A Forty-four-Year-Old Man with Right Shoulder Pain
May 21, 2014
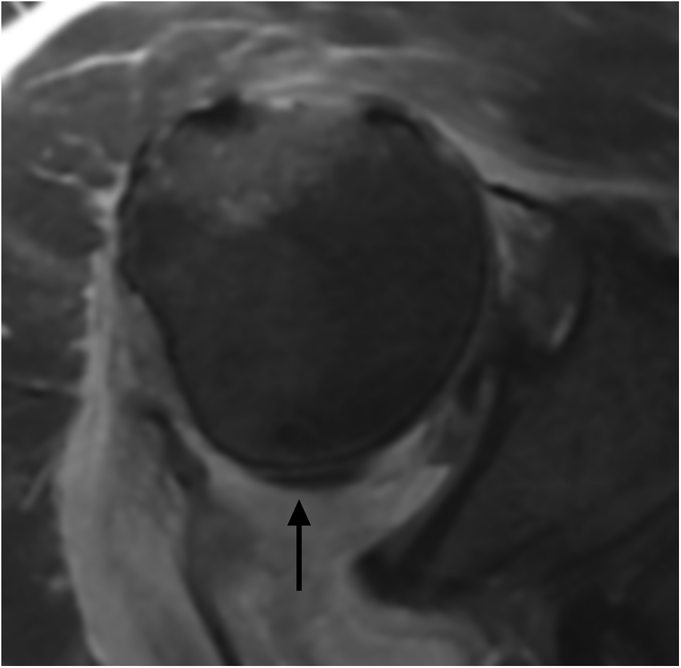
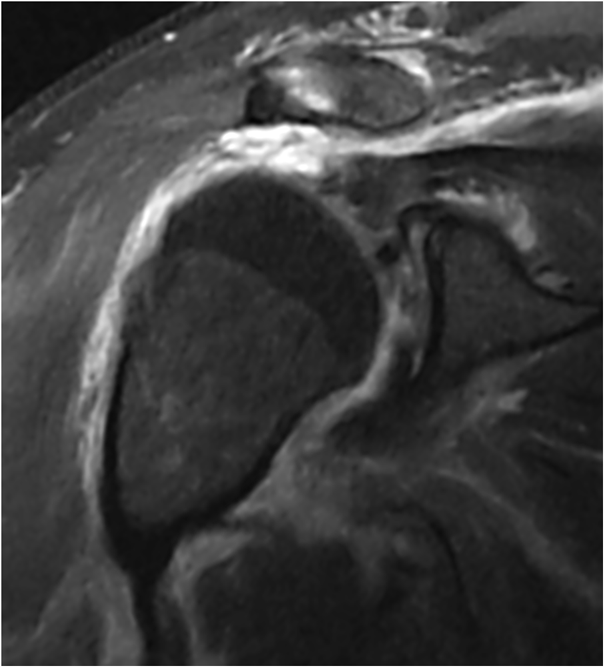
A forty-four-year-old man presented to the Emergency Department following a high-speed motorcycle collision. Upon arrival, the patient’s symptoms included right shoulder pain and decreased range of motion. On physical examination, the humeral head was displaced anteriorly, resulting in loss of the normal contour of the shoulder. The entire right upper extremity was swollen. Sensation was intact throughout the axillary, radial, median, and ulnar distributions, and a 2+ radial pulse was noted at the wrist. Active and passive shoulder range of motion was limited, and additional attempts at assessing shoulder range of motion were not tolerated because of severe pain. An initial radiograph (Fig. 1) of the right shoulder revealed an anterior glenohumeral dislocation with osseous fragments in the glenohumeral joint space. The humeral head was displaced medial and inferior to the coracoid process. Under moderate sedation, attempts to reduce the right shoulder dislocation were performed without success. Computed tomography (CT) of the shoulder (Figs. 2-A and 2-B) obtained after the attempted reduction revealed a persistent anterior dislocation with intra-articular fracture fragments and avulsion of the greater tuberosity.
