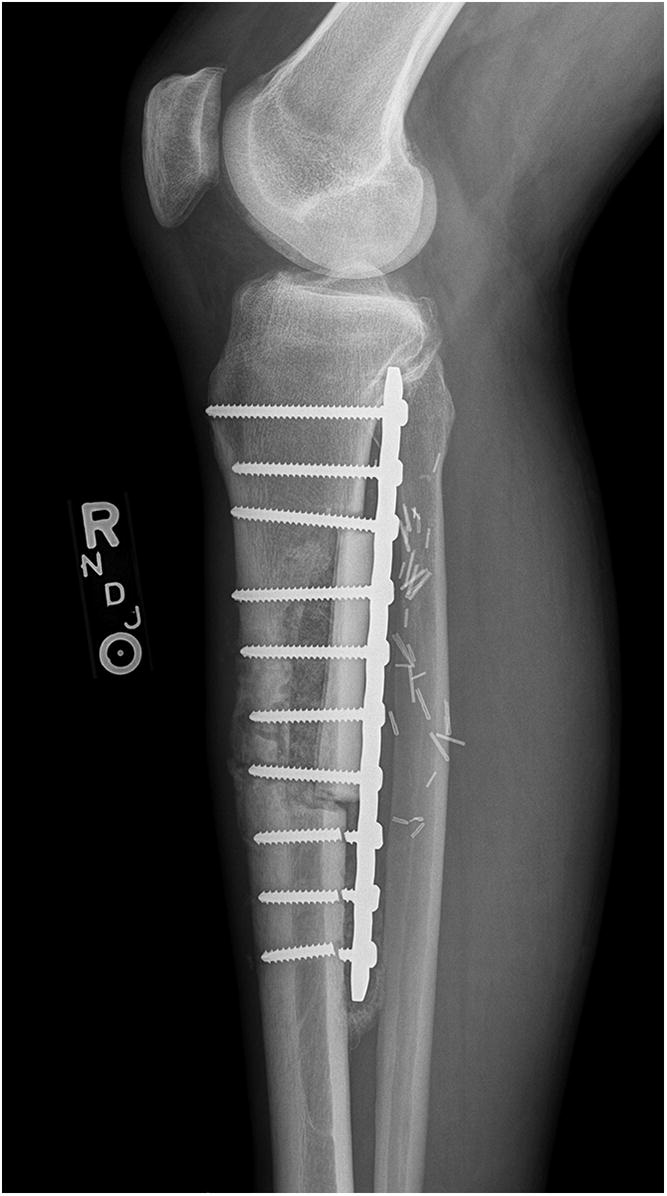
A 65-year-old man with no noteworthy medical history presented to urgent care in June 2015 with progressively worsening right calf pain after driving for approximately 8 hours. He was sent to the emergency department for a suspected deep vein thrombosis. An ultrasound of the lower extremity showed no evidence of thrombosis, but revealed a soft-tissue mass in the calf. Radiographs of the tibia were within normal limits, with subtle vascular calcifications (Fig. 1). Magnetic resonance imaging (MRI) revealed a 6.3 × 4.1 × 2.9-cm heterogeneous mass located in the deep posterior compartment of the leg, involving the proximal tibial diaphysis, without intraosseous involvement (Figs. 2 and 3).
The patient was referred to an orthopaedic oncologist, and a computed tomography (CT)-guided biopsy of the mass was performed through a posteromedial approach.
Routine hematoxylin and eosin staining showed findings similar to those seen in Figure 5. The lesion was also positive for vimentin and CD99, and negative for cytokeratins (AE1/AE3 and CAM5.2), S100, CD31, CD34, human melanoma black (HMB-45), CD3, CD20, desmin, and terminal deoxynucleotidyl transferase (TdT). An additional specimen was positive for EWSR1 gene rearrangement by analysis with fluorescent in situ hybridization (FISH).
After transferring care to our institution, the patient was started on neoadjuvant chemotherapy in August 2015 with vincristine, doxorubicin, and cyclophosphamide (VAC), alternating with ifosfamide and etoposide for a total of 5 cycles. Because of an adverse reaction that included fever and rash, the ifosfamide and the etoposide were discontinued after 2 cycles. The vincristine was discontinued after the third cycle when the patient developed an ileus. Neoadjuvant chemotherapy was completed in December 2015; repeat MRI showed a reduction in tumor size to 3.6 × 3.3 × 2.0 cm (Fig. 4). The patient subsequently underwent wide resection.
