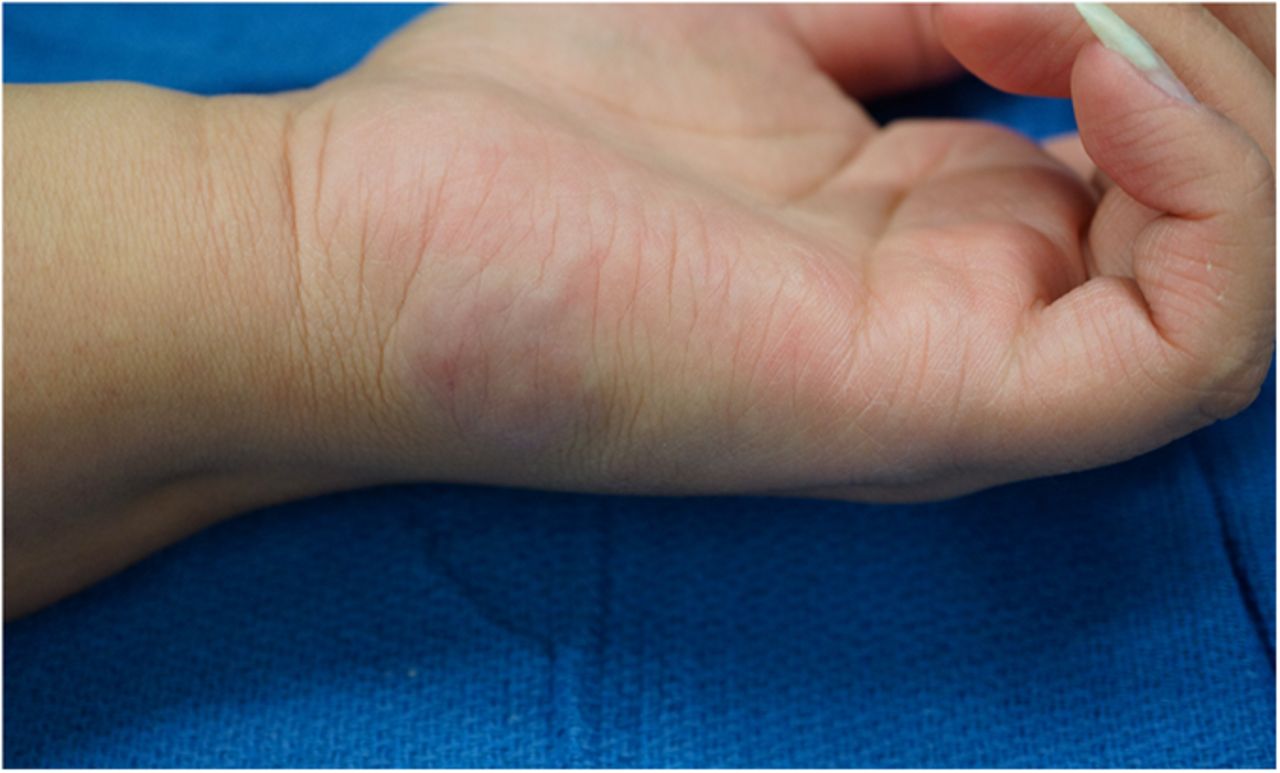
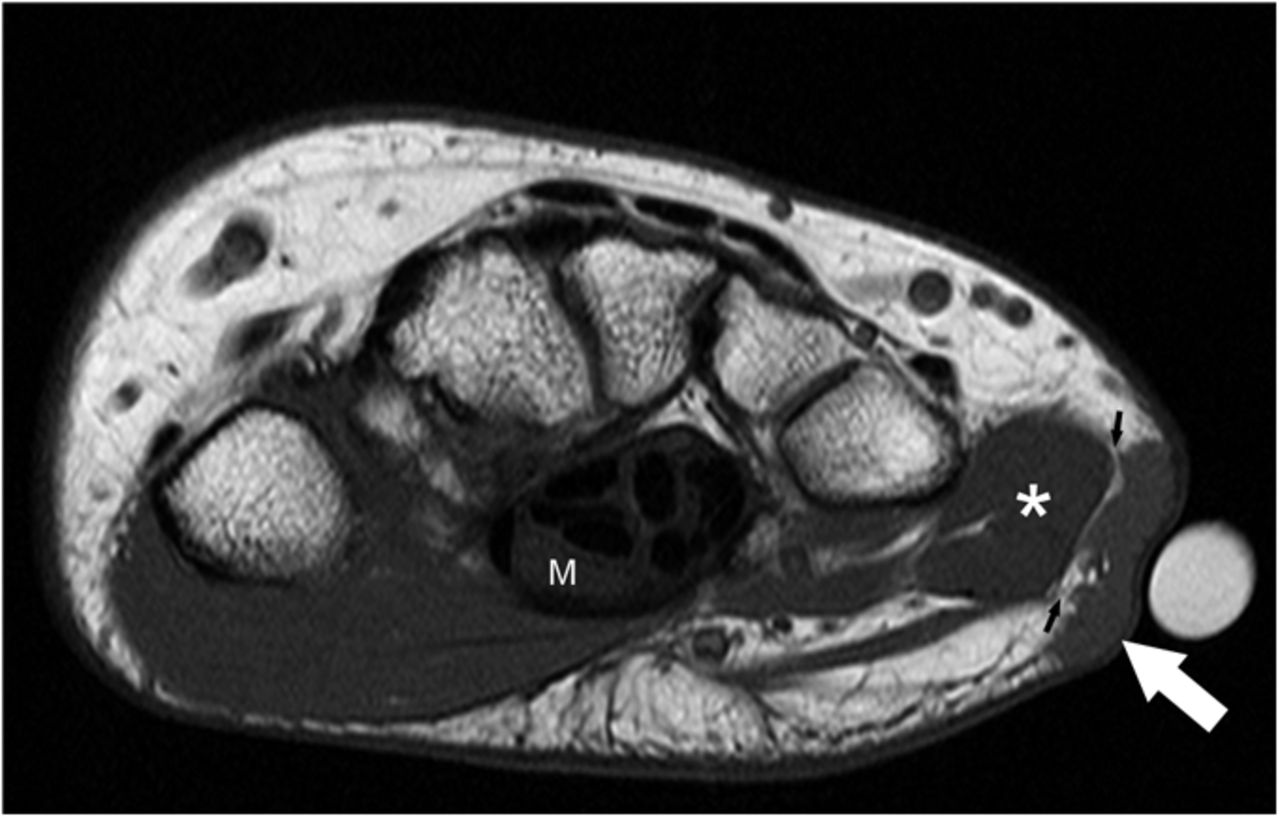

 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B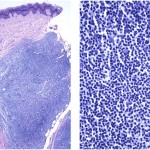 Fig. 3
Fig. 3