A Fifty-three-Year-Old Woman with Hip and Thigh Pain
June 18, 2014
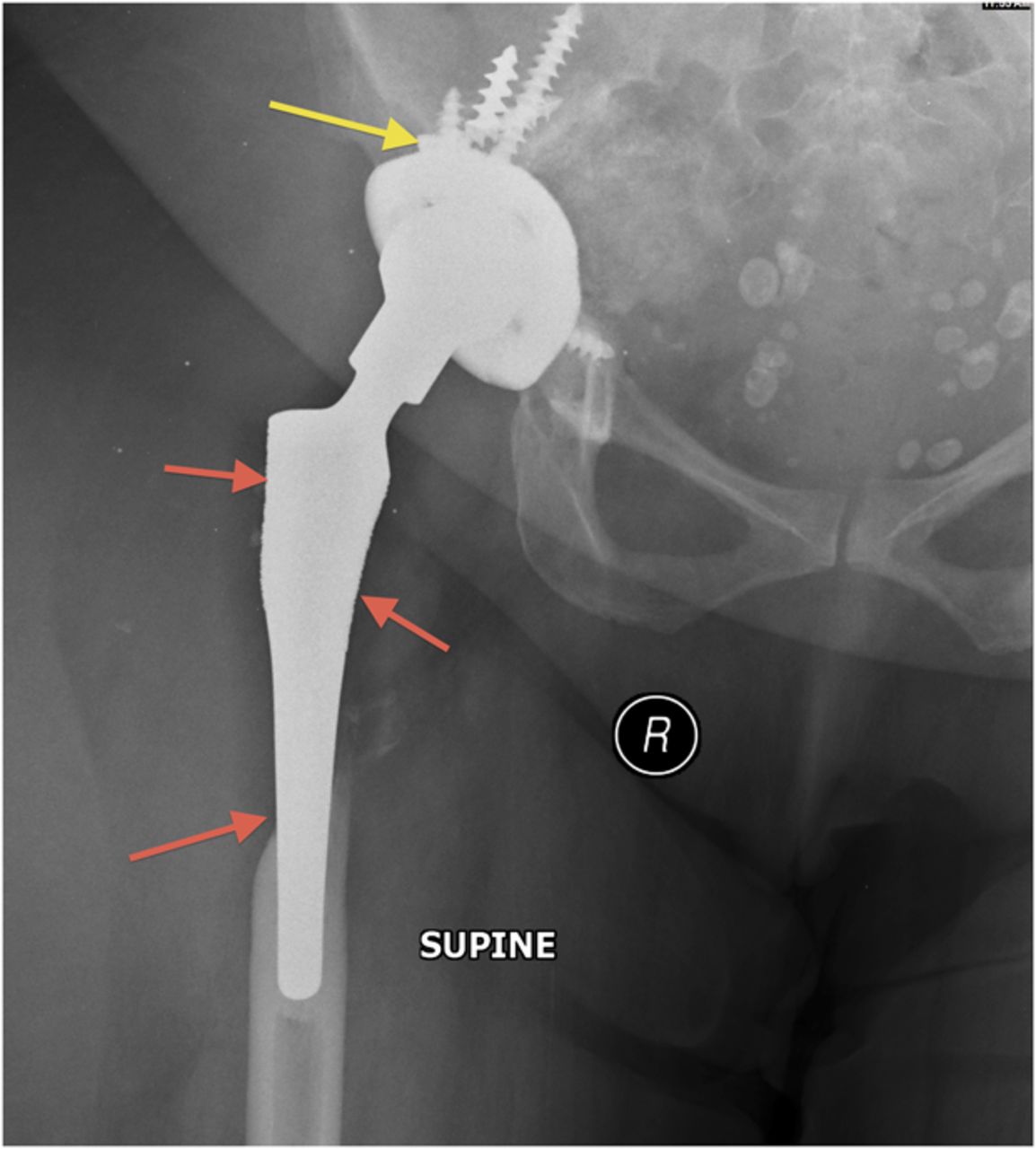
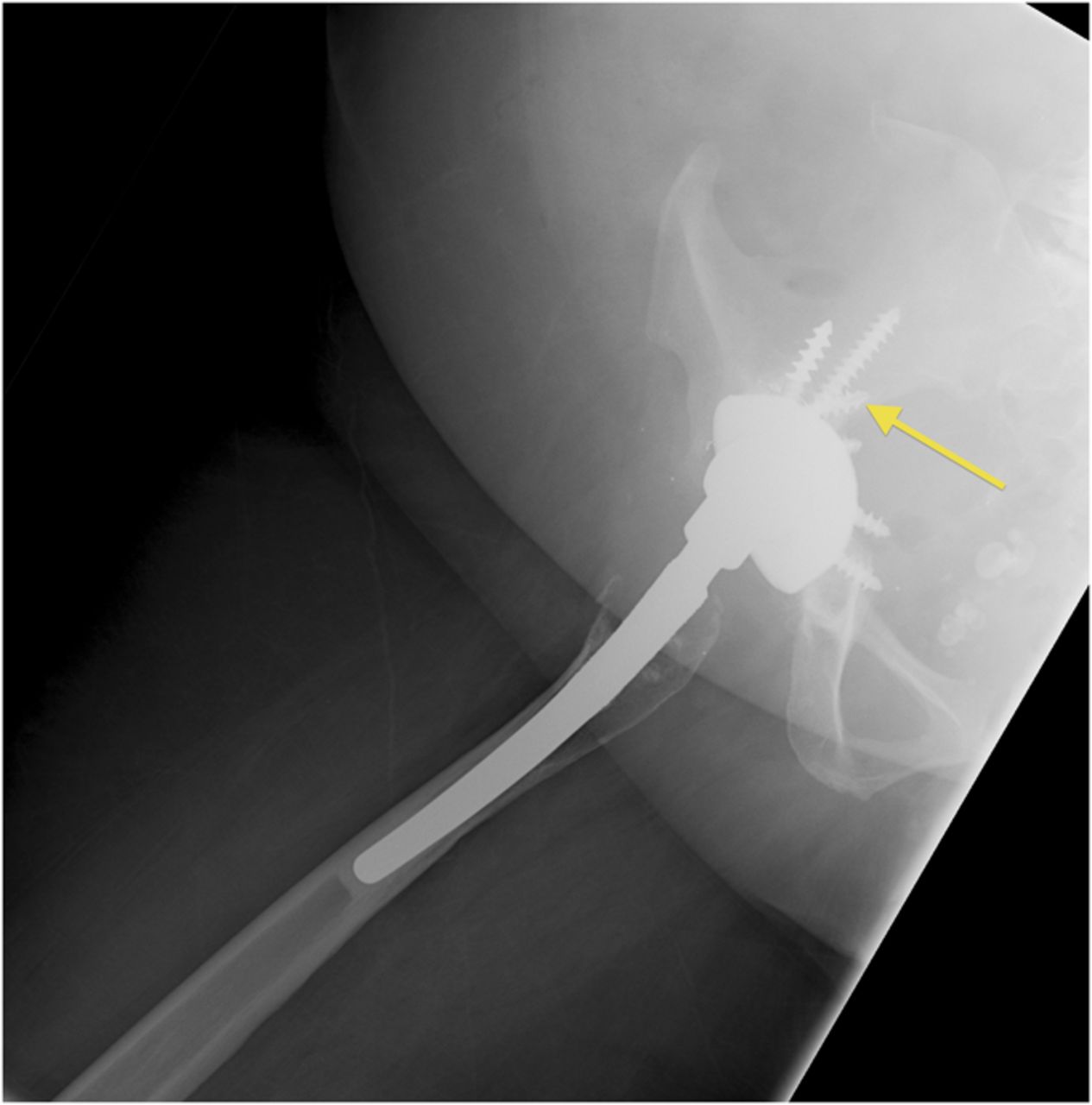
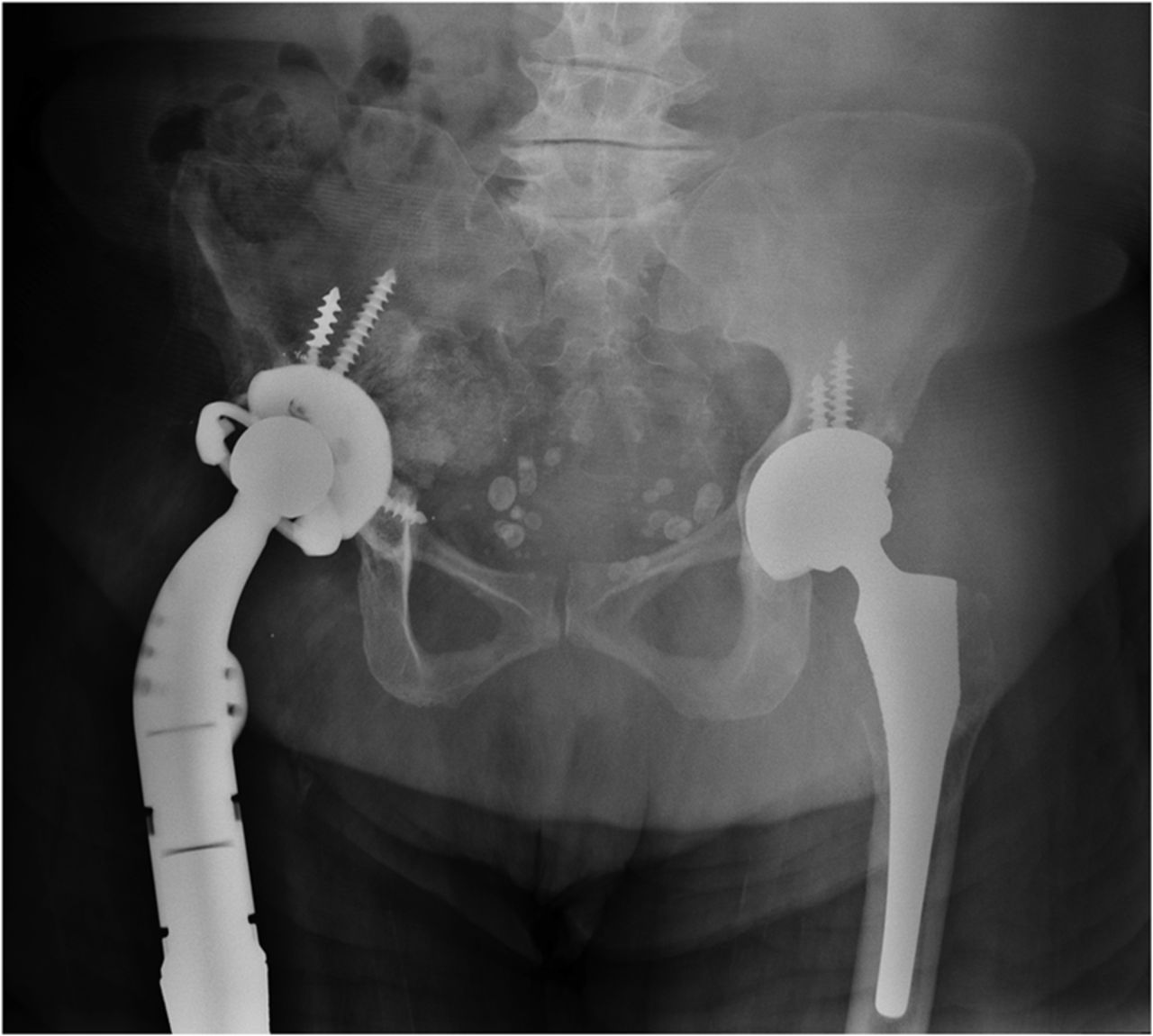
A fifty-three-year-old woman with a history of juvenile rheumatoid arthritis presented to our tertiary care center for a regularly scheduled follow-up of a right hip arthroplasty. She reported acute onset of pain and progressive swelling about the right hip and thigh, which she believed began after hitting a bump in the road while riding in a car three months prior to presentation. Primary right total hip arthroplasty had been performed in 1985. She subsequently underwent a successful two-stage revision hip arthroplasty for sepsis in the mid-1990s, in addition to subsequent structural pelvic bone-grafting for osteolysis in the early 2000s, followed later by polyethylene exchange and pelvic bone-grafting in 2009 (Fig. 1). On examination, the patient had no focal neurologic deficits but did have decreased right dorsalis pedis and posterior tibial pulses as compared with the contralateral extremity. There was a large nonpulsatile compressible mass on the posterolateral aspect of the hip (Fig. 2). Radiographs demonstrated severe implant-threatening bone loss around the femoral component, with substantial interval worsening from previous examinations (Figs. 3-A and 3-B).
