A 48-Year-Old Woman with Intermittent Groin Pain
December 21, 2016
A 48-year-old woman presented with a 12-month history of intermittent pain in the groin and left buttock on exertion. Thereafter, she developed radiating pain in the left lower limb. Palpation of the lumbar (L3-L5) facet joints and left groin was painful, the left hip displayed a mild decrease in extension-flexion (0°-0°-110°), and internal and external rotation with the hip in flexion measured 20°-0°-30°, with a positive anterior impingement sign. The neurological status was normal. Pelvic and lower-spine radiographs showed a mild borderline dysplasia of the left hip and mild osteoarthritis of the facet joints. An axial radiograph of the left hip showed signs of an uneven anterior head-neck junction with a normal to slightly increased α angle on the lateral view (Fig. 1).
Three weeks later, the patient reported increasing lower-back pain and aggravation of radiating pain to the left lower limb. Magnetic resonance arthrography (MRA) of the left hip showed mild cranial acetabular retroversion, a slight abnormality of the head-neck junction with a mildly increased α angle of 52°, and a small anterosuperior labral tear (Fig. 2). Magnetic resonance imaging (MRI) of the lumbar spine showed bilateral degeneration of the facet joints and a moderate bilateral foraminal stenosis at L5-S1 without evidence of neural root compression.
Over the following 7 months, the patient was managed conservatively, without improvement. Several periradicular infiltrations of the L5 nerve root with use of betamethasone and 1% lidocaine provided only limited alleviation of the pain in the lower limb.
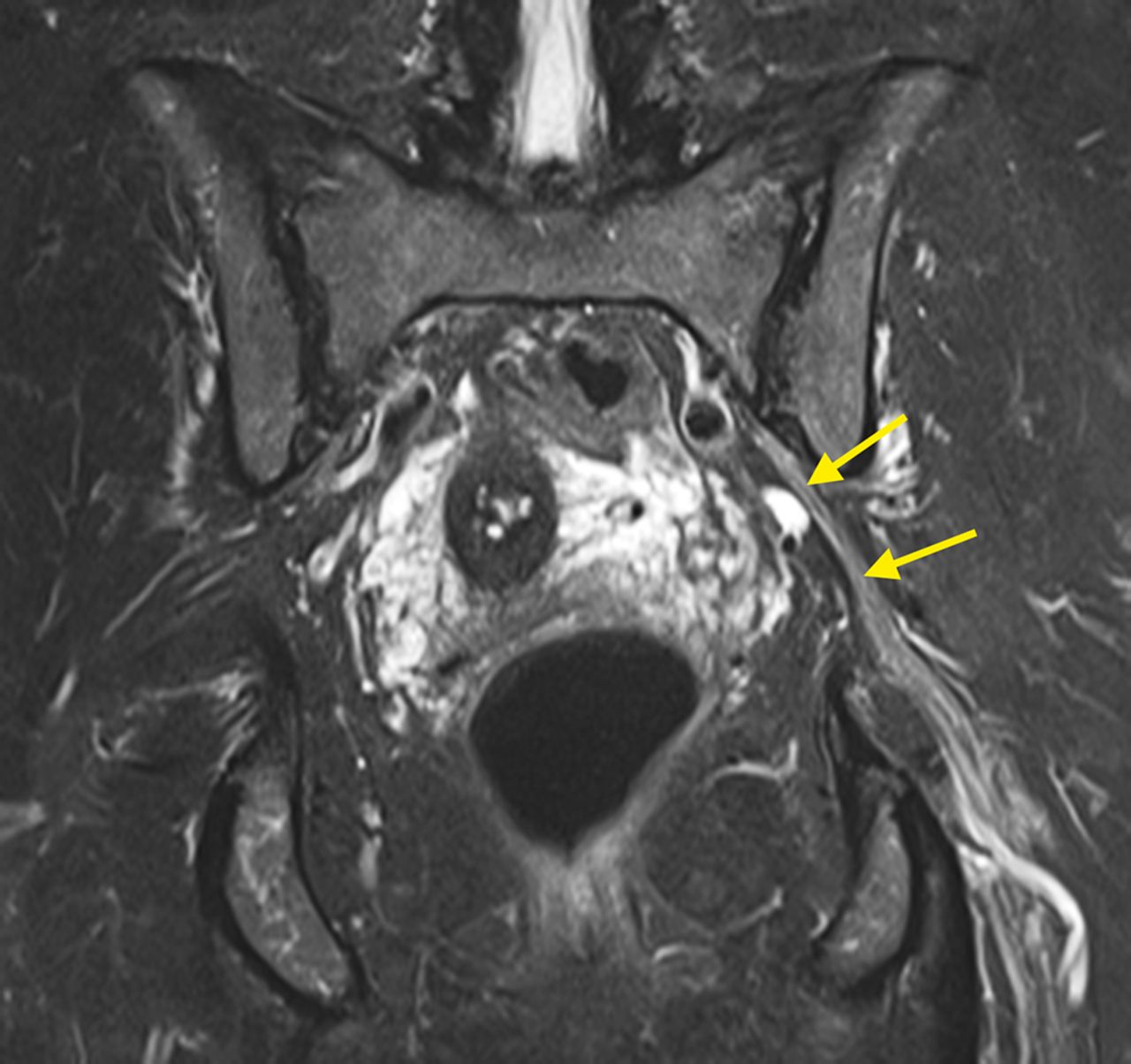
Seven months later, MRI of the pelvis revealed a 10-cm-long lesion that had a filiform origin at the dorsal aspect of the hip joint and continued in a pearl-necklace-like form along the obturator internus muscle. Epineurally accompanying the sciatic nerve, it extended through the greater sciatic notch, with a maximum diameter of 10 mm. On its intrapelvic course, the lesion caused severe L5 root compression, which was highly indicative of an intraneural pathway. MRI displayed a distended sciatic nerve with an endogenous intraneural mass. The quadratus femoris muscle showed edema and fatty degeneration (Figs. 3-A through 3-E).
A comparison of the recent MRI findings with the initial MRA scans revealed the presence of the initially overlooked lesion in the previous images and clearly demonstrated a connection to the joint cavity through a capsular tear. Electromyographic and neurographic assessments of the tibial and peroneal nerves were normal. A laparoscopic approach would have addressed only the intrapelvic portion of the lesion and would have been associated with a high risk of recurrence. We favored addressing the origin of the lesion and expected that open resection of the extrapelvic portion combined with labral refixation via surgical hip dislocation would result in resorption the intrapelvic portion.
