A 7-year-old girl was evaluated by her pediatrician for frontal headaches, dizziness, vomiting, and pulsatile tinnitus. The workup included computed tomography (CT) and magnetic resonance imaging (MRI) of the head, which demonstrated a 6 × 6.6 × 7.1-cm left frontal lobe mass. Further imaging was negative for additional visceral or osseous lesions. She was treated with total resection, adjuvant chemotherapy, and local radiation. Histology was consistent with a dural-based leiomyosarcoma.
The patient first presented to our orthopaedic oncology clinic at the age of 12 years with the chief symptom of atraumatic left hip pain of 1 year in duration, causing her to limp. The initial workup included whole-body bone scan, radiograph of the pelvis (Fig. 1-A), and MRI (Figs. 1-B and 1-C) of the left hip by which a lesion of the left posterior column and ischium was identified. A CT-guided needle biopsy was obtained, and the patient underwent arterial embolization of several branches of the left obturator artery. A follow-up MRI 1 month later demonstrated an increase in cystic formation and size of the lesion. The patient subsequently underwent percutaneous CT-guided chemical ablation with doxycycline with albumin twice within 2 months. Six weeks later, an MRI of the pelvis demonstrated a decrease in the cystic component of the lesion. She had temporary alleviation of her symptoms until presenting to the hospital 3 months later with atraumatic, acute-onset left hip pain and inability to bear weight. No pathologic fractures were noted on CT. She followed up at the orthopaedic oncology clinic, and surgical intervention was recommended. The patient underwent intralesional curettage and grafting with PRO-DENSE synthetic bone graft substitute for structural support through a posterior approach (Fig. 2). Histologic findings from the intraoperative biopsy are shown in Figure 3. Recommendations were made for 2 months of non-weight-bearing followed by surveillance imaging with CT to assess the structural integrity of the pelvis and with MRI to rule out recurrence, although these studies were not completed until 9 months postoperatively. Recommendations were then made for a repeat MRI 6 months later, after which she would undergo continued surveillance with serial radiographs. The patient began bearing full weight at 1 month postoperatively and returned to sports after 10 months. At 32 months postoperatively, she had no signs of recurrence.
The patient again presented to the orthopaedic oncology clinic at the age of 14 years with the chief symptom of left knee pain after a minor fall. Radiographs and MRI of the knee are shown in Figures 4-A through 4-D. Bone scan demonstrated increased uptake in the left proximal part of the tibia. The patient underwent intralesional curettage, grafting with Norian synthetic bone graft substitute, and prophylactic internal fixation (Figs. 5-A and 5-B). Histology from the intraoperative biopsy is shown in Figure 6. Recommendations were made for protected weight bearing with crutches and a knee immobilizer for 2 weeks, followed by gradual weaning from crutches and knee immobilizer. The patient returned to normal daily activities after 4 weeks, and physical therapy was initiated. She was instructed to refrain from athletic activity for another month. Surveillance imaging with serial radiographs was recommended. At 12 months postoperatively, she showed no signs of recurrence.
In the event that she developed pain at an additional site, the patient was instructed to return for clinical evaluation with radiographs and possibly MRI.
Imaging and histology of the first lesion were interpreted as a conventional aneurysmal bone cyst (ABC), and the second lesion was a solid variant of ABC. Therefore, the patient was considered to have had metachronous, polyostotic ABCs.
Proceed to Discussion >>Reference: Naylor WM, Collier CD, Redline RW, Getty PJ. Metachronous, polyostotic aneurysmal bone cysts in an adolescent female: a case report. JBJS Case Connect. 2019 Dec;9(4):e0263. Erratum in: JBJS Case Connect. 2019 Dec;9(4):e0263ER.
ABCs are benign lesions of bone that can be locally aggressive with an expansive and osteolytic radiographic appearance. They are usually located in the metaphysis of long bones (52%) with an incidence of 0.14 per 100,000. The female-to-male ratio is 1.16:1, with a peak incidence occurring during the second decade of life; however, they may present at any age. The term “aneurysmal bone cyst” was first coined in the literature by Jaffe and Lichtenstein in 1942 when presenting 2 cases of ABCs, one in the superior pubic ramus of a 17-year-old male patient and the other in the vertebral column of an 18-year-old male patient. Pain, swelling, and local tissue warmth are often the primary presenting symptoms. Because of their expansive and locally aggressive nature, ABCs may result in a mass effect on adjacent neurovascular structures depending on their location; 1 case of an ABC in the first rib that resulted in thoracic outlet syndrome has been published. Cottalorda et al. reported the most common location for ABCs to occur as the femur (22.3%), tibia (17.4%), spine (14.7%), humerus (10.5%), pelvis (8.8%), and fibula (8.3%), although other ranges of anatomic distribution have also been described. Recurrence rates after treatment are high in younger patients.