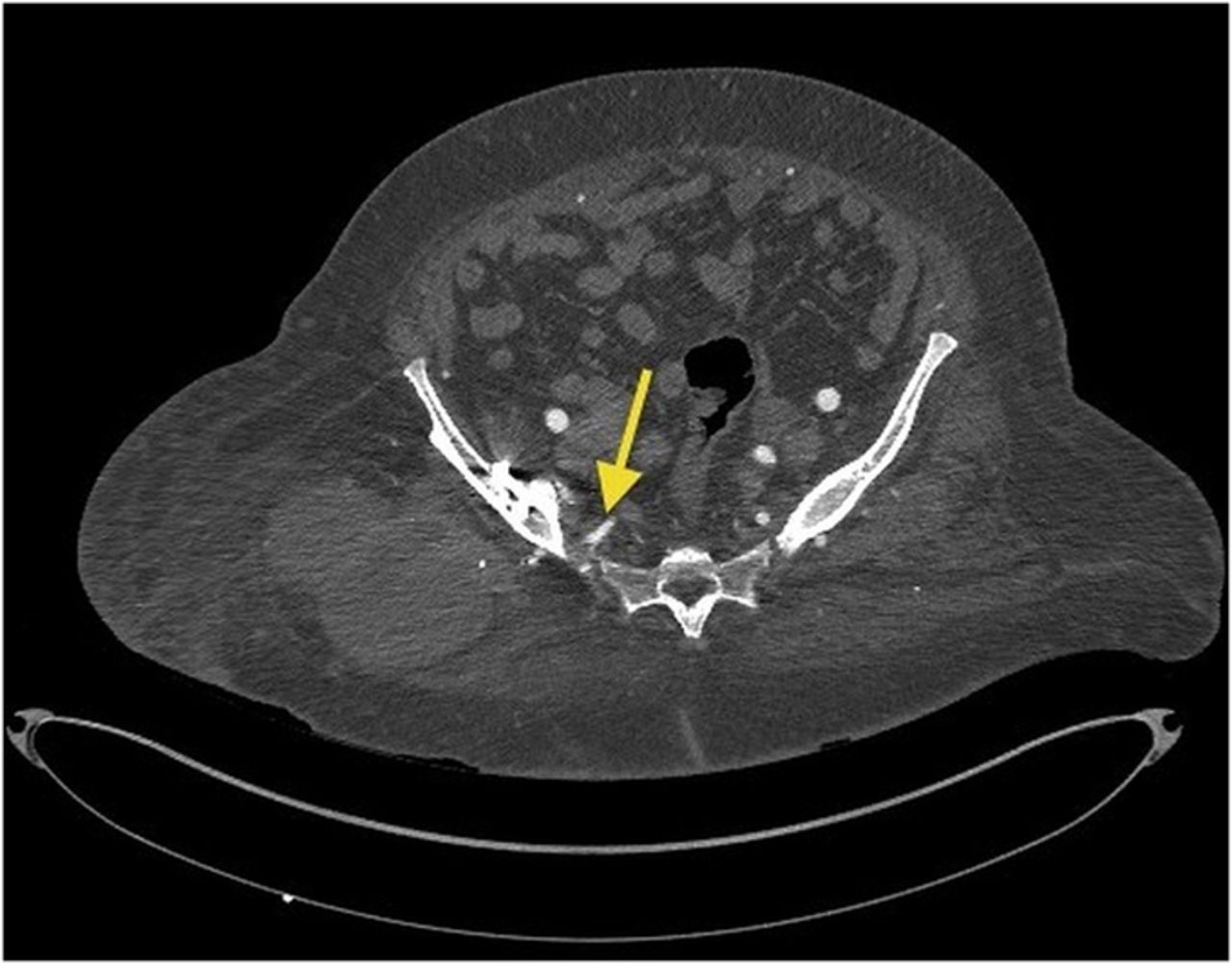
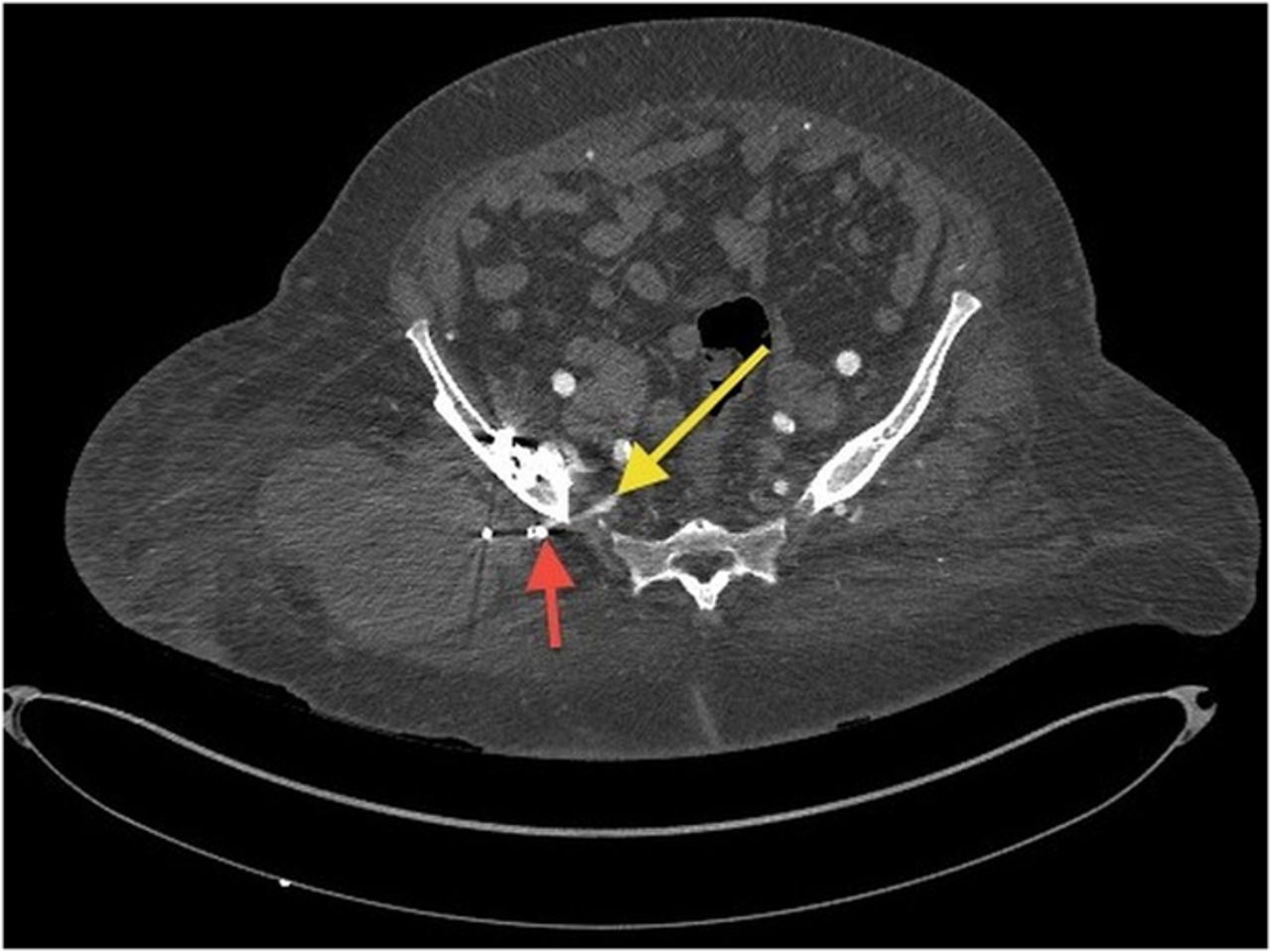
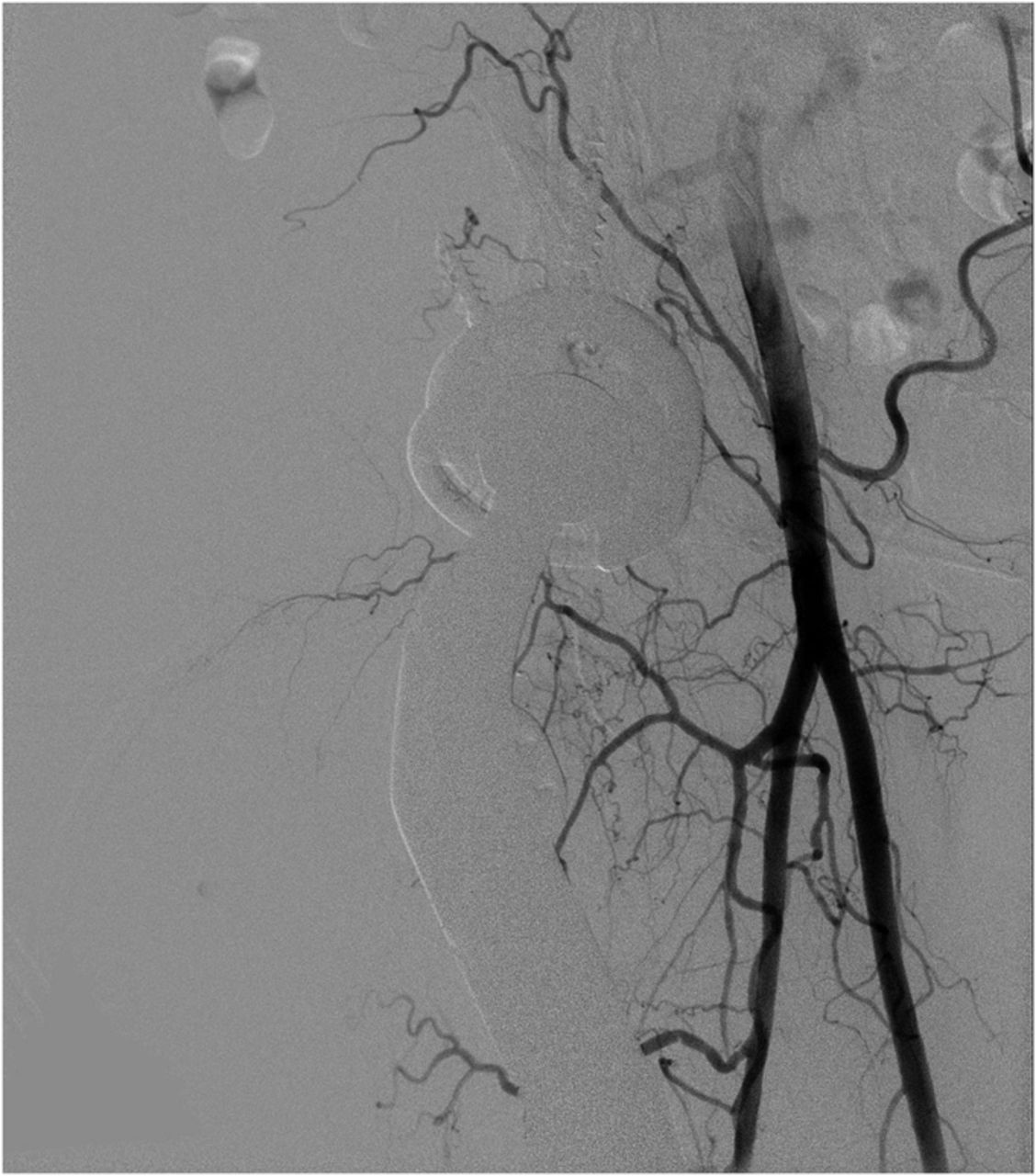
Because of the patient’s asymmetric pulses, a vascular surgery consultation was obtained, and a computerized tomography (CT) angiogram was performed. The study failed to identify any active source of bleeding or arterial compression. Although compression of the femoral artery was expected given the diminished distal pulses, this was not evident on the CT angiogram. It is possible that either intermittent compression or compression undetectable by CT angiogram may have caused the clinically perceived diminished pulses. A free-floating screw was identified near the sciatic notch, contiguous with the superior gluteal artery. Adjacent to this screw, there was a large fluid density (measuring 13 × 19 × 26 cm) surrounding the right hip (Figs. 4-A and 4-B). The original hematoma source, presumably the superior gluteal artery, more than likely had tamponaded by the time of imaging. We proceeded with the revision right total hip arthroplasty with use of a proximal femoral replacement and constrained cemented liner with the retained acetabular shell (Zimmer, Warsaw, Indiana) (Fig. 5-A). While other revision options exist, it was the senior author’s impression that this provided a reasonably stable, durable construct. After the incision had been made, a large hematoma was encountered and evacuated, but no active source of bleeding was identified. In continuity with the hematoma, there was localized necrosis of surrounding soft tissues, including skin, fat, fascia, and muscle, in addition to extensive proximal femoral bone loss, likely secondary to stress shielding compounded by pressure necrosis (Figs. 3-A and 3-B). A free screw was found within the sciatic notch, adjacent to the damaged superior gluteal artery. The screw was removed with minimal effort and without inciting additional bleeding (Fig. 5-B). A postoperative repeat angiogram of the right hemipelvis and lower extremity failed to identify any source of ongoing bleeding (Fig. 6). The patient was returned to the operating room two weeks later for a planned complex wound closure with local tissue transfer by plastic surgeons. Six months postoperatively, she was pain-free and walking with a Trendelenburg gait without an assistive device. Based upon the physical examination, there had been no recollection of fluid.
Proceed to Discussion >>Reference: Alvi HM, Mednick RE, Manning DW. Tissue necrosis resulting from vascular injury due to failed hardware in revision total hip arthroplasty: a case report. JBJS Case Connector. 2013 Oct 09;3(4):e99.
Although the incidence of vascular injury associated with total hip arthroplasty is only 0.25%, the results can be devastating. The majority of injuries can be prevented by diligent and meticulous surgical technique. Specifically, with the placement of periacetabular retractors, injury to surrounding vessels can be minimized with the use of blunt retractors and through cautious placement with respect to surrounding vascular structures. With regard to acetabular screw placement, heeding the Wasielewski four-quadrant system (avoiding the anterior inferior and anterior superior quadrants) results in decreased risk of vascular injury. Yet, even with meticulous technique, the risk for vascular injury cannot be completely eliminated. Revision total hip arthroplasty, an independent risk factor for vascular