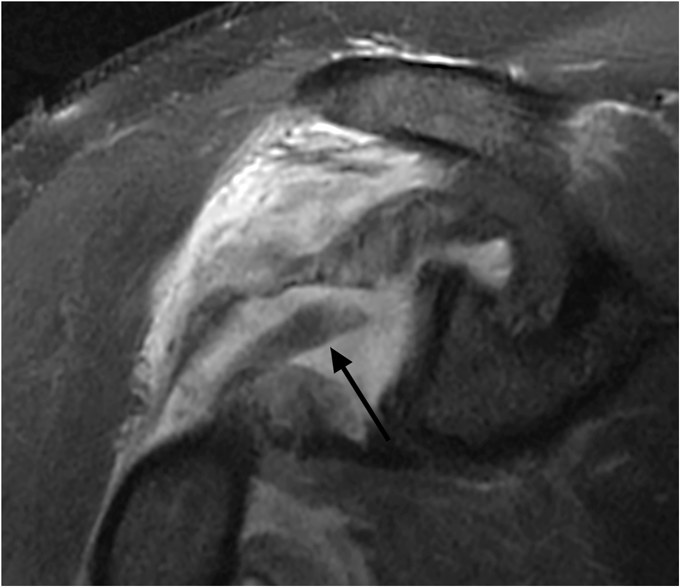
Subsequent magnetic resonance imaging (MRI) (Figs. 3-A through 3-D) showed massive rotator cuff tearing with complete tears of the supraspinatus, infraspinatus, and teres minor tendons. Their myotendinous junctions were retracted to the level of the glenohumeral joint. The subscapularis appeared to be attenuated. The long head of the biceps (LHB) tendon was laterally dislocated and entrapped posterior to the humeral head. Given the severe nature of the injury, a decision was made to proceed with an open approach to the glenohumeral joint to assess the capsular damage and repair the rotator cuff. A deltopectoral incision was used that coursed approximately 2 cm lateral to the coracoid. It was modified in a “bra-strap” fashion over the acromion to allow for an approach through both the deltopectoral interval and the interval between the anterior and middle deltoid heads. There was a substantial amount of hemorrhage and swelling. Through the deltopectoral interval, the subscapularis tendon was found to be stretched but attached to the lesser tuberosity. The undersurface of the subscapularis tendon was palpated through a traumatic window in the rotator interval and no additional injury was noted. The axillary nerve was palpated and found to be intact. The biceps tendon was dislocated laterally and resided posterior to the humeral head. In order to gain better access to the posterior rotator cuff and its footprint, the lateral skin flap was elevated, and a split was made in the raphe between the anterior and middle deltoid heads. The deltoid was elevated slightly off the acromion to increase exposure. The bursa was excised, and the rotator cuff was identified. The supraspinatus tendon was attached to an osseous fragment that had been avulsed from the greater tuberosity just posterior to the bicipital groove. Three #5 FiberWire sutures (Arthrex, Naples, Florida) were sequentially placed in the rotator cuff tendons with use of a Mason-Allen configuration to gain control of the supraspinatus, infraspinatus, and teres minor. The tissue quality was fair. A Cobb elevator and finger dissection were used to mobilize the rotator cuff. The humeral head was inspected and found to be completely uncovered as the rotator cuff had avulsed from it. The footprints were prepared with use of a Cobb elevator to stimulate bleeding for the repair. Two #2 FiberWire sutures were placed through bone tunnels that exited just lateral to the supraspinatus fracture site. The arm was internally rotated, and Super Revo anchors (5.0 mm) (ConMed Linvatec, Largo, Florida) were placed in the teres minor and infraspinatus footprints. These were single-loaded and double-loaded anchors, respectively. Horizontal mattress sutures from each anchor were placed through the teres minor and infraspinatus. The sutures previously placed through the bone tunnels were passed through the supraspinatus tendon just medial to the osseous fragment. The #5 FiberWire sutures, previously placed through the teres minor and infraspinatus, were anchored just lateral to their respective footprints with use of 4.5-mm PopLok anchors (ConMed Linvatec). Upon completion, the rotator cuff moved with the humeral head as a unit. The biceps tenodesis was performed by passing two #2 FiberWire sutures through the tendon and anchoring it in the bicipital groove with an additional 4.5-mm PopLok anchor. The deltoid was repaired back to the acromion through drill-holes with use of #2 FiberWire suture. Postoperatively, the patient used a sling with an abduction pillow. Because of the extensive nature of the injury, the high re-tear rate of such a massive rotator cuff tear, and the patient’s relatively young age, the arm was maintained in the sling with limited movement for six weeks. Following this period, an additional six weeks of passive and active-assisted range of motion were begun under the guidance of a physical therapist, with active motion beginning at three months postsurgery. At five months following surgery, the patient could reach the hand to his mouth and to the top of his head. He could actively forward flex the affected arm fully in the supine position, but had limited forward flexion against gravity to 80° because of reduced strength. Throughout the postoperative course, he had intact sensation in the axillary distribution, and the deltoid muscle fired actively. External rotation strength was graded as 4 of 5. With the arm at his side, the patient had a 10° lag sign. Active external rotation was 40°, and passive external rotation was 50°. The hornblower’s test was negative. The patient declined additional diagnostic procedures to evaluate the integrity of the repair. He denied any pain or sense of shoulder instability and, shortly thereafter at his request, he was discharged from rehabilitation services and he returned to work.