Previous theories regarding the etiology of ABCs include “improper repair of a traumatic subperiosteal hemorrhage, a vascular disturbance of the bone, or hemorrhage into a preexisting lesion”; however, cytogenic data have demonstrated multiple chromosomal translocations and the formation of fusion genes involving ubiquitin-specific peptidase 6 in ABCs, identifying a true neoplastic etiology. Aneurysmal changes in bone are distinct from ABCs and may occur secondary, or reactive, to other lesions such as giant cell tumor, chondroblastoma, chondromyxoid fibroma, nonossifying fibroma, osteoblastoma, fibrosarcoma, fibrous histiocytoma, osteosarcoma, and fibrous dysplasia. When the diagnosis is in doubt, biopsy should precede operative treatment to provide a definitive diagnosis and rule out malignancy, including telangiectatic osteosarcoma, which has many radiographic similarities with an ABC.
Although some ABCs have been reported to regress spontaneously, most cases require interventional management for symptomatic relief and to avoid progression, which may lead to pathologic fracture. Operative treatment of ABCs may involve aggressive curettage with some form of adjuvant treatment such as phenol, liquid nitrogen, high-speed burr, or argon beam coagulation. The use of a high-speed burr has been associated with a decreased rate of recurrence. The use of a high-speed burr in conjunction with argon beam coagulation has been shown to decrease the rate of recurrence from 20.6% to 7.5% when compared with the high-speed burr alone; however, this combination has also demonstrated a postoperative fracture rate of 12.5%. Depending on the anatomic location and size of the lesion, prophylactic internal fixation for added structural support may be considered to address this complication.
To our knowledge, there are only 5 published cases of metachronous, polyostotic ABCs in 4 male patients and 1 female patient. The longest documented interval between clinical presentation of the first and second lesions is 15 years, whereas the shortest interval is 3 months. The highest number of lesions reported in a single patient is 5. Cytogenetic analysis by Scheil-Bertram et al. did not yield chromosomal structural abnormalities as demonstrated in previous studies. None of the cases presented have demonstrated an association between metachronous, polyostotic ABCs and a previous history of malignancy.
ABCs are typically treated surgically. When open treatment would require a more extensile approach or if the lesion is inaccessible, less invasive options may be attempted such as selective arterial embolization or percutaneous sclerotherapy. Selective arterial embolization is used to disrupt the blood supply to the ABC, ideally resulting in ossification within 2 to 4 months. Potential complications include disruption of vascularity of adjacent tissues. In 2 separate retrospective studies, sclerotherapy with doxycycline has been shown to have a local recurrence rate of 5% at 24 months and 6% at 18 months. However, sclerotherapy also has the potential for complications including pulmonary embolism, skin necrosis, osteomyelitis, and hypopigmentation. Treatment with radiation therapy has also been described but is generally avoided, as it may lead to malignant transformation of ABCs.
The patient in this case underwent both selective arterial embolization and percutaneous sclerotherapy of her left periacetabular ABC. Recurrence of her symptoms led to the recommendation for intralesional curettage and bone grafting. Intraoperative biopsy showed findings consistent with the classic variant of ABC; however, the decision for surgery was made on the basis that regardless of whether the pain the patient was experiencing was secondary to an ABC or mechanical pain due to weakened bone, the treatment would be the same. Whether the ABC represents a recurrence or incomplete response to treatment is unknown.
It is well established that ABCs affect male and female patients. However, to our knowledge, there are only 5 published cases of metachronous, polyostotic ABCs, with only 1 case describing lesions in a female patient. This is the second case demonstrating that female patients may also develop polyostotic disease. None of the 5 previously reported patients with metachronous, polyostotic ABCs had a history of malignancy. Interestingly, the current patient did have a history of malignancy, and there was suspicion for metastasis both times that she presented with an osseous lesion. For this reason, diagnostic biopsy before intervention was indicated. When the diagnosis is uncertain, biopsy should precede definitive treatment, as in the case presented here.
