A Nineteen-Year-Old, Right-Hand-Dominant Baseball Player with Right Shoulder Pain
February 19, 2014
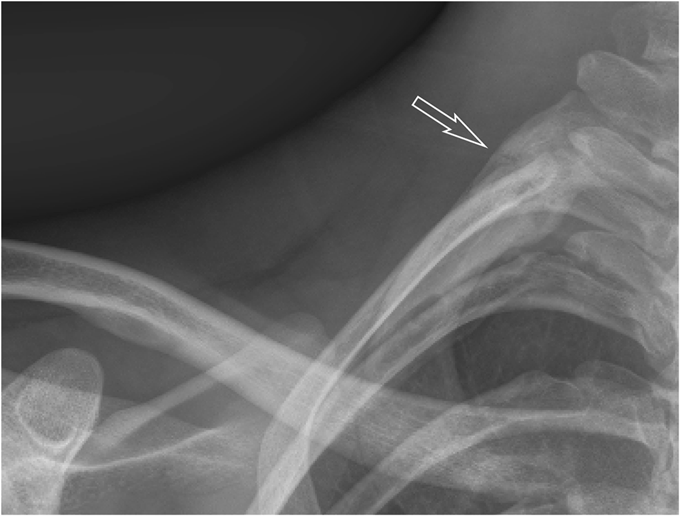
A nineteen-year-old right-hand-dominant male collegiate baseball pitcher presented to the office with the symptom of right shoulder pain. He denied any history of trauma but stated that he had felt a popping sensation in the shoulder while pitching several days prior to presentation, and he had had pain since that time with both pitching and activities of daily living. He denied any change in the pitching mechanics or increase in the number of pitches in the preceding several weeks. He had no prior history of trauma to the spine or thorax. The pain was aggravated by the late-cocking phase of throwing. He also admitted to difficulty with deep inspiration because of the pain at the base of the neck, but had no dyspnea at rest. On examination, he was 6'8" (203.2 cm) tall and weighed 193 lb (87.5 kg), and he had a body mass index of 21.3. He was in no acute respiratory distress. Pain was elicited with deep palpation of the upper trapezius muscle posterosuperiorly, just lateral to C8-T1 at the cervicothoracic junction. Shoulder range of motion was to 180° of forward flexion and abduction bilaterally, and 60° of external rotation in adduction on the right. He did experience pain during both passive and active motion when the arm was brought beyond 90° of abduction, which was aggravated by external rotation from 45° to 90°. Manual muscle testing of the rotator cuff revealed full strength bilaterally. He had no pain with the active-compression test for labral pathology or the posterior impingement sign as described by Meister et al. He had no pain with adduction of the arm across the chest. He had a pain-free arc of motion with forward elevation from 0° to 180°. He had no prominence of the medial scapular border to suggest scapular dyskinesis. The radial pulses were palpable and symmetric bilaterally with the arms at his side, and they did not diminish with full shoulder abduction. He was neurologically intact throughout the upper extremities. Radiographs of the right shoulder, obtained on initial presentation, are shown in Figure 1. After discussion with a radiologist, it was felt that the patient should undergo a computed tomography (CT) scan with angiography to rule out pneumothorax and to evaluate for any vascular compromise. The CT angiogram (CTA) was obtained the following day (Figs. 2-A and 2-B). Three-dimensional reconstructions of the CT scan are shown in Figure 3. Although there was evidence of subclavian artery stenosis, circulation was intact distal to the compression, with contrast noted in the axillary and brachial arteries. No pneumothorax was seen on any of the imaging studies, and the patient was discharged home with instructions to return to the emergency department for any symptoms of peripheral vascular compromise or shortness of breath. He was instructed to refrain from sports activities until he was seen in follow-up. He also underwent consultation with vascular surgery, and no intervention or additional workup was recommended; because he had palpable pulses that did not diminish with full shoulder abduction, the patient did not clinically demonstrate signs of arterial thoracic outlet syndrome.
At nine weeks postinjury, the patient returned to clinic and underwent repeat imaging of the right shoulder. Osseous bridging and callus formation were evident (Fig. 4); on physical examination, the patient had no tenderness at the fracture site or with shoulder range of motion. He remained neurovascularly intact with complete abduction of the shoulder, and he was released to play baseball at this time.
Proceed to Discussion >>Reference: Chimenti PC, Elfar JC, Giordano BD. Dominant-Sided First-Rib Stress Fracture in a Collegiate Baseball Pitcher: A Case Report. JBJS Case Connector, 2013 Oct 23;3(4):e108.
