A 45-Year-Old Woman with Osteoarthritis of the Hip
July 7, 2021
A 45-year-old woman presented with end-stage osteoarthritis of the left hip. All conservative treatment measures had been exhausted, and she therefore underwent total hip arthroplasty. The patient was positioned in the right lateral decubitus position, and a posterior approach to the hip was used. Successful implantation of a cementless acetabular cup and polyethylene liner was executed (Trilogy; Zimmer). During preparation of the femoral canal for a cementless, modular stem (Fibermetal Midcoat; Zimmer), a complication occurred. After discussion with the family the arthroplasty was completed, and after subsequent discussion with the asymptomatic patient, no further intervention was attempted. Imaging studies were obtained at regular intervals, including at 8 years after the arthroplasty (Figs. 1 and 2-A through 2-D).
Imaging studies confirmed the postoperative diagnosis of a dislodged and migrated trial femoral head.
During the trialing process at the arthroplasty, the trial femoral head became dislodged on dislocation of the hip and migrated anteriorly through the capsule. Manual retrieval of the trial femoral head was attempted, but it only migrated further into the pelvis. Retrieval was attempted with various instruments with no success. After various attempts were made at retrieval, it was believed that the only way to obtain the trial femoral head would be to use a different surgical approach. It was determined that the case would be completed, and a discussion would be held with the patient and her family postoperatively. The femoral stem implantation was finished, and the incision was closed. The radiographic images showed the location of the trial femoral head in the iliopsoas bursa, along the inner table of the pelvis. As noted above, the patient was asymptomatic, and, after extensive discussion, the patient opted to simply undergo observation and forgo any further intervention. The polymer composition of the trial femoral head, poly(etherimide), is a U.S. Food and Drug Administration–approved material that is chemically stable with no demonstrable biologic activity.
The patient had no complications with the left hip for approximately 14 years. She was seen at 2 weeks, 6 weeks, and 1 year, following the same postoperative protocol as all uncomplicated patients. She had no further symptoms of abdominal or pelvic discomfort and showed no signs of neurovascular compromise at any of these visits. She was seen at 2-year to 5-year intervals since then for either routine follow-up or for symptoms related to other joints. Given her lack of symptoms, continued observation was our treatment strategy. The patient was last seen 17 years after the index procedure and remained asymptomatic. Radiographs at that time did not suggest any migration of the retained trial femoral head.
Proceed to Discussion >>Reference: Wallis C, Ninomiya JT. Intrapelvic loss of a trial femoral head during total hip arthroplasty: a case report. JBJS Case Connect. 2020 Jul-Sep;10(3):e19.00118.
Intraoperative loss of a trial femoral head is an unfortunate and preventable complication of total hip arthroplasty. Although there are relatively few documented incidents of this complication, it has been suggested that this likely occurs more frequently than is reported. Most of the reports on this complication have described retrieving the trial femoral head either immediately or with a delayed surgical exposure. Various approaches have been described for successfully retrieving this foreign body, including the ilioinguinal, Stoppa, and proximal Smith-Peterson processes. One report described losing the trial femoral head during a direct lateral approach and then retrieving the trial femoral head via a posterior approach through the same incision. Most of these approaches were performed in a delayed fashion. There was 1 report of successful laparoscopic retrieval by a general surgeon. In addition, another case report described using a Satinsky aortic clamp to obtain the lost trial femoral head without use of an additional surgical approach.