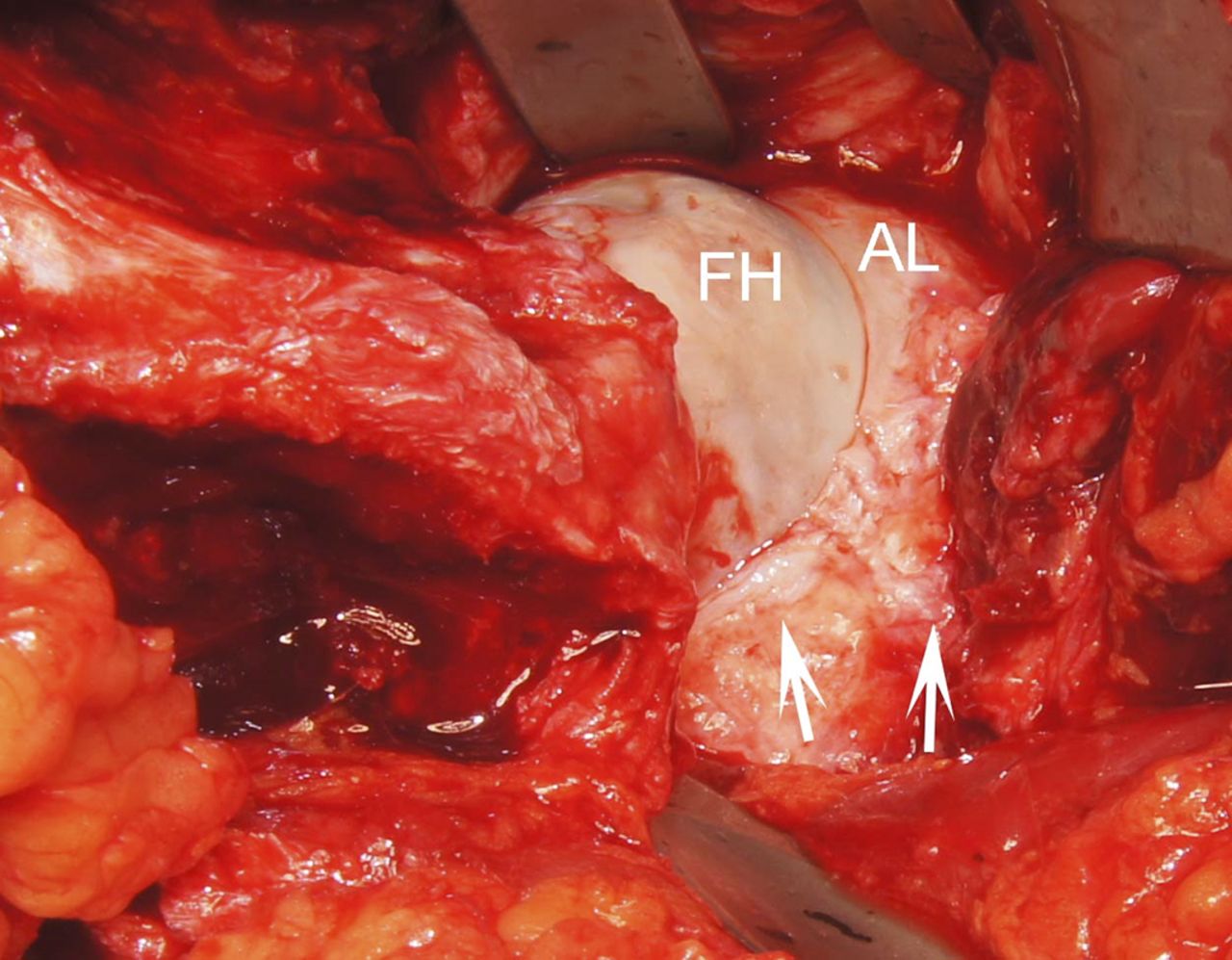
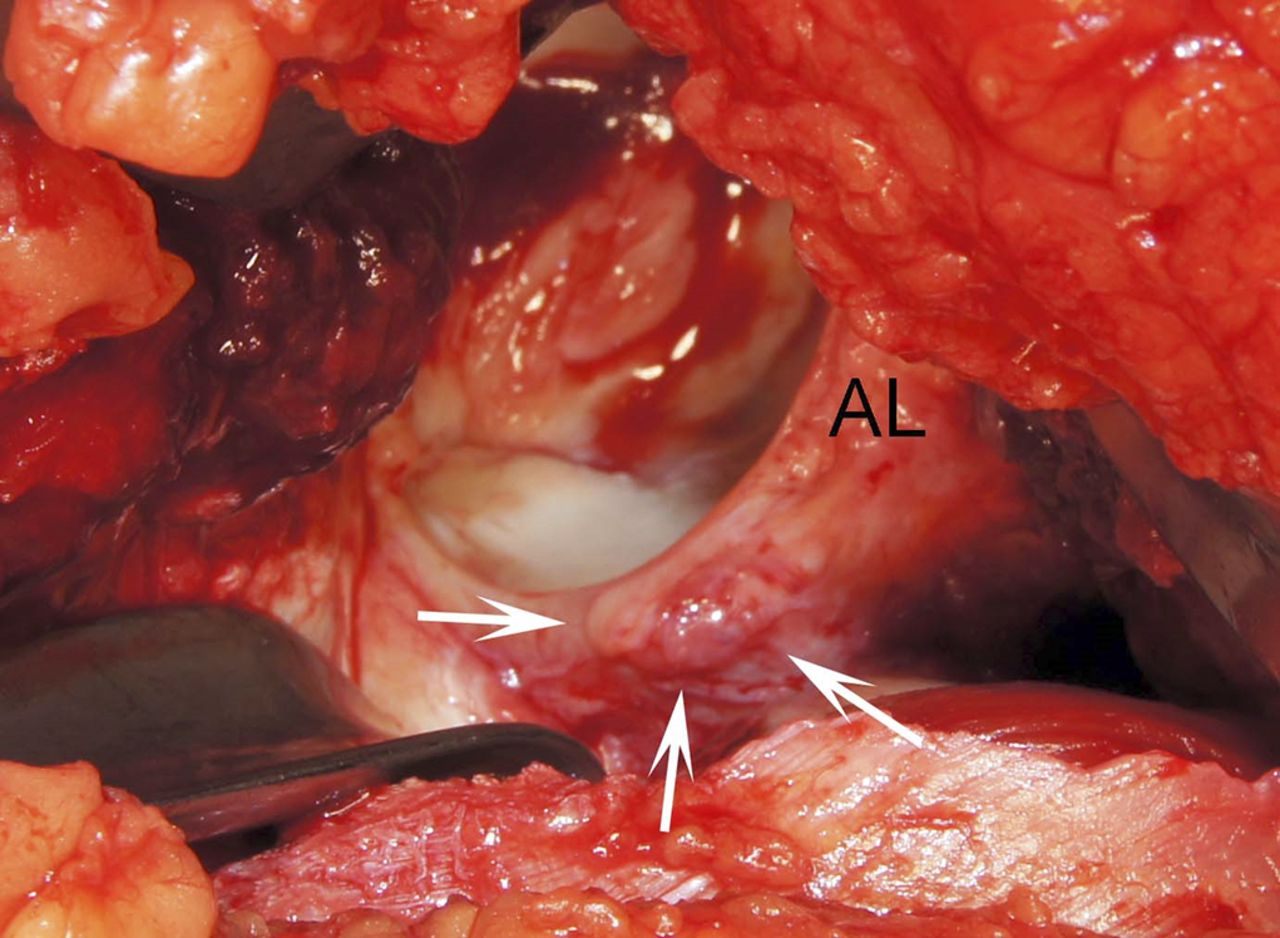
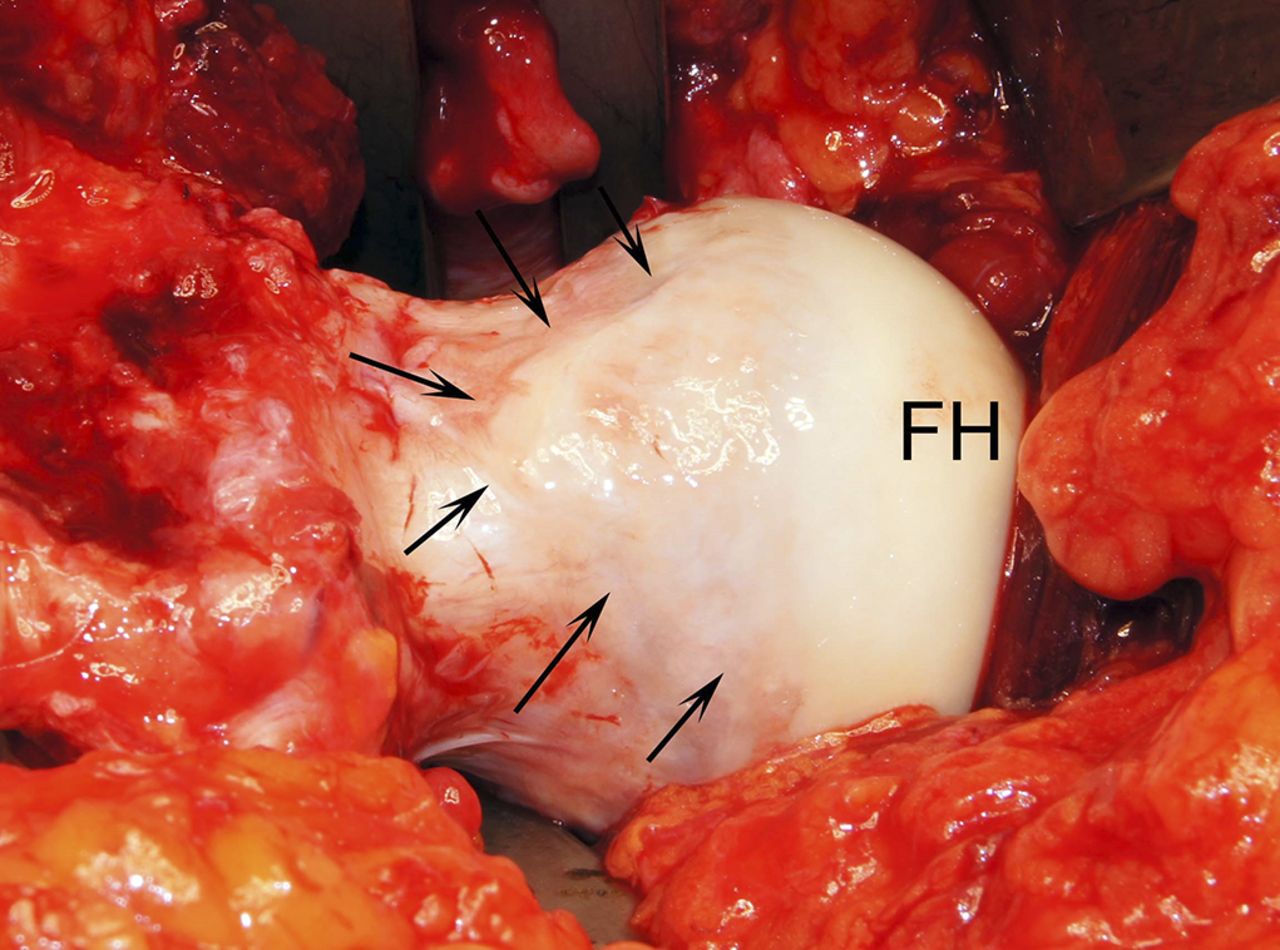
Surgery was performed through a posterolateral approach with the patient in the lateral decubitus position. A trigastric trochanteric step-cut osteotomy, with all external rotators being left attached to the femur, was performed to protect the course of the medial femoral circumflex artery. Toward the sciatic notch, a tightly filled, epineurally located ganglion was found to be causing the nerve compression. Following the piriformis muscle, the cyst continued to the posterior margin of the hip-joint capsule. Intra-articular findings showed a mild cam-type deformity in an anterosuperior position (Figs. 4-A through 4-D). In contrast to the preoperative MRI findings, there was no labral tear as had been previously suspected. The origin of the ganglion could be identified in the posterior position. The extrapelvic portion of the ganglion was excised macroscopically from the labrum up to the sciatic notch without opening of the epineural sheath. Furthermore, an offset correction of the femoral head was performed. After reduction of the femoral head and fixation of the trochanteric osteotomy with two 4.5-mm screws, no residual mass was palpable over the course of the sciatic nerve. Correct repositioning and fixation were confirmed on immediate postoperative radiographs. Histological analysis of the fragmented tissue sample showed a ganglion cyst without a clearly identifiable synovial lining.