Metachronous ABCs are rare and have been reported to present anywhere from 3 months to 15 years after diagnosis of the initial lesion. Therefore, whole-body imaging studies to rule out polyostotic lesions in the workup of a solitary ABC are unnecessary. If polyostotic disease is suspected on the basis of clinical presentation and history, additional imaging may be warranted. Patients with multiple ABCs should be managed by following the standard approach for treatment of each lesion and routine postoperative imaging surveillance to rule out recurrence.
Reference: Naylor WM, Collier CD, Redline RW, Getty PJ. Metachronous, polyostotic aneurysmal bone cysts in an adolescent female: a case report. JBJS Case Connect. 2019 Dec;9(4):e0263. Erratum in: JBJS Case Connect. 2019 Dec;9(4):e0263ER.
What is the diagnosis?
Metastatic leiomyosarcoma
Polyostotic fibrous dysplasia
McCune-Albright syndrome
Multifocal giant cell tumor of bone
Metachronous, polyostotic aneurysmal bone cysts



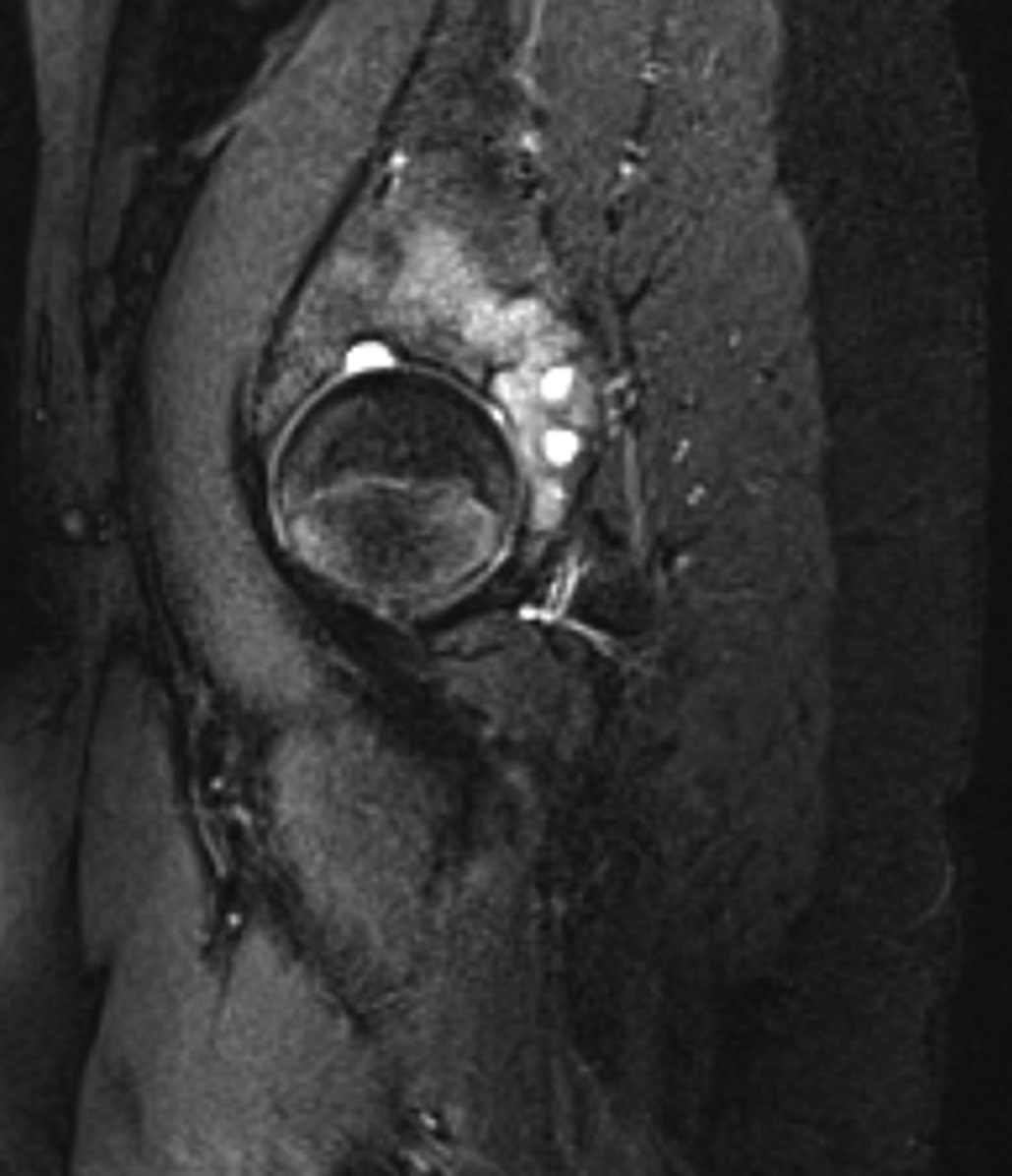