Proceed to Discussion >>Reference: Wortley P, Omar L, Robertson W, Moore D, Cho Sims G, Omar H. Nonreducible shoulder due to acute posterior dislocation of the long head of the biceps tendon: a case report and review of the literature. JBJS Case Connector. 2014 Mar 12;4(1):e26 1-4.
Posterior or lateral LHB tendon dislocation is associated with high-energy trauma to the shoulder and requires disruption of the lateral stabilizing structures of the biceps, which include the anterior supraspinatus tendon, superior glenohumeral ligament, and the coracohumeral ligament. Avulsion fractures of the greater tuberosity and severe rotator cuff injury are commonly associated. The greater tuberosity disruption destabilizes the bicipital groove, enabling the tendon to dislocate. The displaced tendon will obstruct attempts at closed reduction of the anterior glenohumeral dislocation. The displaced tendon can also interfere with reduction of the greater tuberosity by becoming interposed between fracture fragments. A potential alternative mechanism of this injury involving subperiosteal stripping of the supraspinatus and infraspinatus tendons from their osseous insertion sites has also been described. Rare cases of posterior LHB tendon dislocation occurring without an associated greater tuberosity fracture have also previously been reported. The patient described in this case report had a combination of these injuries. The supraspinatus tendon was avulsed with an ossific fragment from the greater tuberosity, while the infraspinatus and teres minor were avulsed from their footprints without fracture. Posterior or lateral LHB tendon dislocation may be suspected clinically by the inability to successfully relocate the shoulder following anterior glenohumeral dislocation or by persistent pain or disability after attempted closed reduction. However, imaging is essential for the diagnosis and for assessing the extent of injury for appropriate surgical planning. In previous case reports, imaging features of conventional radiographs, CT, and MRI associated with posterior LHB tendon dislocation have been described. Radiographic features associated with posterior LHB tendon dislocation include anterior humeral subluxation/dislocation, medial displacement of the humeral head relative to the coracoid process, greater tuberosity fracture fragment, and displacement of the greater tuberosity fracture fragment from the humeral head in excess of 1 cm. In the few case reports that included CT imaging, findings associated with posterior LHB tendon dislocation included anterior subluxation of the humeral head, greater tuberosity fracture, and coracoid process fracture. To our knowledge, MRI findings of posterior LHB tendon dislocation have been described previously in only three case reports. Key findings on MRI included an empty bicipital groove, anterior subluxation/dislocation of the humeral head, greater tuberosity fracture, and rupture of the supraspinatus and infraspinatus tendons. Scrutiny of the lateral soft-tissue stabilizers is critical for diagnosis since the LHB tendon dislocates laterally with respect to the proximal part of the humerus to reside along the posterior margin of the humeral head. The diagnosis of posterior LHB tendon dislocation should be suspected following anterior shoulder dislocation resulting from a high-velocity mechanism with failed attempts at reduction, particularly when an associated displaced greater tuberosity fracture is identified. MRI is the preferred imaging modality for confirmation and provides an accurate assessment of associated injuries for surgical planning since open reduction and biceps tenodesis/tenotomy are necessary for successful treatment.
Reference: Wortley P, Omar L, Robertson W, Moore D, Cho Sims G, Omar H. Nonreducible shoulder due to acute posterior dislocation of the long head of the biceps tendon: a case report and review of the literature. JBJS Case Connector. 2014 Mar 12;4(1):e26 1-4.