Clinical follow-up examinations at 3, 6, and 12 months postoperatively indicated relief of the femoroacetabular impingement (FAI)-related symptoms, with improved left hip extension-flexion (0°-0°-125°), internal-external rotation (55°-0°-40°), and abduction (50°). The impingement test revealed only mild tenderness on internal rotation. The previous radicular pain in the left lower limb stemming from the nerve compression had been reduced to only numb discomfort. At 6 months, radiographs showed complete union of the trochanteric osteotomy site and sufficient correction of the femoral offset (α angle, 37°; offset, 8 mm). At 12 months, MRI showed complete recovery of the sciatic nerve without signs of residual cystic structures (Fig. 5).
Proceed to Discussion >>Reference: Briem T, Haemmerle G, Kramers-de Quervain I, Leunig M. Synovial ganglion of the hip as a rare cause of L5 radiculopathy. A case report. JBJS Case Connect. 2016 Jul 27;6(3):e59.
The initial presentation of this patient with pain in the buttock, pain in the left groin, and radiating pain in the left lower limb as well as a moderate bilateral foraminal L5-S1 stenosis led to our first impression of an intraspinal reason for sciatica, despite the patient’s substantially decreased hip function. Most radicular pain that is caused by an intraspinal source is greater in the leg than in the back. In contrast, our patient initially presented with pain that was predominantly located in the buttock and groin. The second MRI, in fact, confirmed an extraspinal cause of sciatica.
There are different types of cystic lesions. Ganglion and synovial cysts are similar in terms of clinical and radiographic presentation. However, ganglion cysts are lined with connective tissue, whereas synovial cysts have a synovial-cell lining. Our MRI findings clearly showed an intra-articular connection of the ganglion to the joint cavity, which strongly indicated a synovial lining suggestive of a synovial ganglion. In most cases, synovial ganglia are located in the vicinity of the knee or wrist joint. As synovial ganglia may be associated with degenerative disease, the formation of a synovial ganglion in our patient was considered unlikely because there were only mild degenerative findings. In the hip, elevated intra-articular pressure is required to force the synovial fluid into the acetabulum or surrounding soft tissue, which can cause a paralabral ganglion cyst. Therefore, we hypothesized that the finding of mild cam-type FAI might have been contributing to this pathomechanism. It is potentially feasible that mild instability might have led to a capsular rent that was causing the described symptoms. As cam decompression improved the clinical findings in our patient, our proposal seems valid.