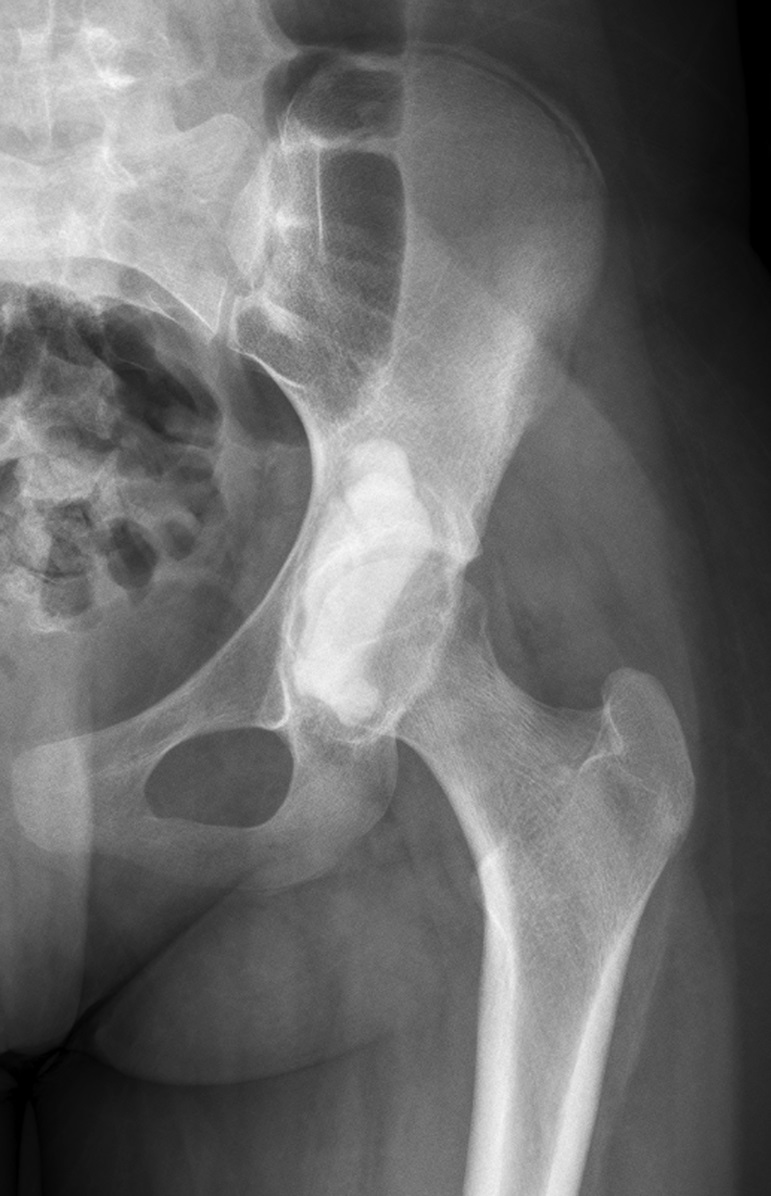
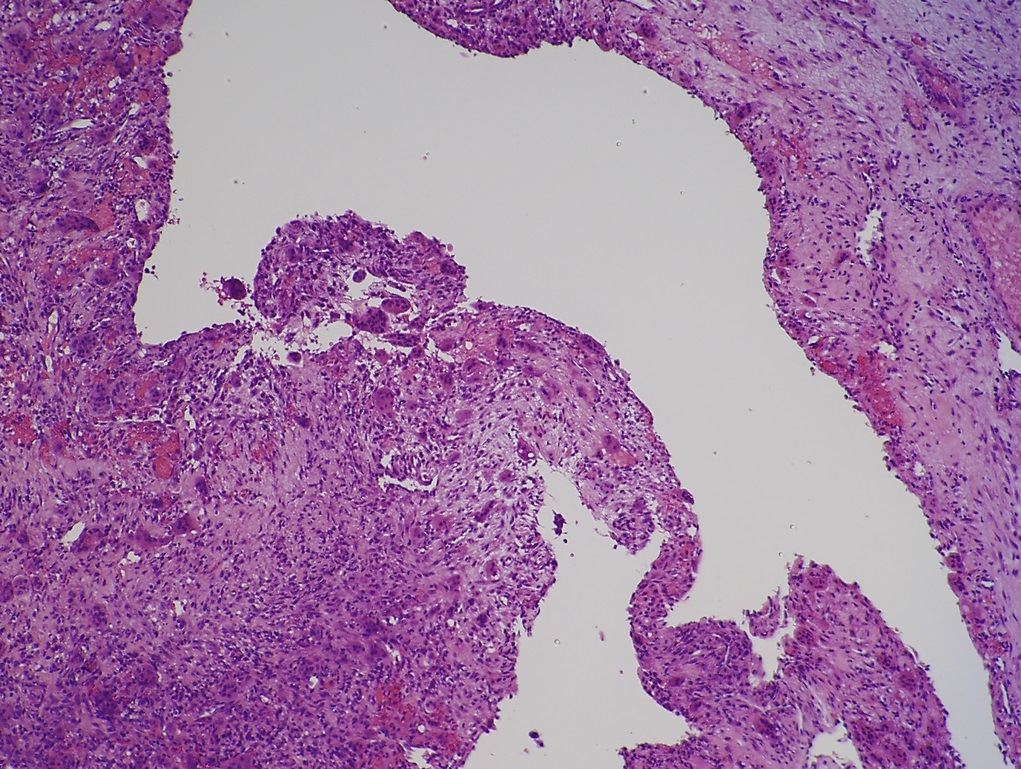


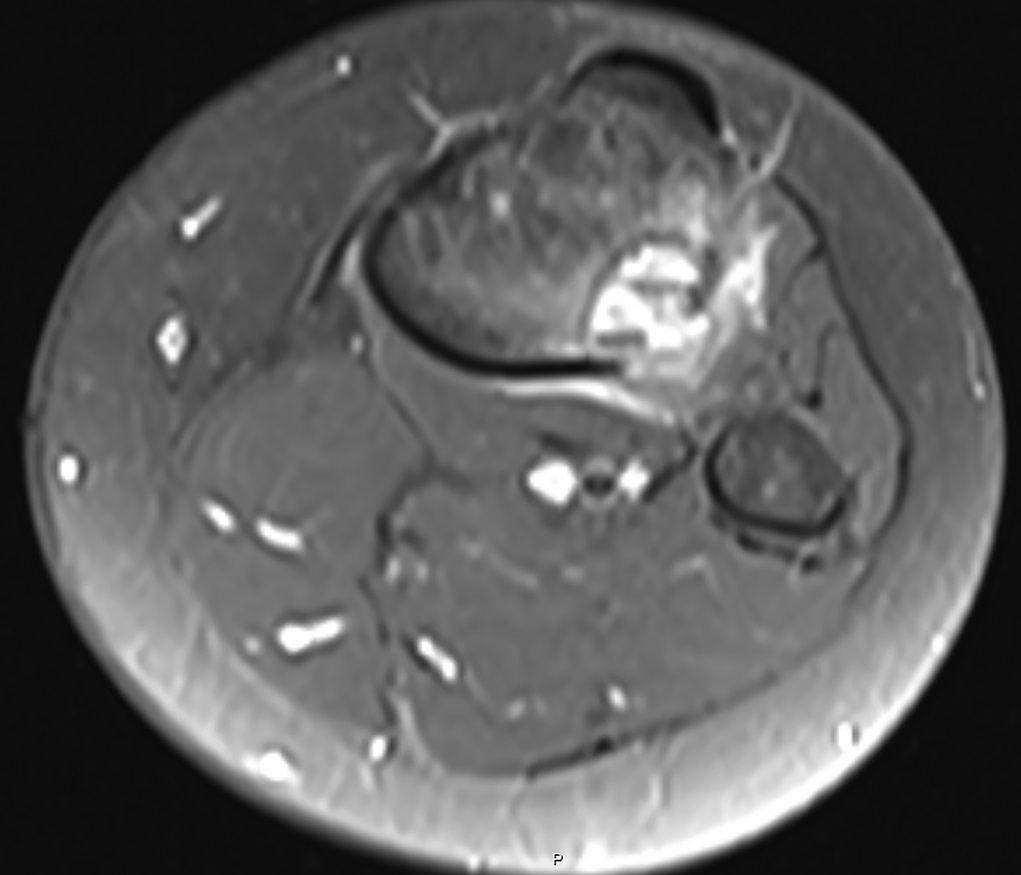
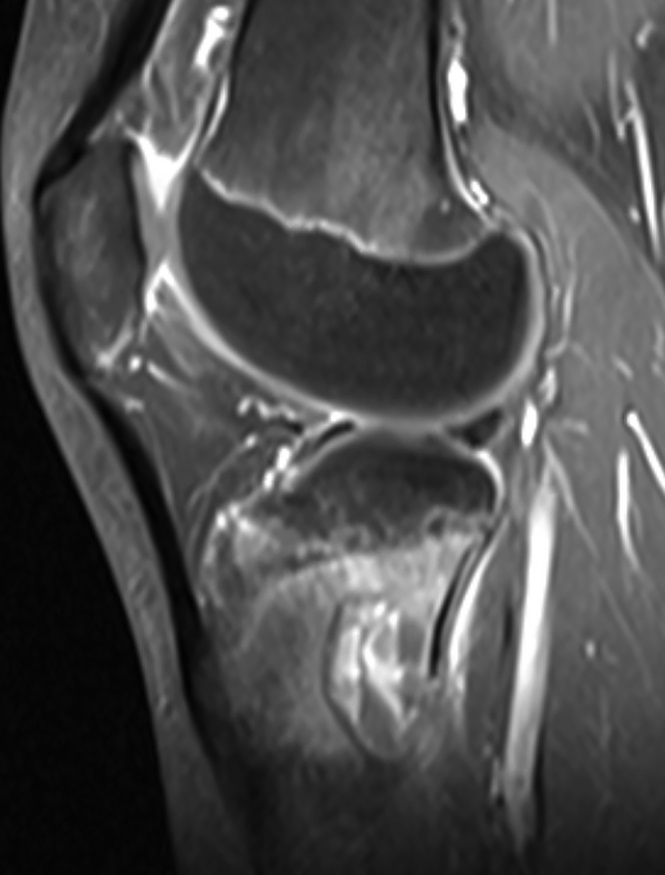
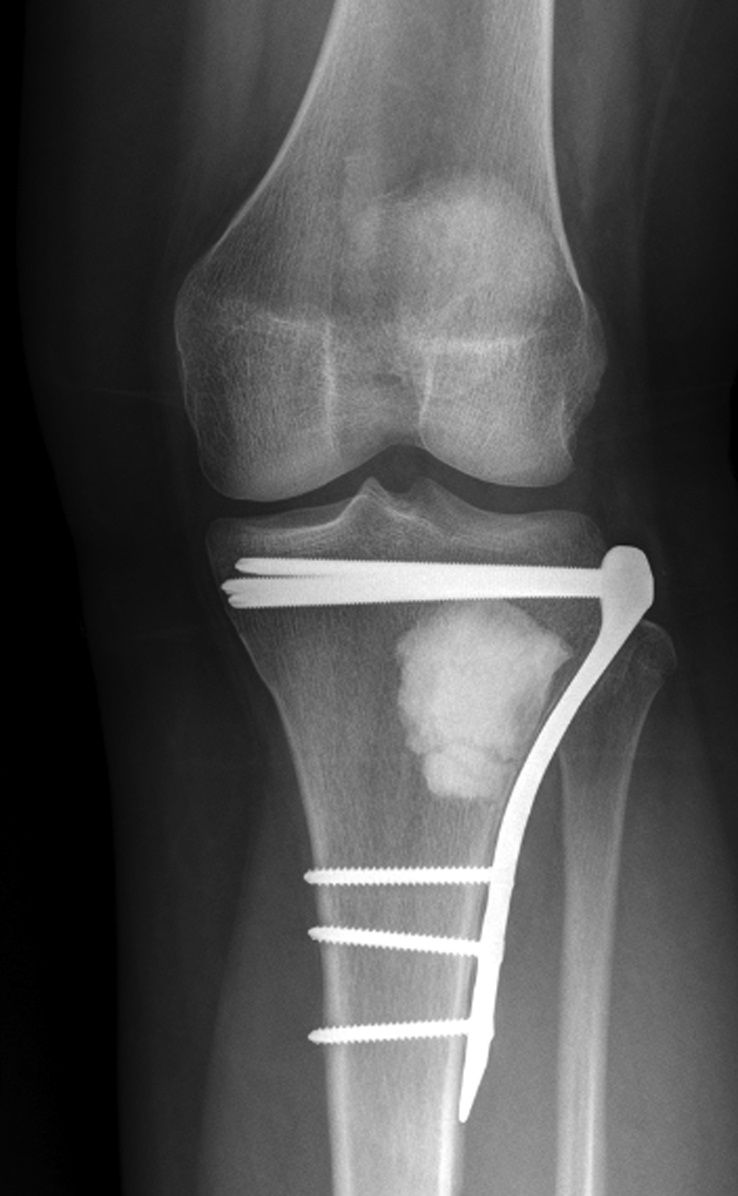

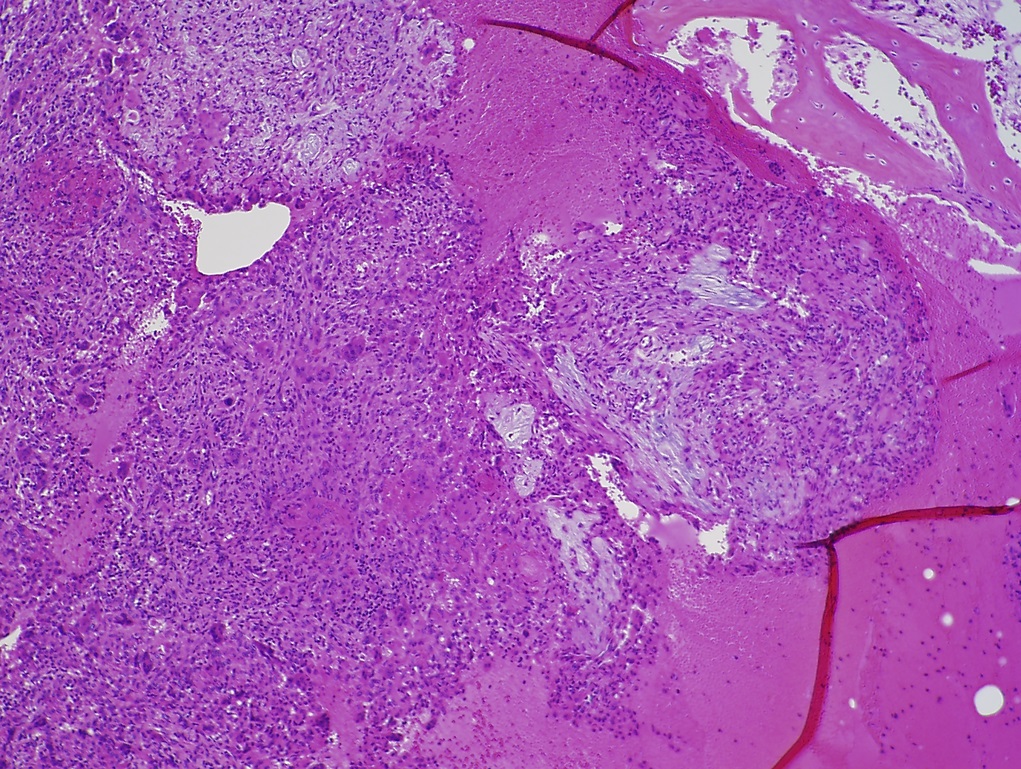
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 1-C
Fig. 1-C Fig. 2
Fig. 2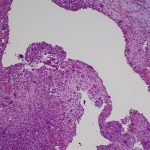 Fig. 3
Fig. 3 Fig. 4-A
Fig. 4-A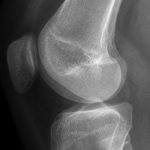 Fig. 4-B
Fig. 4-B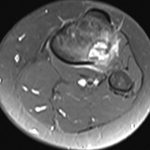 Fig. 4-C
Fig. 4-C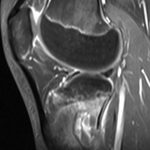 Fig. 4-D
Fig. 4-D Fig. 5-A
Fig. 5-A Fig. 5-B
Fig. 5-B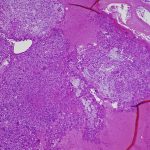 Fig. 6
Fig. 6