With the patient in the prone position, a longitudinal incision was made on the posteromedial aspect of the leg, entering the deep posterior compartment. Several flexors in the deep compartment were taken with the lesion as a soft-tissue margin. A burr was used circumferentially to begin resection of the mass, and a large osteotome was used to complete the resection. A 9.0 × 4.5 × 4.0-cm bone and soft-tissue mass was removed. The mass involved the periosteum, with <0.1-cm involvement of cortical bone. The margins were negative.
Hematoxylin and eosin staining of sections is shown in Figures 5 and 6.
The pathology of the resection specimen confirmed the diagnosis of the original biopsy of periosteal Ewing sarcoma.
The patient underwent reconstruction with a cortical allograft and plate fixation (Figs. 7 and 8). He tolerated the procedure well and was discharged home.
Six weeks postoperatively, the patient started adjuvant chemotherapy with cyclophosphamide and dactinomycin every 3 weeks for a total of 12 cycles. During chemotherapy, and also likely because of early weight-bearing, the patient had a failure of the allograft reconstruction with an anterior tibial cortex fracture and distal hardware failure (Figs. 9 and 10). The tibial reconstruction was revised with bulk allograft and an intramedullary nail (Figs. 11 and 12). The postoperative course was uneventful. CT of the chest 1 year from the start of treatment showed no change in the stable lung nodule and no new evidence of metastatic disease.
Proceed to Discussion >>Reference: Bedard J, Burns J, de Comas A. Periosteal Ewing sarcoma in a 65-year-old man: a case report. JBJS Case Connect. 2017 Apr 26;7(2):e27.
Ewing sarcoma is a primary bone malignancy most commonly found in pediatric patients. This tumor occurs in medullary, extraskeletal, and periosteal forms (in decreasing order of frequency). Medullary Ewing sarcoma accounts for about 90% of all cases, while only a few dozen cases of the periosteal form have been reported. Compared with the more common medullary and extraskeletal forms, periosteal Ewing sarcoma has a marked male predominance, typically lacks presenting metastases, and more frequently affects the proximal aspect of the extremities. In a review of 29 cases of periosteal Ewing sarcoma, the average patient age was 16.8 years, ranging from 11 to 36 years. The diaphysis of long bones was most commonly involved, with tumors occurring most frequently in the femur, followed by the humerus, the tibia, the fibula, and the scapula. In our patient, MRI confirmed the periosteal origin of the mass and demonstrated no medullary involvement.
Approximately one-quarter of patients with medullary Ewing sarcoma have detectable metastases at presentation. The 5-year relapse-free survival rate for patients without initial metastases approaches 60%. For patients with metastases at diagnosis, the 5-year survival rate drops to 22%. Approximately 30% to 40% of patients experience recurrent disease, with survival rates similar to those for patients with metastatic disease. For older patients with medullary Ewing sarcoma, the prognosis is unclear. While some studies show no difference in prognosis among age groups, other studies indicate inferior survival for patients >40 years old. Periosteal Ewing sarcoma typically has a less aggressive clinical course and is associated with a better prognosis. This is potentially because of the localization in the space surrounded by cortical bone and periosteum, resulting in reduced risk of metastases. In a retrospective study of 29 patients with periosteal Ewing sarcoma, 88% of patients had an uneventful course of treatment. Ewing sarcoma is generally treated with the VAC protocol and wide surgical resection. Because there is substantial variation among chemotherapy and radiation protocols, as well as the need for surgical resection for small round blue-cell tumors, it is critical to confirm the diagnosis. In the case of periosteal Ewing sarcoma, hemicortical resection may be performed because there is, by definition, no medullary involvement. A unicortical segment of bone is sufficient to obtain a negative margin. This is vastly different from conventional Ewing sarcoma, which requires total resection circumferentially.