In general, the finding of a large symptomatic synovial ganglion of the hip is rare. Most cases are associated with compression of neurovascular structures anterior to the hip. In the case of our patient, the cyst was oriented posteriorly. MRI findings of an endogenous mass within the distended sciatic nerve strongly suggested an intrapelvic, intraneural course of the ganglion (Fig. 3-D). Spinner et al. presented a clinical report describing 5 patients with intraneural ganglia affecting the sciatic nerve or lumbar plexus, with a connection to the posteromedial aspect of the hip. They proposed a unified theory to explain the formation and propagation of these intraneural cysts involving an articular branch connection to a synovial joint. In line with this proposal, our MRI findings of edema and fatty degeneration of the quadratus femoris muscle (Fig. 3-E) support the idea of the cyst following an articular branch of the lumbar plexus. The innervation pattern of the hip typically includes articular branches from the sciatic, superior gluteal, quadratus femoris, obturator, and femoral nerves. The nerve to the quadratus femoris supplies the posteromedial region, which was consistent with the intraoperative finding of the origin of the cyst. Moreover, it is believed that capsular weakness or deficiency may favor cyst development. Thus, it seems likely that, in our patient, the mild cam-type deformity contributed to the hip capsule lesion.
Other reports dealing with tibial and peroneal intraneural ganglia and considering the unified theory have highlighted the importance of treating the underlying pathological mechanism, including resection of the articular branch and drainage of the cyst. As we did not address the intrapelvic part of the lesion, additional clinical and radiographic follow-up was being maintained at the time of writing. Complete ganglion regression at 12 months postoperatively is consistent with the decrease in L5 radiculopathy.
The initial MRI findings were misinterpreted because the triad of pain in the buttock, groin, and lower limb could not be attributed to a single underlying pathological lesion, although the cyst was perfectly visible. This case highlights the fact that a combined presentation of symptoms attributable to intrinsic hip disease and peripheral radiculopathy should raise suspicion for a shared cause of these entities. The identification of a possible joint connection in cases of juxta-articular ganglia is crucial as failure to recognize and adequately treat the joint connection might lead to relapse.