There have been a few reports on the retention of the femoral head with a close follow-up. There is certainly concern that the retention of a large foreign body such as a trial femoral head may lead to the compression of nearby structures such as the iliac artery and vein and their branches, branches of the lumbosacral plexus, and the ureter. Some have also speculated that there is a risk of erosion into the gastrointestinal tract. Irritation of these structures should be tested by a complete neurovascular examination of both lower extremities and assessment for any abdominal or pelvic discomfort. Our patient did not display any abnormal symptoms or examination findings, and furthermore, the computed tomographic (CT) scan showed the trial femoral head positioned along the inner table of the ilium within the iliopsoas bursa, well away from any of these dangerous structures. Some of the patients who were under observation eventually required surgical removal of the trial femoral head because of either abdominal discomfort or a sensation of clicking in the pelvis where the trial was located. There has been no documentation of any neurovascular compromise, although again this is a feared complication of long-term retention of the component. Our patient was seen at 17 years after the index surgical procedure, and, at that time, radiographs showed no demonstrable migration of the trial femoral head within the pelvis. Given this finding along with the lack of any associated symptoms, it was mutually decided to not obtain any further imaging such as a CT scan.
Several preventative measures have been described to avoid this complication. It is important for any trainee or assistant to be aware of this potential obstacle and of the inherent modularity of the trial femoral head and ease of dislodging it. Perhaps the most commonly cited deterrent to successful retrieval is attempting this manually. Almost all case studies have shown that this has only served to push the trial femoral head further into the pelvis. Some studies have suggested packing the anterior capsule with a lap or gauze to prevent migration of the trial femoral head into the pelvis. Although this seems intuitive, this may interfere with an accurate test of stability when trialing components. One would think that this technique would be most appropriate if the anterior hip is packed only just before dislocation of the trial