The histologic features of periosteal Ewing sarcoma, characterized by uniform small round cells, are analogous to the medullary and extraskeletal forms. These cells have round nuclei containing fine chromatin and scanty clear or eosinophilic cytoplasm with indistinct cytoplasmic membranes. Because this histology has a wide differential diagnosis, including rhabdomyosarcoma, small-cell osteosarcoma, neuroblastoma, malignant lymphoma, Merkel cell carcinoma, and desmoplastic small round cell tumors, additional diagnostic studies are necessary. No specific immunohistochemical markers for Ewing sarcoma exist, although cells are immunoreactive to vimentin, and the cell membrane protein CD99 is consistently expressed. The use of molecular analysis is becoming increasingly important in identifying gene rearrangements in soft-tissue tumors. Ewing sarcoma is characterized by a balanced reciprocal translocation, t(11;22)(q24;q12), which encodes an oncogenic transcription factor. The most common fusion protein product is EWS-FLI1, found in over 85% of patients with Ewing sarcoma. In this combination, EWS, a gene belonging to the TET family of RNA-binding proteins, fuses with FLI1, a member of the ETS family of transcription factors. While the EWS-FLI1 translocation is the most common, other translocation permutations of the TET family and the ETS family have been identified in the pathogenesis of Ewing sarcoma. FISH is increasingly being used to identify EWS, also known as EWSR1, gene rearrangements in confirming the diagnosis of Ewing sarcoma. In our patient, CD99 positivity and FISH demonstrating EWSR1 rearrangement confirmed the diagnosis of Ewing sarcoma.
To our knowledge, this case represents the first report of periosteal Ewing sarcoma in a 65-year-old patient. He underwent standard treatment for the sarcoma and