A Thirty-one-Year-Old Woman with Left Gluteal Pain
March 5, 2014
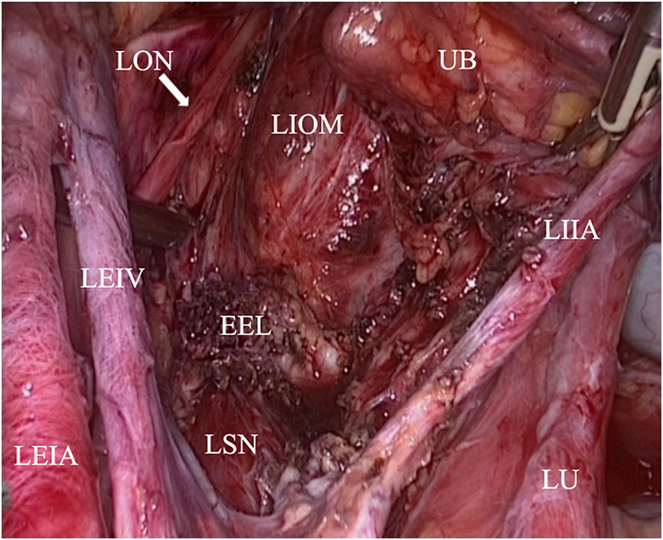
A thirty-one-year-old woman presented with the symptom of cyclical left gluteal pain for more than two years. The pain had become increasingly intense with a longer duration, and it radiated to the dorsal aspect of the left thigh as well as to the lateral aspect of the lower leg. Because of atrophy of the left calf, the patient was evaluated by orthopaedists, and common diagnoses were excluded. She started experimental oral gestrinone therapy (2.5 mg twice daily for eight months). During that treatment period, open neurolysis of the left common peroneal nerve was performed. Recurrent pain and paresthesia of the left leg persisted, and the patient developed difficulty walking and had a steppage gait as well as a foot drop. She was referred to our department after the local hospital identified a lesion that involved the left sciatic nerve. On examination, the patient had a steppage gait; atrophy of the hamstring muscle and calf; and decreased strength in the left hamstring (3/5), tibialis anterior (0/5), tibialis posterior (4/5), gastrocnemius (0/5), soleus (0/5), and flexor hallucis longus (0/5) muscles. Tenderness was present over the greater sciatic notch, as well as the obturator foramen, but no mass could be detected. Sensation was decreased over the lateral aspect of the calf and the medial dorsum of the foot. Bimanual pelvic exploration revealed a painful vaginal nodule that measured 2.5 cm × 2 cm. A digital rectal examination revealed tenderness superior to the left ischial spine, but no lesion was palpated. With compression of the left buttock, the pain became extremely intense and intolerable. Radiographs and magnetic resonance imaging (MRI) of the lumbar spine were normal. MRI of the pelvis demonstrated lesions located posterior to the cervix and superolateral to the left ovary. MRI of the left thigh showed a soft-tissue mass involving the left sciatic nerve at the sciatic notch level, and thickening of the distal course of the sciatic nerve (Figs. 1-A and 1-B). Atrophy of the left gluteal muscle as well as edema of the biceps and semitendinosus muscles was also identified. Electromyography demonstrated left tibial and peroneal nerve injury. Evidence of denervation in the left gluteus maximus, biceps femoris, tibialis anterior, and gastrocnemius muscles was also revealed, which was considered to be an injury of the L4-S1 sacral plexus. A combination of laparoscopic and transgluteal approaches to achieve complete removal of the intrapelvic and extrapelvic lesions and to achieve full neurolysis of the sciatic nerve was proposed by a team of gynecologists, orthopaedists, and microsurgical experts. The patient initially was placed in the lithotomy position, and laparoscopic exploration was performed by the gynecologists. Nodules involving the posterior fornix (infiltrating the full-thickness of the vaginal wall) and the right uterosacral ligament were completely resected. The left ureter, the external and internal iliac vessels, the obturator nerve, and the sciatic nerve were carefully dissected. An area of tissue was found near the greater sciatic foramen, extending distally and combining with the extrapelvic focus. Resection of the endopelvic part of the lesion was performed. The patient was then placed in the prone position for orthopaedic and microscopic surgery. Suspicious macroscopic pathologic hard tissue around the nerve was resected. Incision of the epineurium of the sciatic nerve and removal of the endoneurial fibrosis were performed under the microscope. Finally, neurolysis was achieved (Figs. 2-A and 2-B) and a pathological examination was performed.