In 1966, Curran and Kelly reported the first case of first-rib fracture in a baseball pitcher, but this case involved the patient’s nondominant arm. Previously published studies have hypothesized differing mechanisms as a cause for dominant and nondominant-sided injuries. With our patient, our hypothesis is that the first rib underwent a stress fracture from repeated microtrauma from the opposing shear forces of the serratus anterior and scalene muscles. Mintz et al. reported the case of a weightlifter with a stress fracture of the nondominant first rib; they examined the recruitment of the serratus anterior and scalene muscles with use of T2-weighted magnetic resonance imaging (MRI). The authors argued that contracture of the scalene muscles alone, while sufficient to explain a nondominant-sided injury in pitchers, would require the addition of eccentric contraction from the serratus anterior muscle in order to produce dominant-sided injury. This hypothesis is supported by electromyography findings showing increased activity in the serratus anterior during the late cocking and deceleration phases of the throwing motion. Many other cases of first-rib stress fractures have subsequently been reported, including a seventeen-year-old athlete who sustained a dominant-sided injury from pitching; he returned to play after only nine months of rest to allow for osseous union. Another case report describes a pitcher who developed an asymptomatic nonunion at four months, returned to sport at six months, and remained asymptomatic at the fourteen-month follow-up. The first rib is broad, flat, and C-shaped in structure, with two shallow grooves on the cephalad surface for the subclavian artery and vein. Although relatively protected by surrounding muscle, the first rib remains vulnerable to stress fractures because of the shear forces it experiences through the opposing actions of the serratus anterior (caudad force) and scalene muscles (cephalad force). The most common anatomical location for fatigue fractures of the first rib is through the shallow groove for the subclavian artery at the junction of the anterior one-third and posterior two-thirds of the rib, just posterior to the scalene tubercle. Our case illustrates that not all fatigue fractures occur through the subclavian groove; the fracture in our patient occurred through the posterior one-third of the rib, near the insertion of the middle scalene muscle (Fig. 5). As seen in Figure 3, the anterior aspect of the rib was displaced in a cephalad direction because of the action of the anterior scalene muscle, while the posterior aspect of the fracture was inferiorly displaced because of the pull of the serratus anterior muscle. The fulcrum for the pivoting of the fracture may have been the insertion of the middle scalene muscle, which resulted in narrowing of the costoclavicular interval and stenosis of the subclavian artery (Figs. 2-B and 3). Our patient underwent an urgent CT scan with angiography because of shortness of breath and pain with deep inspiration, and because radiographs were not able to rule out the presence of a pneumothorax with a high degree of certainty. Prior studies have examined the role of angiography in this type of injury. In a review of 730 cases of traumatic first-rib fractures, Gupta et al. reported an overall incidence of vascular injury of 3% for isolated first-rib fractures and 24% if multiple ribs were involved. The authors presented specific indications for angiography, including mediastinal widening on chest radiographs, absent or diminished pulses in the upper extremities, brachial plexus injuries, expanding hematoma, or substantially displaced (>4 mm) posterior rib fractures. While our patient did not present with any clinical signs of arterial thoracic outlet syndrome, the CTA did show evidence of vascular compromise focally at the costoclavicular interval. Vascular surgery literature indicates that any clinical sign of pain, claudication, pallor, or poikilothermia in the arm or hand in the presence of an osseous abnormality mandates arterial imaging for further diagnosis. Up to 80% of patients with symptomatic stenosis and focal osseous lesions may have arterial pathology that requires operative management. This case highlights the importance of maintaining a high index of suspicion for possible vascular injury with first-rib stress fractures, even in the absence of clinically apparent signs. While some authors have suggested that first-rib stress fractures may be predisposed to delayed or nonunion and have allowed prolonged time (nine months) for healing to occur before allowing return to play, we suggest that return to sport may be considered once clinical and radiographic signs of union have been observed, which may be earlier than previously reported.
Reference: Chimenti PC, Elfar JC, Giordano BD. Dominant-Sided First-Rib Stress Fracture in a Collegiate Baseball Pitcher: A Case Report. JBJS Case Connector, 2013 Oct 23;3(4):e108.
Osteoblastoma of the first rib
Stress fracture of the first rib
Osteoid osteoma of the first rib
Acute fracture of the first rib

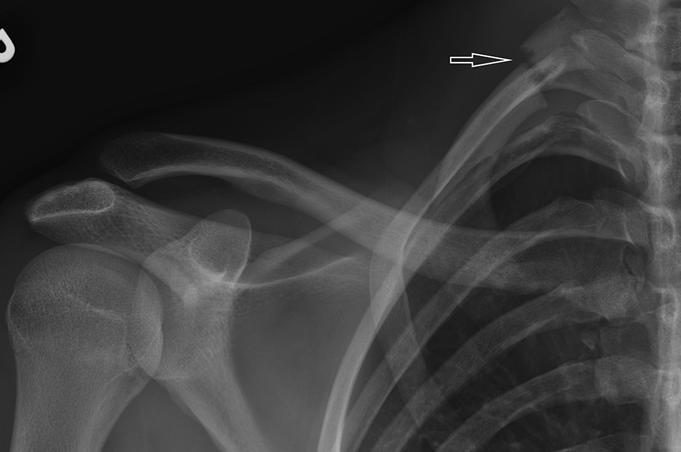


 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 2
Fig. 2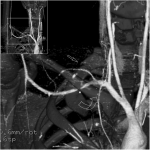 Fig. 3
Fig. 3 Fig. 4
Fig. 4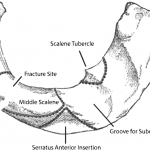 Fig. 5
Fig. 5