had an excellent short-term outcome. While periosteal Ewing sarcoma is rare, especially in an older individual, it is an important consideration in the differential diagnosis of masses presenting in soft tissues near bone.
Reference: Bedard J, Burns J, de Comas A. Periosteal Ewing sarcoma in a 65-year-old man: a case report. JBJS Case Connect. 2017 Apr 26;7(2):e27.
What is the diagnosis?
Periosteal osteosarcoma
Synovial sarcoma
Periosteal Ewing sarcoma
Malignant lymphoma
Parosteal osteosarcoma



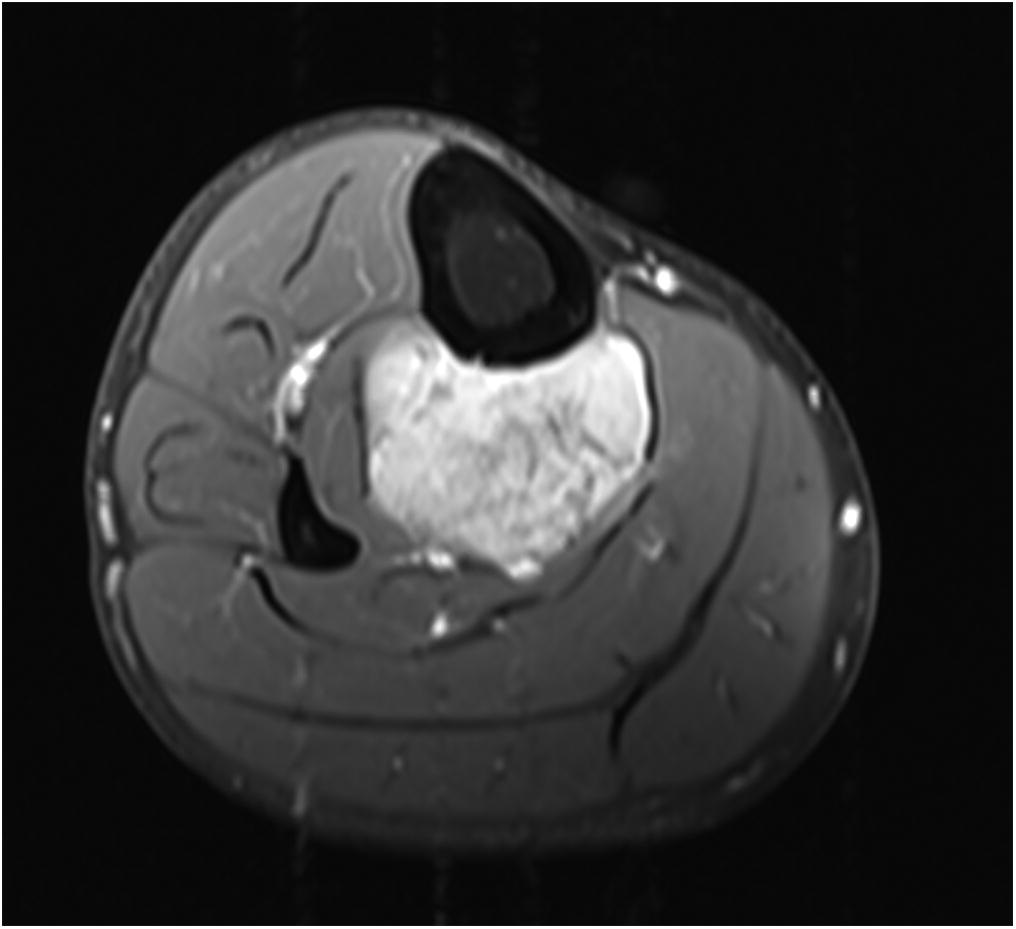
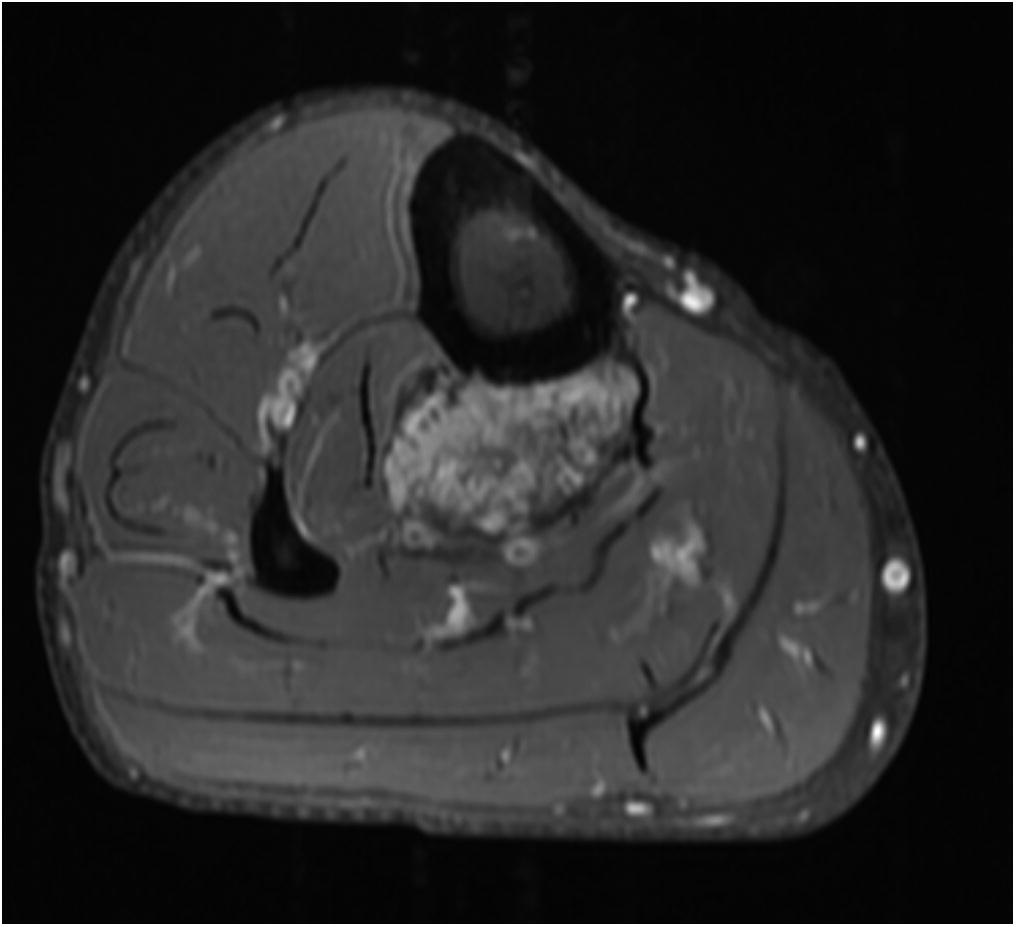
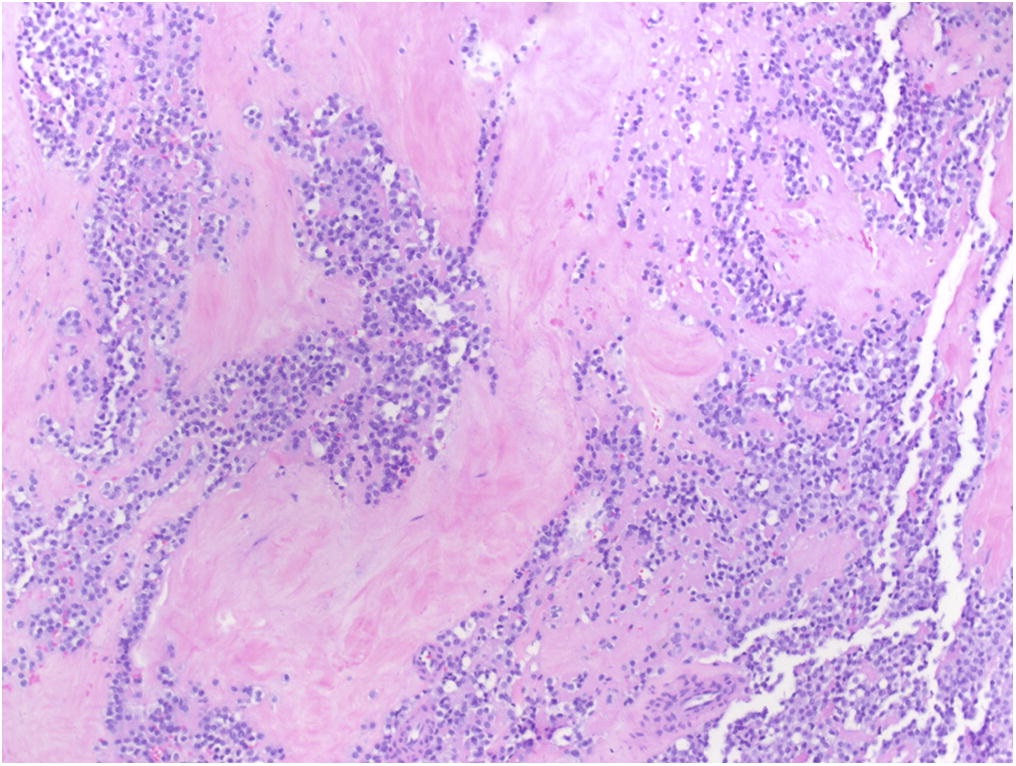
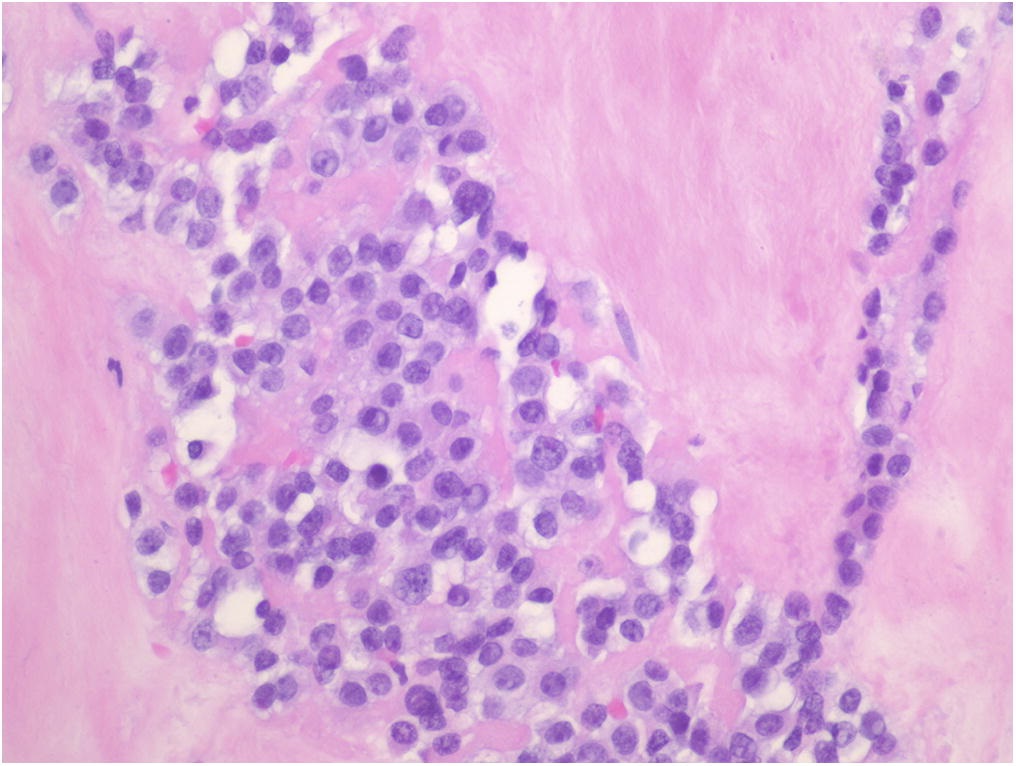
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4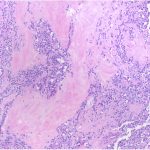 Fig. 5
Fig. 5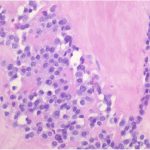 Fig. 6
Fig. 6 Fig. 7
Fig. 7 Fig. 8
Fig. 8 Fig. 9
Fig. 9 Fig. 10
Fig. 10 Fig. 11
Fig. 11 Fig. 12
Fig. 12