Laparoscopic exploration revealed an endopelvic endometriotic lesion involving the sciatic nerve (Fig. 3), which was confirmed by pathological examination (Fig. 4). The patient received treatment with gonadotropin-releasing hormone agonists for six months postoperatively. Prominent pain relief of the left buttock and leg was achieved by the tenth postsurgical day. Inability of dorsiflexion and eversion of the left foot persisted. Muscle strength was evaluated: tibialis anterior muscle, 0/5; extensor digitorum muscle, 0/5; musculus peroneus longus, 0/5; musculus peroneus brevis, 0/5; musculus tibialis posterior, 4/5; and plantar flexion muscle, 4/5. Neurological examination showed loss of sensation of the lateral dorsum of the left foot. At the three-month follow-up, the left gluteal pain had resolved completely. Muscle strength of the left leg was substantially improved, but the patient still had disabling dorsiflexion and eversion of the left ankle joint with a steppage gait. Patient satisfaction about the outcome of surgery was scored from 0 to 10 on a quality of life questionnaire (a score of 0 to 4 is considered “dissatisfied,” 5 to 8 is “satisfied,” and 9 to 10 is “very satisfied”). The patient reported a score of 7 at the three-month follow-up, without sequelae on bowel, bladder, and sexual functions. Additional follow-up at nine months after surgery showed persistent relief from pain, but no additional improvement of the neuromuscular deficit.
Proceed to Discussion >>Reference: Jiang H, Liang Y, Li L, Gu L, Yao S. Cyclic sciatica due to endometriosis of the sciatic nerve: neurolysis with combined laparoscopic and transgluteal approaches: a case report. JBJS Case Connector. 2014 Jan 22;4(1):e11.
Endometriosis, defined as the presence of functioning endometrial tissue in an abnormal anatomical location, affects 10% (range, 4% to 17%) of women of childbearing age. Extrapelvic endometriosis with particular manifestations accounts for a small percentage, including those involving the lung, brain, and bowel. Moreover, cases of isolated deep infiltrating endometriosis and extrapelvic endometriosis (especially of the sciatic nerve) are rare. Even though endopelvic endometriosis was confirmed postoperatively in our patient, the typical symptoms (dysmenorrhea, chronic pelvic pain, dyspareunia) of pelvic endometriosis had not been present. Only the cyclic characteristic of pain had provided a clinical suspicion of endometriosis. Symptomatic patients are often referred to neurologists or orthopaedists. Radiographs and computed tomography of the lumbar spine are normal in most cases, which helps to exclude neurologic and osseous abnormalities. Pelvic and hip MRI may provide direct evidence of the location, shape, and size of the sciatic lesion, as well as information about its relationship with the peripheral tissues and local circulation (enhanced with the addition of contrast-enhanced magnetic resonance angiography). The cystic appearance of the mass presents variable signal intensities on T1 and T2-weighted images because of the variable quantity and age of the hemorrhagic products, and because of the proportion of endometrial cells and stromata within the lesion. Other indirect findings include atrophy and denervation of distant target muscles of the sciatic nerve. In our patient, pathological findings included endometriosis of the bilateral uterosacral ligaments and nodules of the posterior vaginal fornix, piriformis muscle, superior gluteal nerve, sciatic nerve (Fig. 4-A), and obturator lymph nodes (Fig. 4-B). Lymph node involvement by endometriosis is considered to be uncommon, and the status of lymph nodes in endometriosis remains obscure because lymph node dissection is usually not performed for benign disease. In the surgical findings in our patient, the sciatic lesion was isolated from the pelvic lesions. We believe that endometriosis of the sciatic nerve was not the result of retrograde menstruation or coelomic metaplasia. The presence of endometriosis in the lymph nodes might have been a result of lymphatic dissemination originating from the principal focus located in the posterior vaginal fornix and/or the sciatic nerve. Interestingly, one study reported more frequent right-sided involvement than left-sided involvement. A “pocket sign,” defined as the pouch formed by the pelvic peritoneum, which is located in the surrounding retroperitoneal tissues extending toward the sciatic notch, was hypothesized to play an important role in the pathogenesis of sciatic nerve endometriosis. The sigmoid might protect the left lumbosacral plexus and sciatic nerve from direct endometriotic involvement by impeding the access of endometrial cells to the pockets located in the posterior aspect of the left hemipelvis. Early recognition of endometriotic infiltration and timely intervention are necessary to prevent permanent damage of the sciatic nerve. Neurolysis plus resection of the endometriotic foci are effective procedures. For trained laparoscopic surgeons possessing insight into retroperitoneal pelvic (neuro) anatomy, laparoscopic neurolysis of the sciatic nerve is a feasible but challenging procedure. The location of the sciatic lesion in our patient produced limitations for either the laparoscopic or transgluteal approach to safely and adequately expose the sciatic nerve. As a result, a novel combination of both approaches was proposed. Generally, a shorter interval between the onset of motor deficits and decompression is related to a better outcome. Progressive improvement in muscle strength and pain relief is often achieved soon after neurolysis of the sciatic nerve. With delayed diagnosis and intervention, total recovery of motor function is unlikely. In conclusion, women with symptoms of menstruation-related cyclic sciatica should be suspected of having endometriosis involving the sciatic nerve. MRI is necessary for diagnosis. When a laparoscopic or a transgluteal approach fails to result in complete excision of the endometriotic lesions and fails to achieve neurolysis of the sciatic nerve, combining both approaches with cooperation from gynecologists, orthopaedists, and microsurgical experts can be particularly effective.