injury, can leave the surgeon with limited options for acetabular fixation. With decreased posterior bone stock, the surgeon may be forced to gain fixation through the anterior two quadrants, placing the external iliac and femoral vessels at risk. Following both primary and revision total hip arthroplasty, most vascular injuries present early (within twenty-four to seventy-two hours), with either ischemic or hemorrhagic clinical pictures. When vascular injuries have a delayed presentation, they typically manifest as pseudoaneurysms of the femoral or external iliac artery, which classically present as pulsatile groin masses. To our knowledge, this is the first reported case of late vascular injury in total hip arthroplasty presenting as a large nonpulsatile mass with asymmetric pulses, resulting from migrated hardware that caused injury to the superior gluteal artery. The presence of pressure necrosis and extensive bone loss necessitating proximal femoral replacement was also unique. Osteolysis, implant failure, and hardware migration can lead to vascular injury around the hip. Late vascular complications should be considered as a potential etiology for both pulsatile and nonpulsatile soft-tissue masses, especially in patients with findings consistent with claudication or vascular compromise (e.g., asymmetric pulses). Having a high index of suspicion for vascular injury in similar cases may allow for earlier diagnosis and targeted treatment, thereby minimizing potential morbidity and mortality. We recommend prompt vascular consultation and advanced imaging studies, such as CT angiography, for any patient whose clinical picture is concerning for late vascular complication after total hip arthroplasty.