Reference: Briem T, Haemmerle G, Kramers-de Quervain I, Leunig M. Synovial ganglion of the hip as a rare cause of L5 radiculopathy. A case report. JBJS Case Connect. 2016 Jul 27;6(3):e59.
What is the diagnosis?
Plexiform neurofibroma
Cystic schwannoma
Cystic synovial ganglion
Echinococcal cyst
Intraneural lipoma

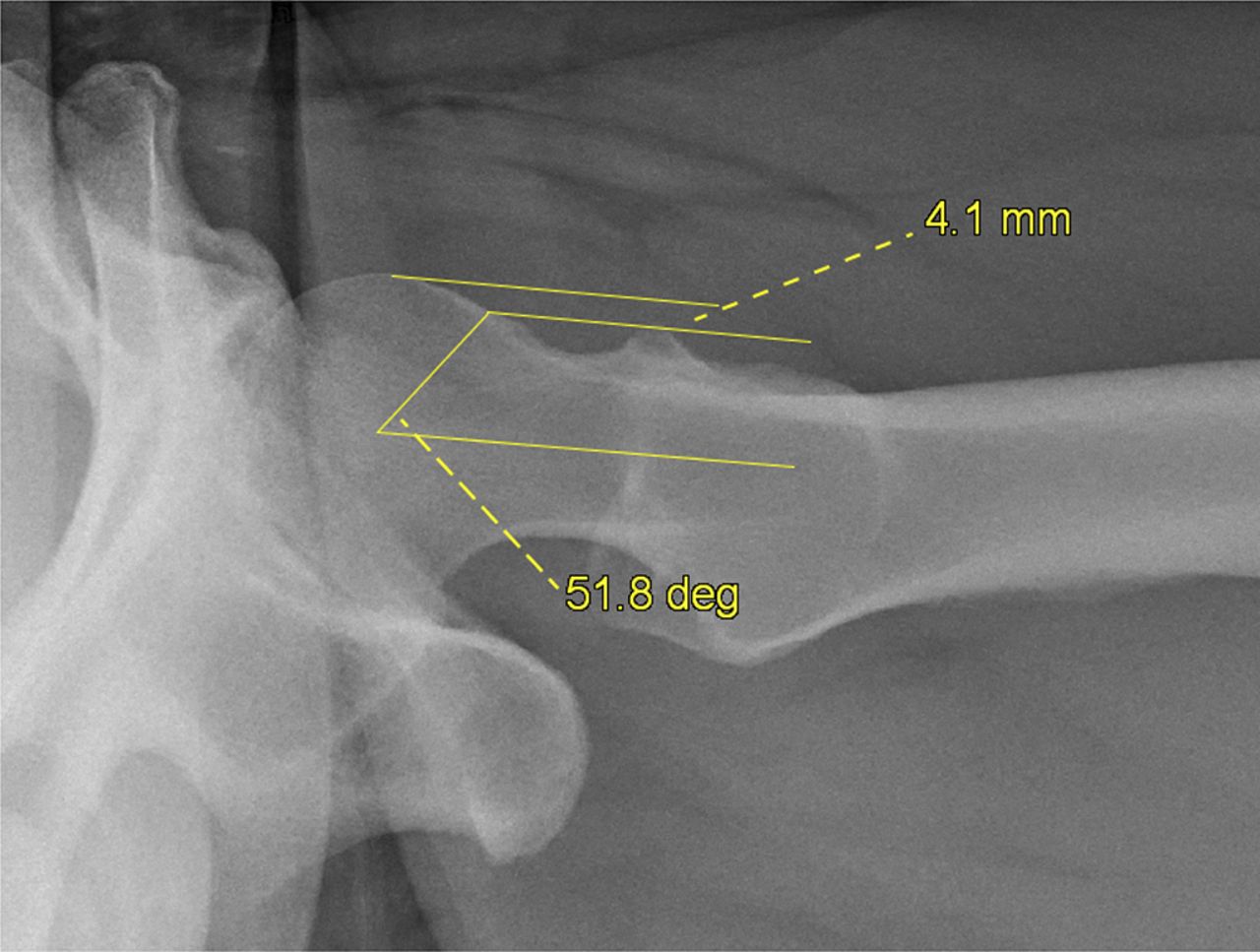
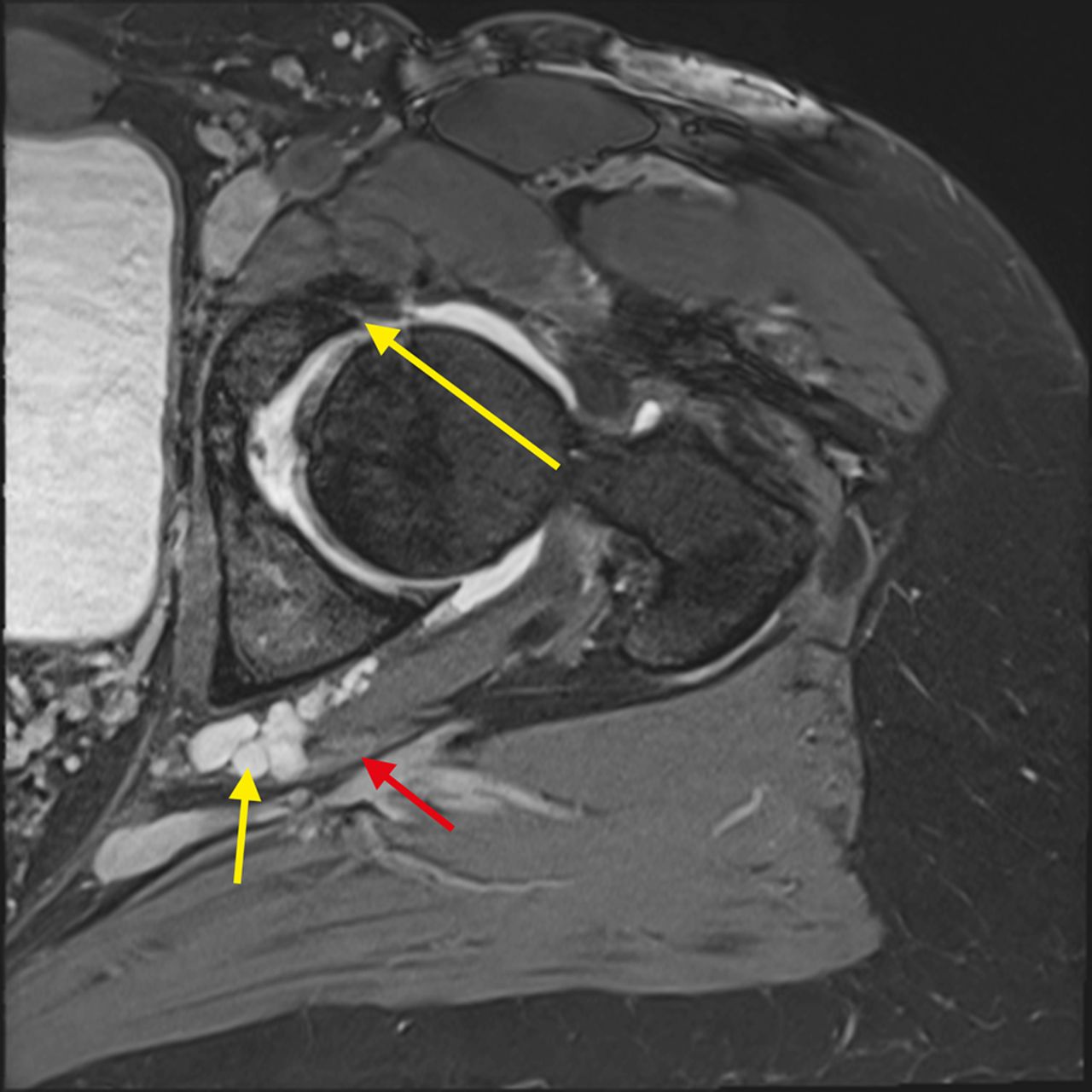
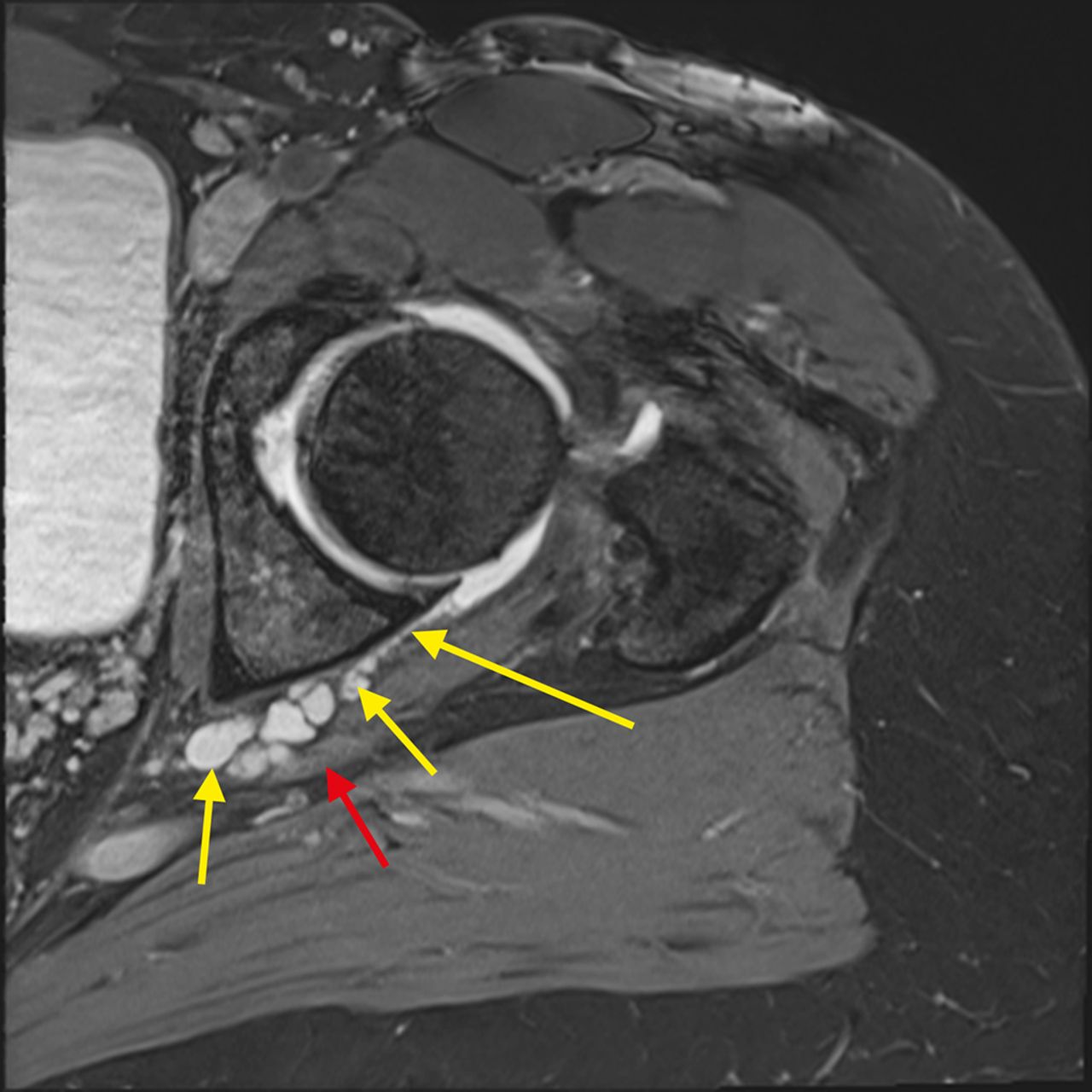
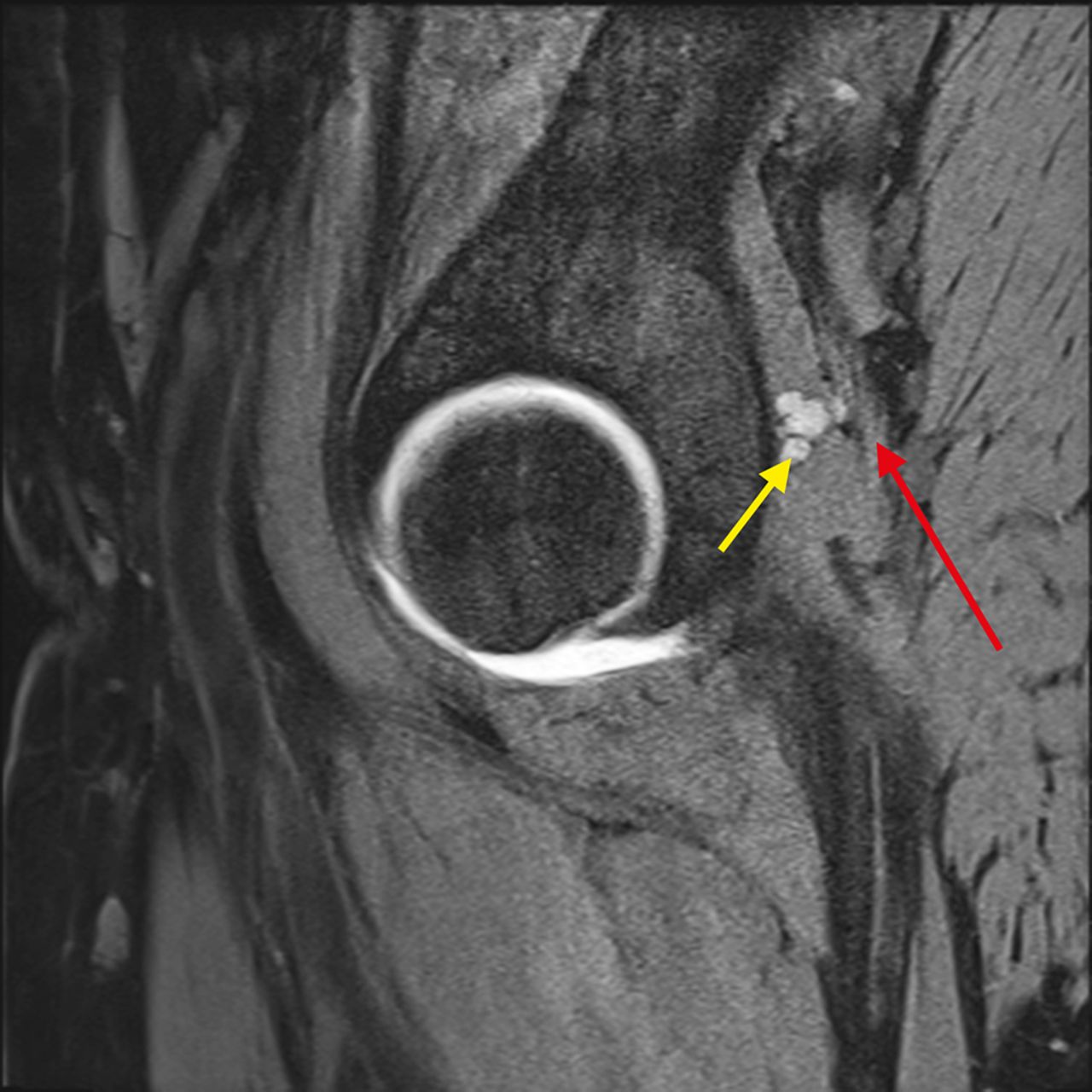
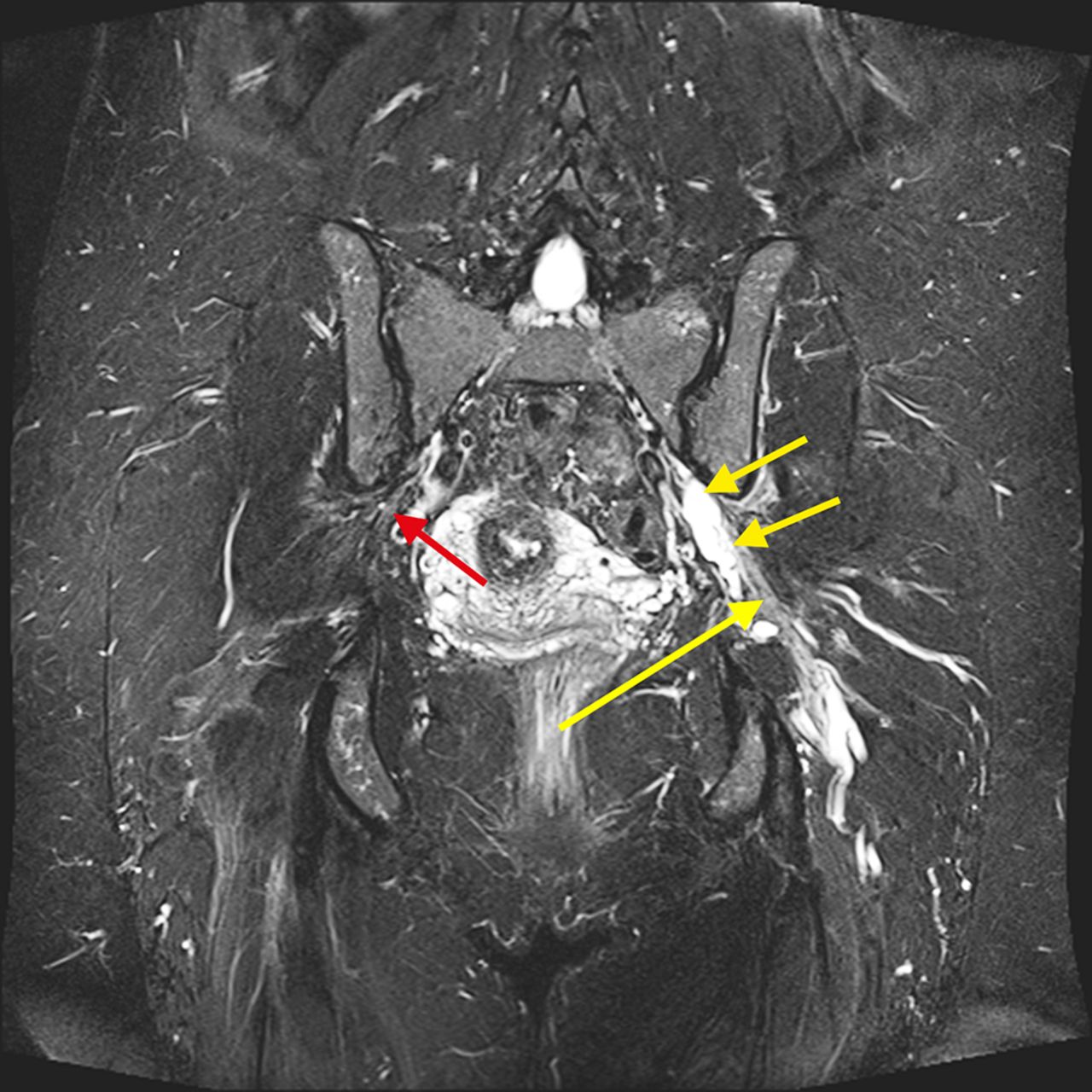
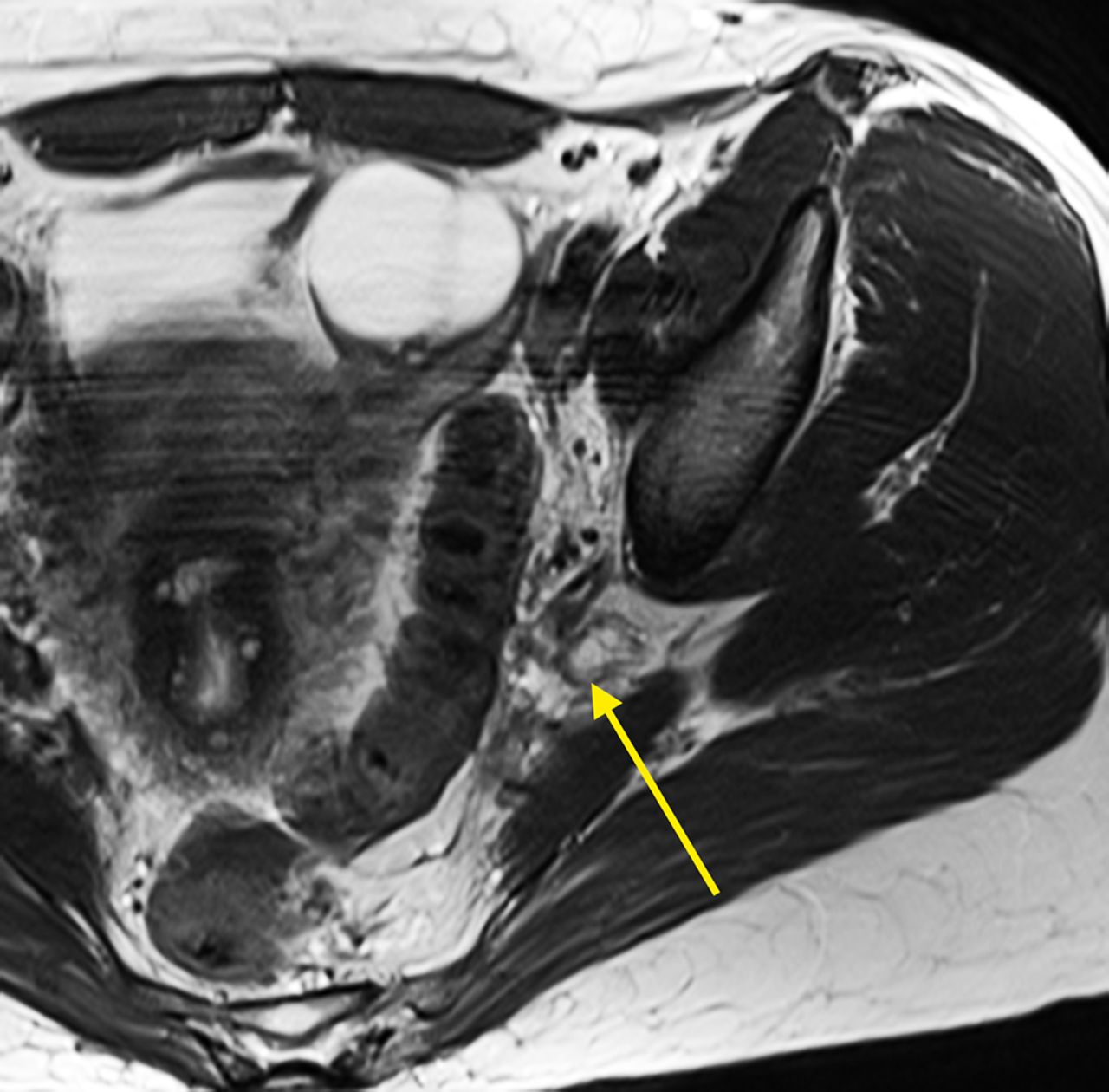
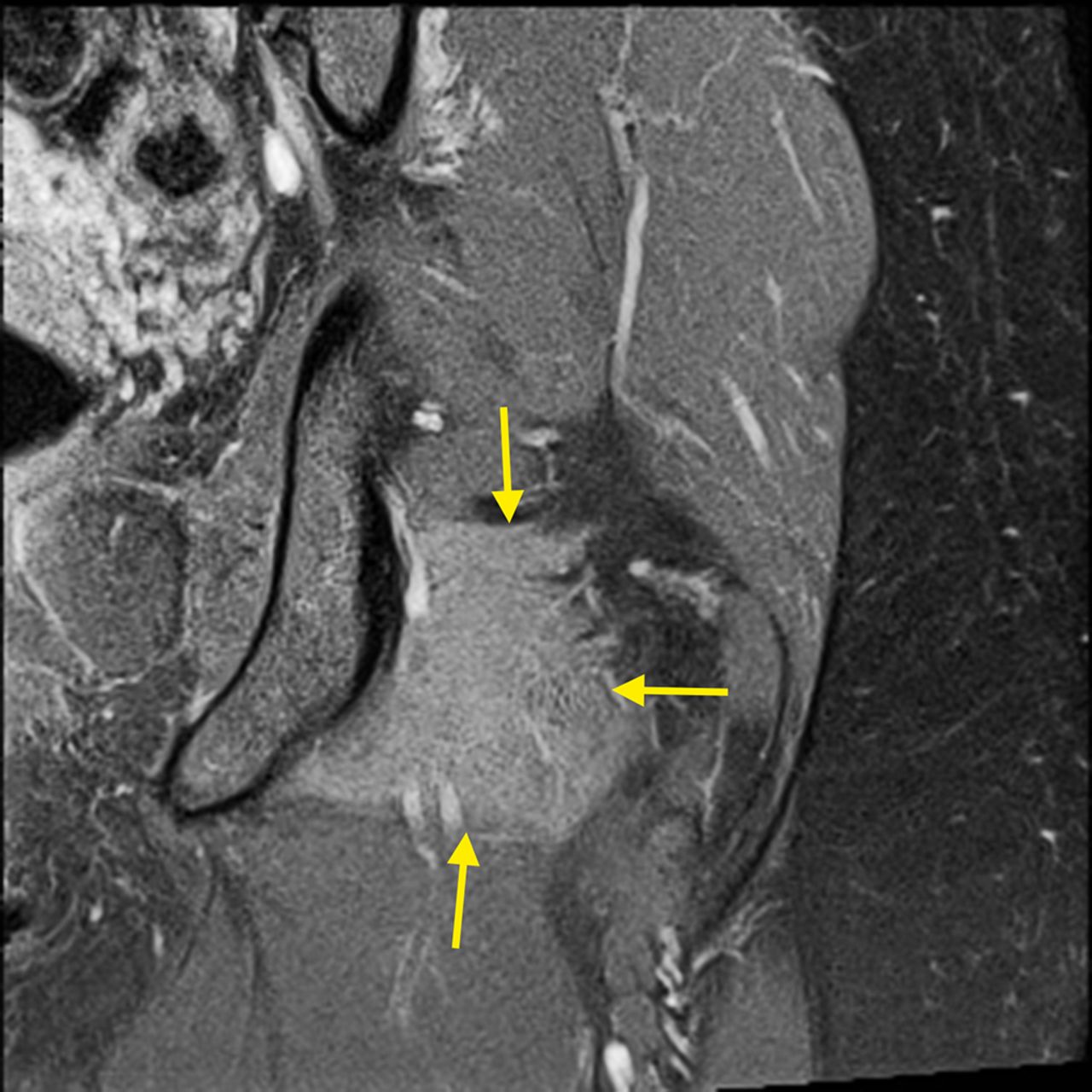
 Fig. 1
Fig. 1 Fig. 2
Fig. 2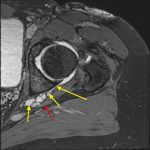 Fig. 3-A
Fig. 3-A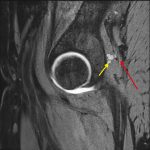 Fig. 3-B
Fig. 3-B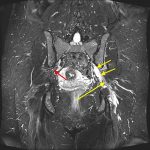 Fig. 3-C
Fig. 3-C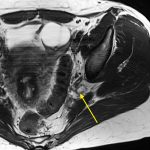 Fig. 3-D
Fig. 3-D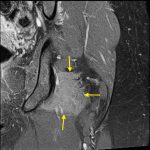 Fig. 3-E
Fig. 3-E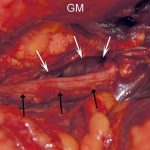 Fig. 4-A
Fig. 4-A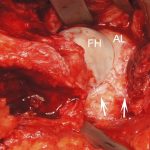 Fig. 4-B
Fig. 4-B Fig. 4-C
Fig. 4-C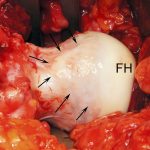 Fig. 4-D
Fig. 4-D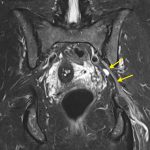 Fig. 5
Fig. 5