Reference: Jiang H, Liang Y, Li L, Gu L, Yao S. Cyclic sciatica due to endometriosis of the sciatic nerve: neurolysis with combined laparoscopic and transgluteal approaches: a case report. JBJS Case Connector. 2014 Jan 22;4(1):e11.
Peritoneal carcinoma
Metastatic colon adenocarcinoma
Endometriosis involving sciatic nerve
Peritoneal tuberculosis
Metastatic cervical cancer

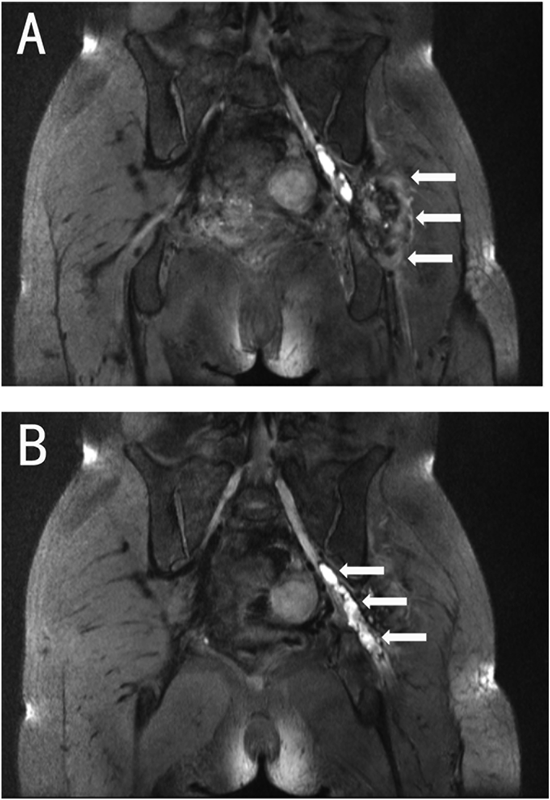
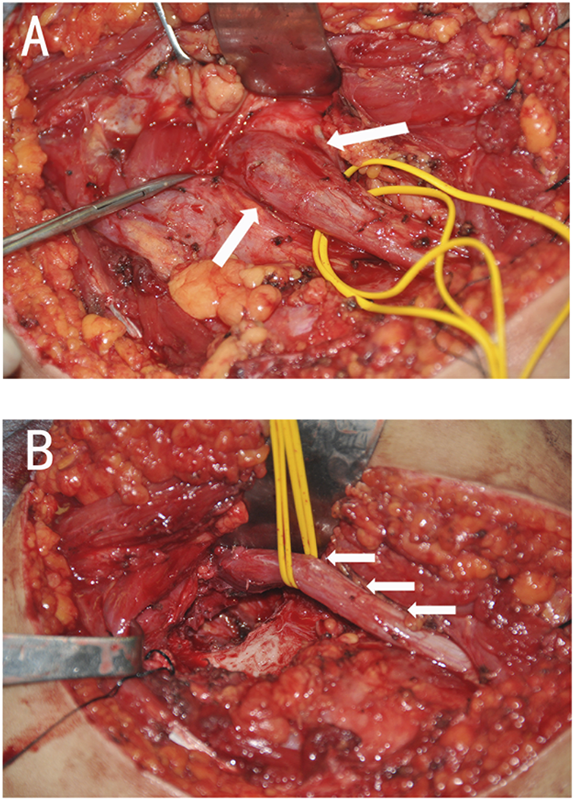
 Fig. 1
Fig. 1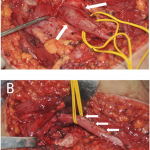 Fig. 2
Fig. 2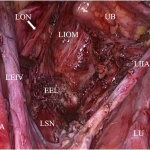 Fig. 3
Fig. 3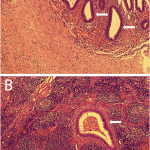 Fig. 4
Fig. 4