components, thus allowing accurate testing of stability. However, this variation would not prevent the trial femoral head from inadvertent dislocation or dislodging before planned dislocation after trialing.
Another strategy that has been described is the use of a necklace of trial femoral heads made from 2 number-2 heavy sutures run through the dome-holes of the components. This would allow easy retrieval of the component if it were to migrate into the pelvis and reportedly does not affect trialing accuracy of total hip arthroplasty components. The reporting institution has stated that there have been no cases of lost trial femoral heads since this strategy was implemented.
Although trial femoral head loss has been reported with both direct lateral and posterolateral approaches to total hip arthroplasty, some have suggested that patients are at increased risk with a direct lateral approach because of the anterior capsulectomy that accompanies this procedure. They also have indicated that increased soft-tissue tension in this approach also increases the risk of intraoperative trial femoral head loss.
Finally, it is imperative to have a thorough discussion with the patient and family, admitting to the unintended complication and outlining potential treatment strategies. This will encourage retained trust from the patient and promote informed decision-making going forward.
Although there are certainly measures that may prevent the intraoperative loss of a trial femoral head and methods to retrieve it once it has been lost, our experience with this 17-year follow-up shows that close observation alone is also a suitable treatment strategy.
Reference: Wallis C, Ninomiya JT. Intrapelvic loss of a trial femoral head during total hip arthroplasty: a case report. JBJS Case Connect. 2020 Jul-Sep;10(3):e19.00118.
What is the diagnosis?
Myositis ossificans
Fractured trunnion with retained chromium cobalt femoral head
Dislodged and migrated polymeric trial femoral head
Broken ceramic femoral head from a previous operation
Misplaced radiographic phantom


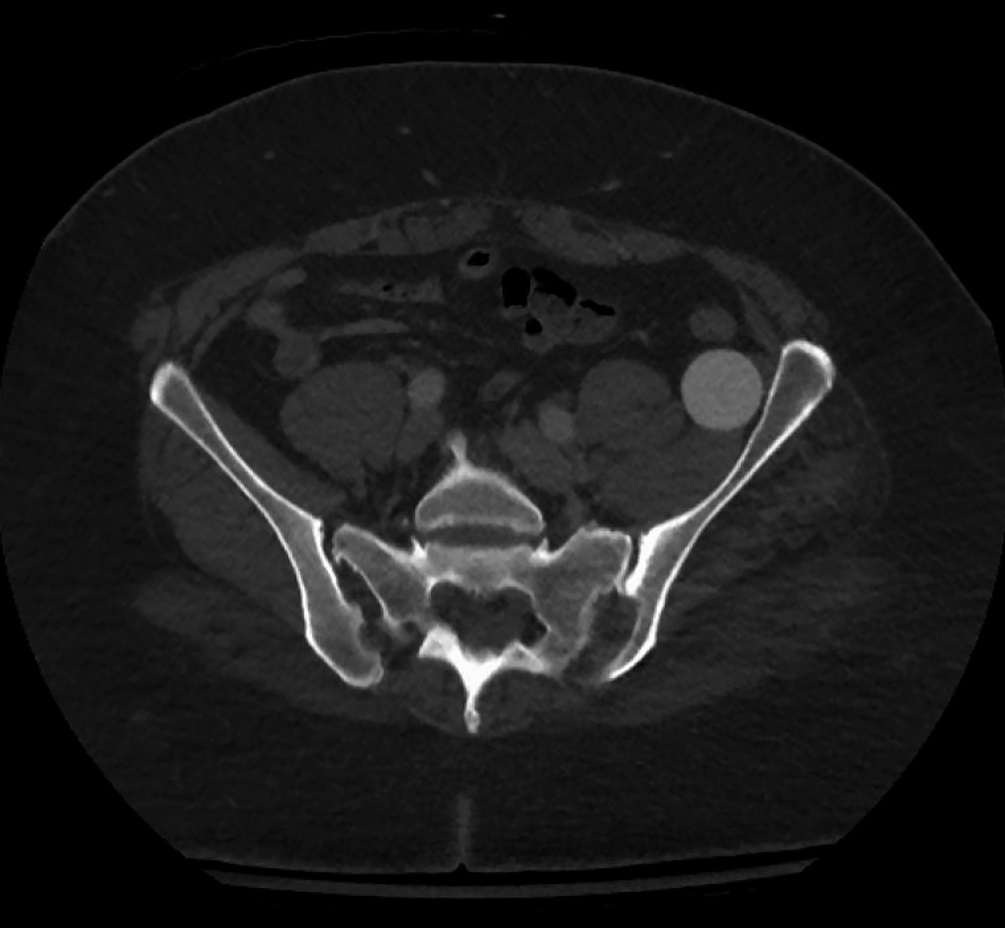
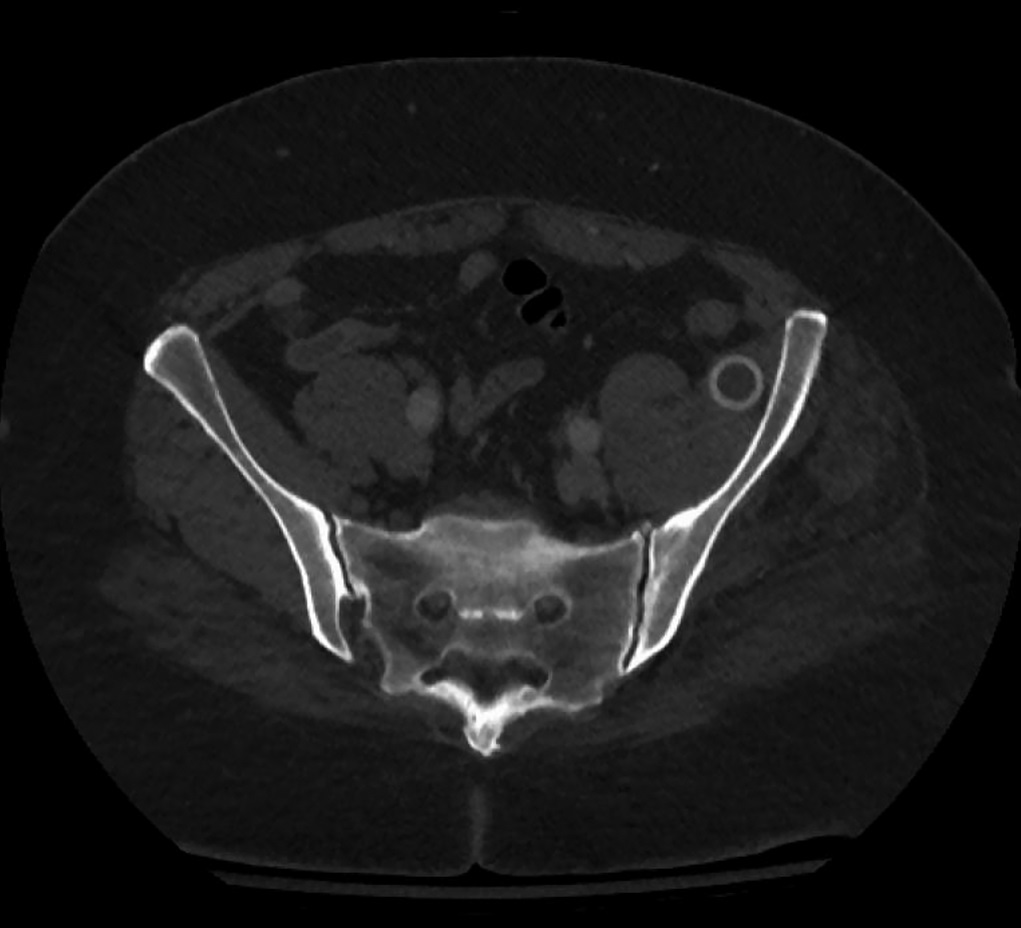
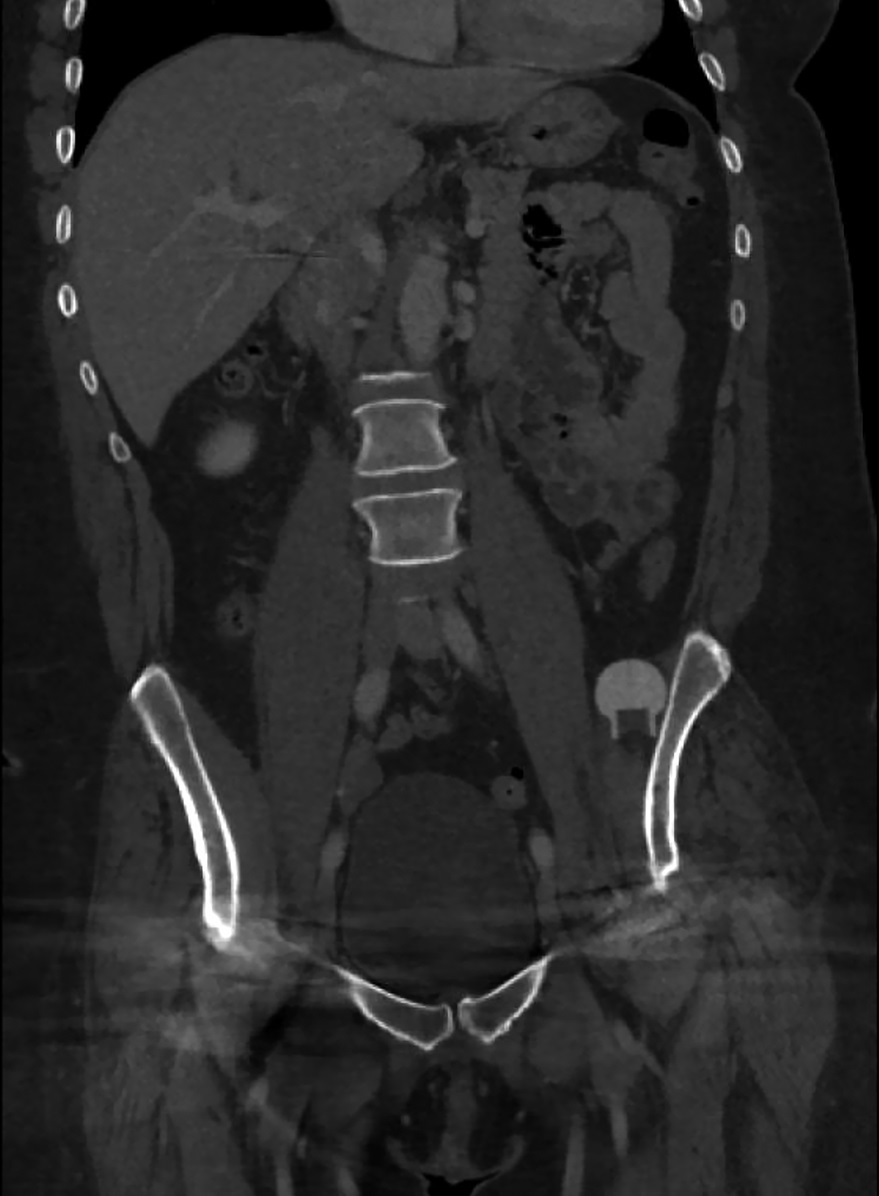
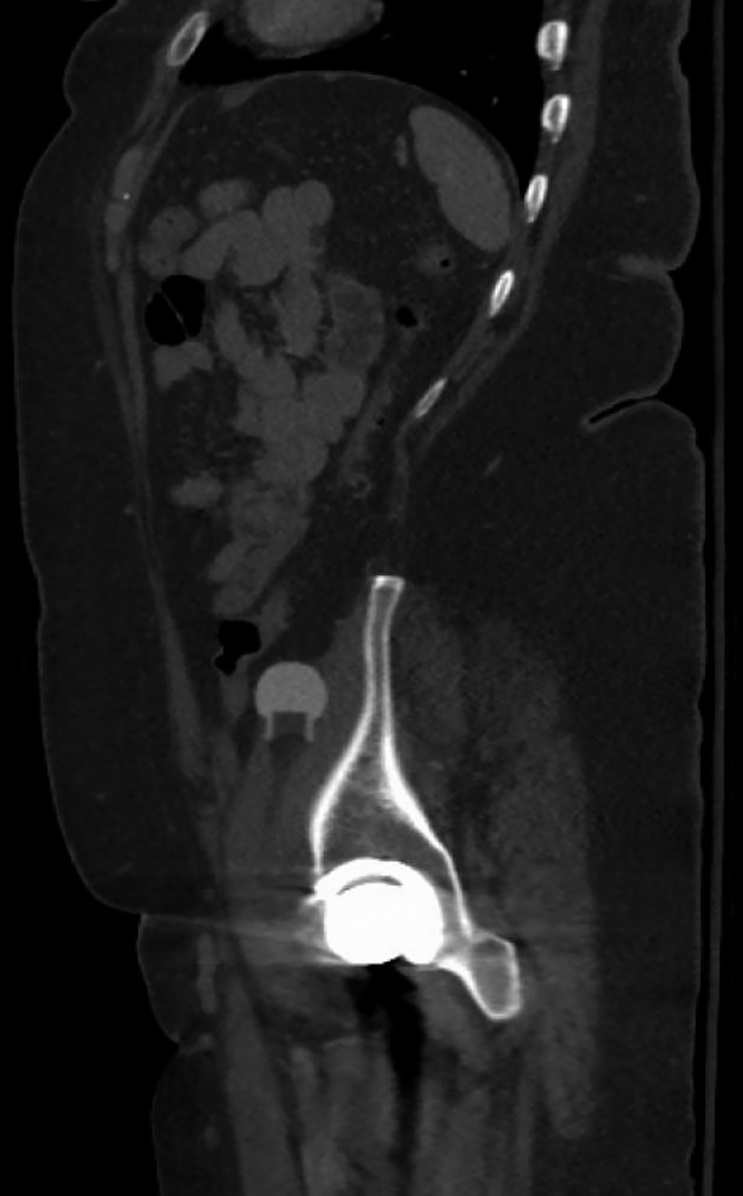
 Fig. 1
Fig. 1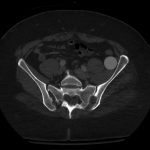 Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 2-C
Fig. 2-C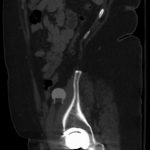 Fig. 2-D
Fig. 2-D