Stump of the anterior glenohumeral ligament
Anterior glenoid labrum
Long head of the biceps tendon
Coracoacromial ligament
Subscapularis tendon stump

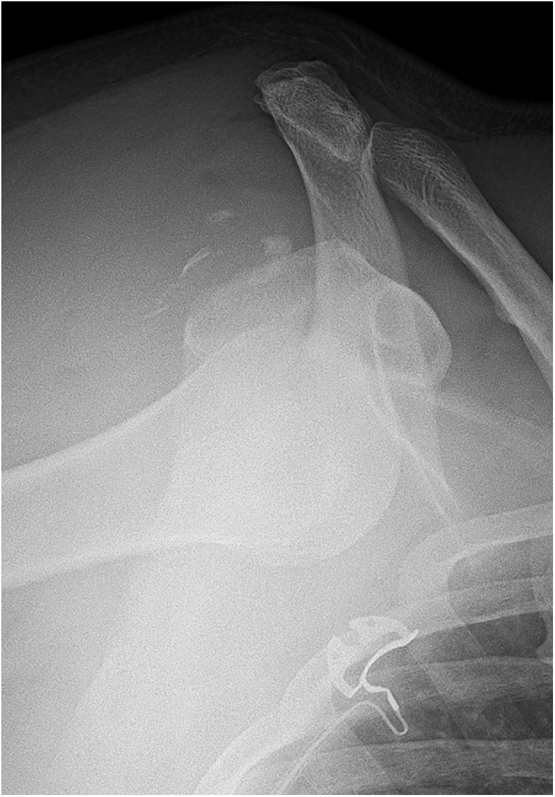
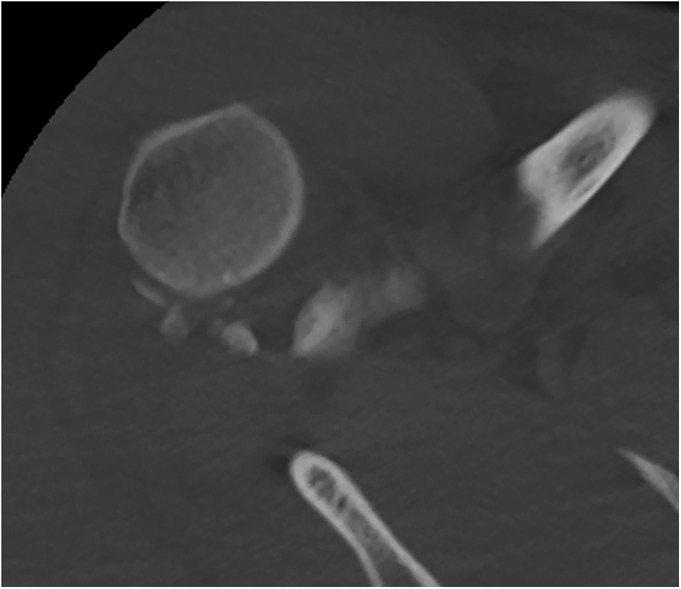
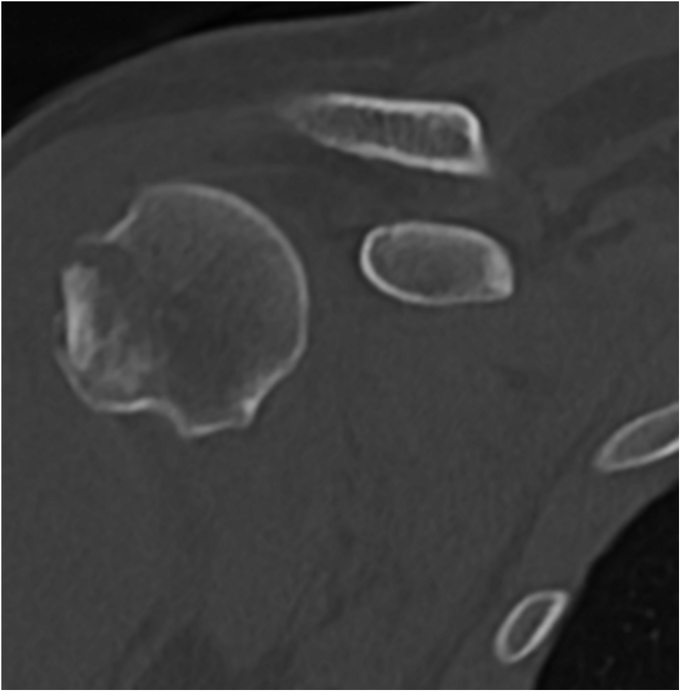
 Fig. 1
Fig. 1 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B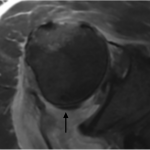 Fig. 3-A
Fig. 3-A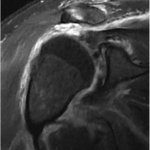 Fig. 3-B
Fig. 3-B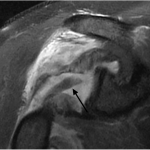 Fig. 3-C
Fig. 3-C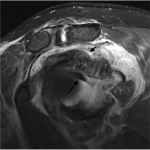 Fig. 3-D
Fig. 3-D