Reference: Alvi HM, Mednick RE, Manning DW. Tissue necrosis resulting from vascular injury due to failed hardware in revision total hip arthroplasty: a case report. JBJS Case Connector. 2013 Oct 09;3(4):e99.
Polyethylene particle disease
Lymphoma of bone
Vascular injury
Malignant fibrous histiocytoma
Metal particle disease

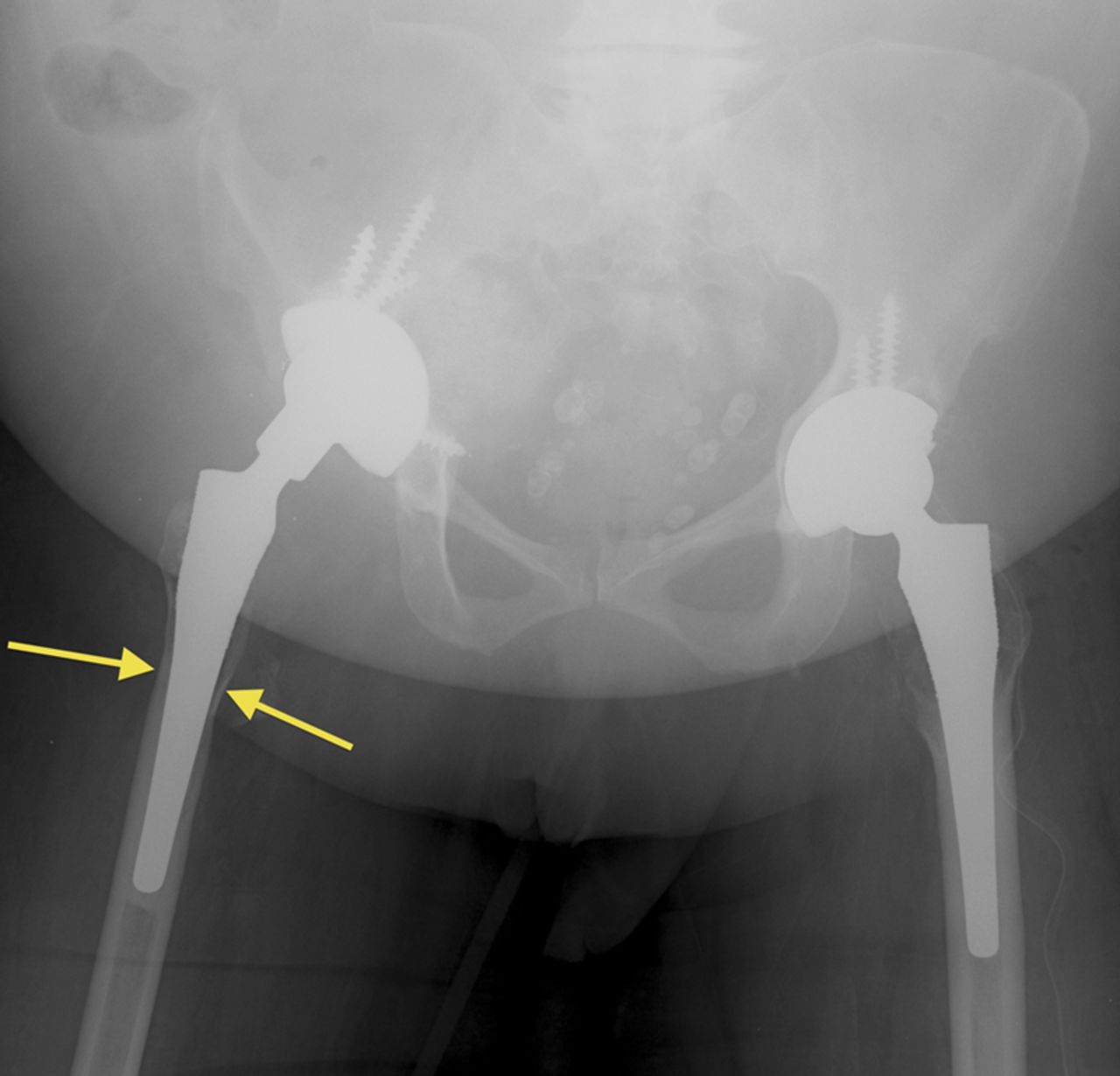
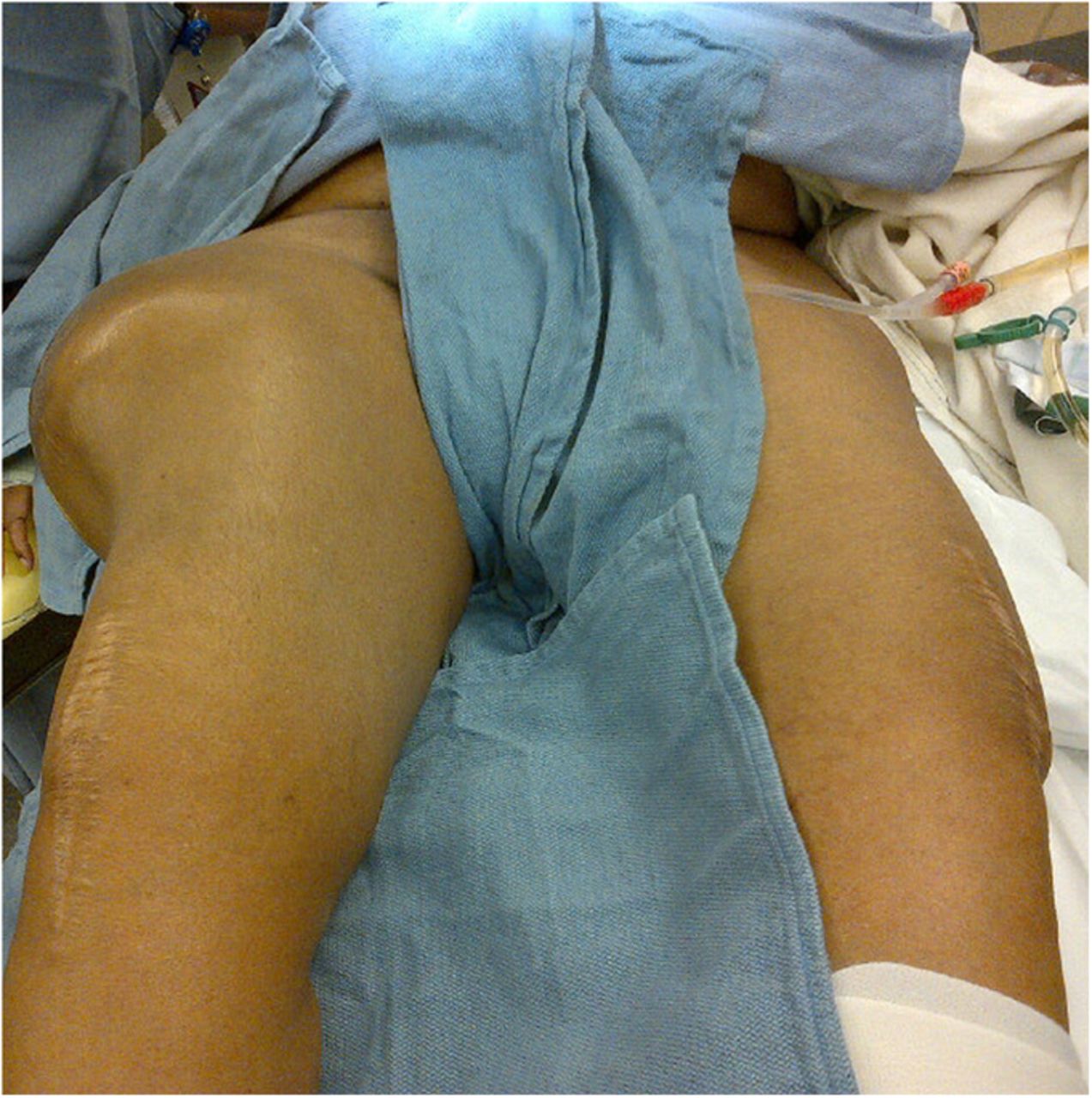
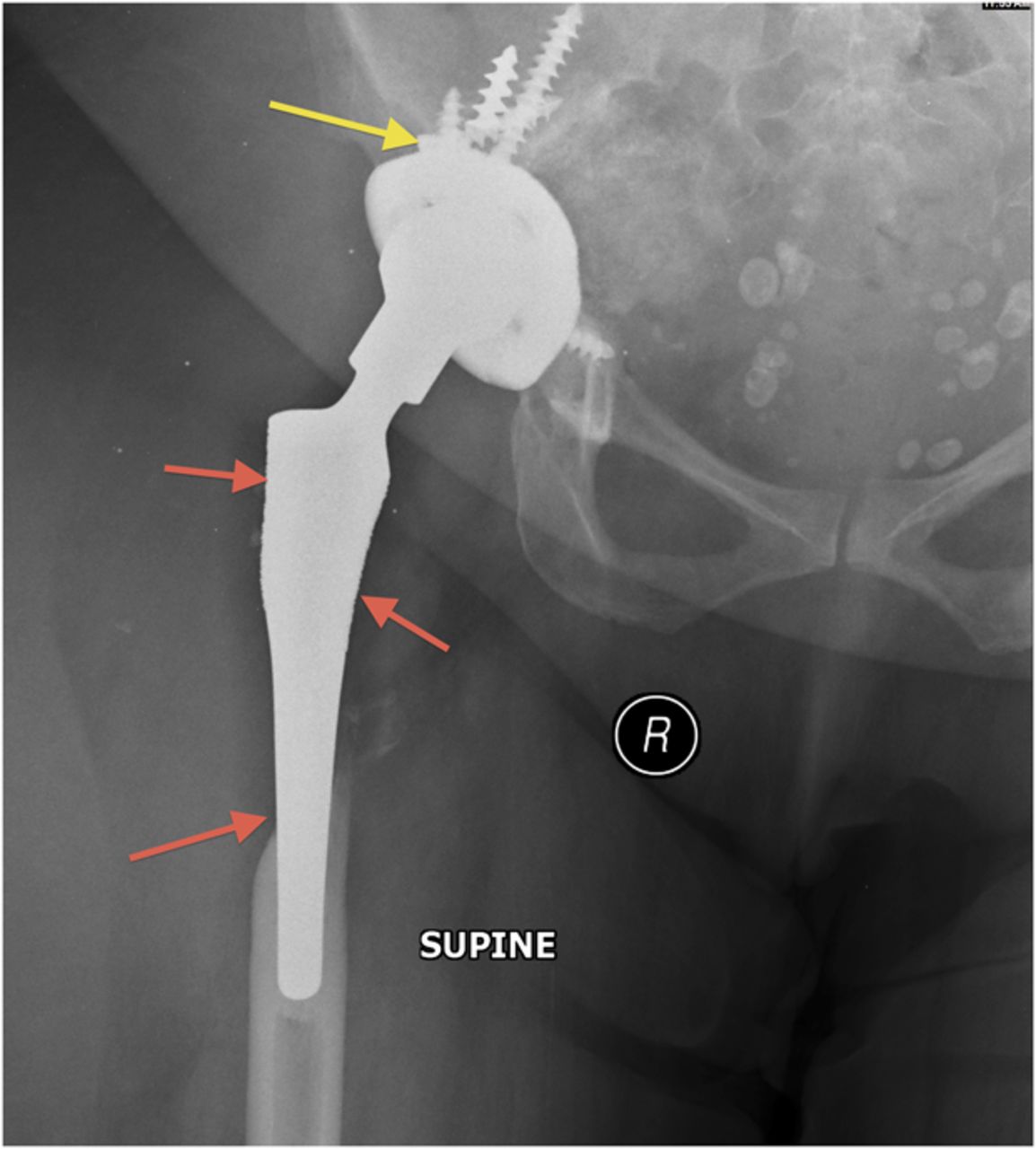
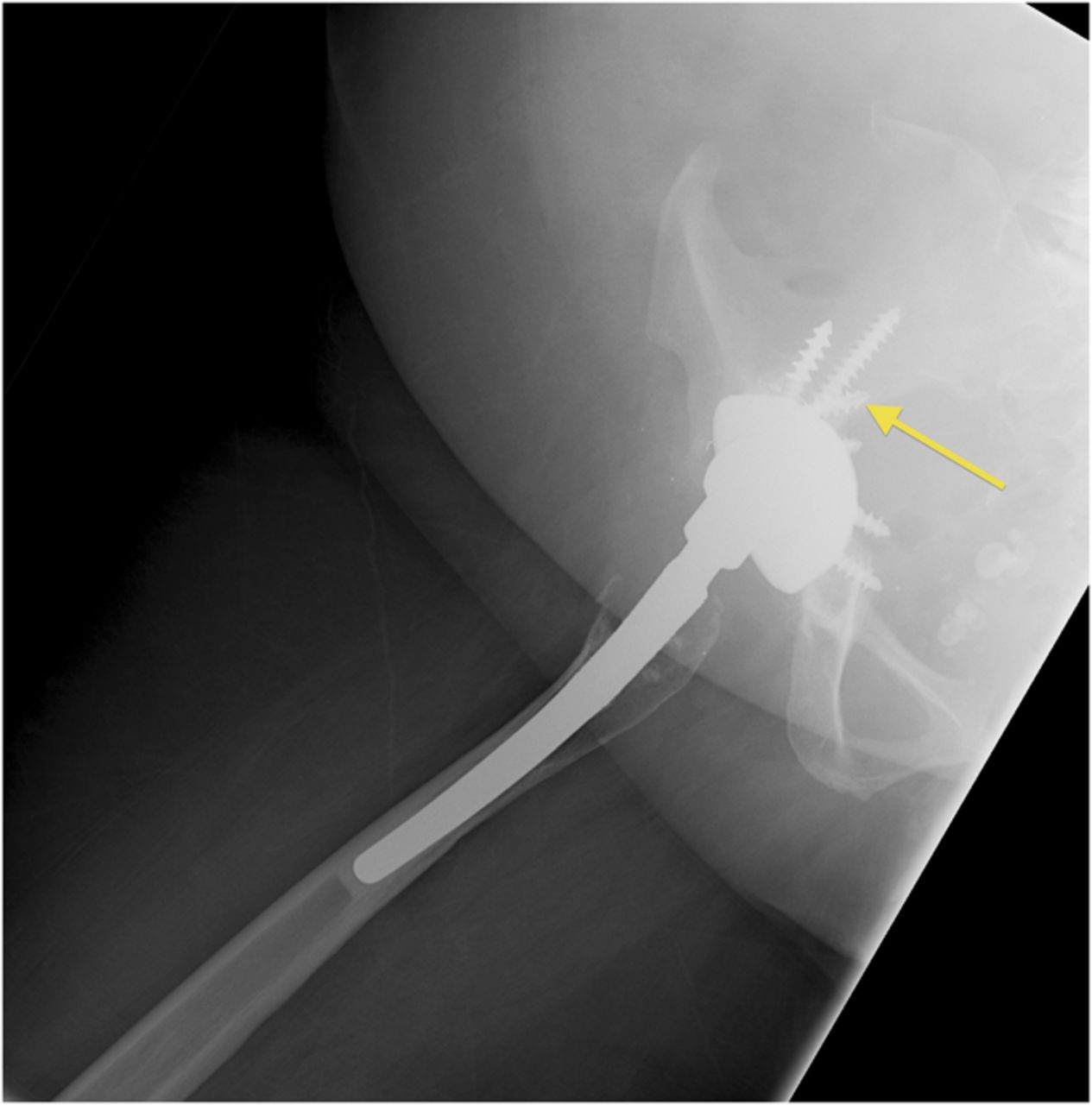
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B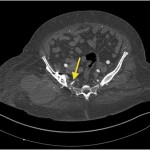 Fig. 4-A
Fig. 4-A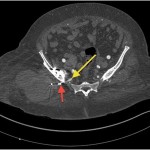 Fig. 4-B
Fig. 4-B Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B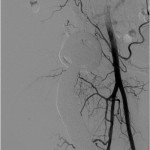 Fig. 6
Fig. 6