The patient was a 15-month-old twin boy being followed for developmental dysplasia of the hip in the setting of breech presentation. His parents noted that he had not yet started walking, whereas his twin brother had begun walking at 14 months of age. The patient’s parents additionally noticed that he avoided putting pressure on the left leg while attempting to walk. His physical examination demonstrated a well-appearing child with no neurologic deficits. On the evaluation of the hips, he had 80° of abduction, 70° of external rotation, and 40° of internal rotation bilaterally with negative Barlow, Ortolani, and Galeazzi signs.
Radiographs demonstrated a radiolucent lesion in the left femoral neck surrounded by scalloping and destruction of the medial femoral neck (Figs. 1 and 2). The patient’s acetabular index was 28° on the left and 30° on the right. Magnetic resonance imaging (MRI) scans were acquired, demonstrating an eccentric, cortical-based lesion at the medial anterior femoral neck with a sclerotic border, in addition to a focal area of anterior cortical breakthrough with a small soft-tissue component (Figs. 3 and 4). There was mild periostitis but no notable perilesional marrow edema, and the lesion did not involve the proximal femoral physis.
A computed tomography (CT)-guided biopsy (Fig. 5) and histological assessment (Figs. 6 and 7) were then performed.
With the combination of radiographic and histologic findings, the patient was diagnosed with infantile myofibroma. Given the patient’s clinical and radiographic findings, namely the gross motor development delays with the inability to ambulate compared with his twin brother, prophylactic fixation was then recommended to stabilize the proximal femur. The patient’s family thus consented to proximal femoral fixation.
In the operating room, fluoroscopic guidance was used to mark the incision along the lateral aspect of the hip starting at the apophysis of the greater trochanter and extending 5 cm distally. Dissection was performed to the level of the iliotibial band, which was bluntly freed of soft-tissue adhesions and then incised longitudinally, revealing the vastus lateralis. An L-shaped incision was made along the posterolateral border of the vastus fascia and vastus ridge. Subperiosteal dissection was performed to expose the proximal femur. After trialing plate options under fluoroscopy, the 2.7-mm 130° pediatric proximal femoral plate was found to fit best. This was contoured on the back table to sit properly on the lateral aspect of the proximal femur. Under fluoroscopic guidance, the plate was positioned on the proximal femur, and a 2.0-mm guidewire was placed centrally in the femoral neck and aimed proximally to avoid the lesion. The final guidewire position was just proximal to the lesion and short of the physis. Two additional wires were placed proximally and distally to hold the plate in appropriate alignment. The guidewire was measured and replaced with an appropriately sized locking screw. Two cortical screws were then placed in the shaft to compress the plate to the bone. A second proximal locking screw was placed unicortically outside the lesion to add additional stability. All remaining guidewires were removed, and final fluoroscopic images were obtained. The wound was then irrigated and closed in a standard layered fashion, and an abduction pillow was used for comfort postoperatively.
The patient recovered uneventfully postoperatively and was discharged home the same day. He was allowed to bear weight as tolerated on the left lower extremity and was discharged with appropriate pain medications. At his first 2-week postoperative visit, his radiographs demonstrated well-positioned implants (Fig. 8), and his parents noted improvement in the supported gait pattern while pushing toys and his walker. The patient began walking independently shortly thereafter. At the patient’s 1-year postoperative follow-up, radiographs showed evidence of healing and improvement of his acetabular indices to 20° bilaterally, consistent with improving dysplasia (Figs. 9 and 10). At that follow-up, the patient was able to run and jump with no limp, consistent with the activity level of his twin brother. In addition, he had a full symmetric range of motion of the hips with negative Barlow, Ortolani, and Galeazzi signs. At the latest follow-up, it was planned for the patient to undergo implant removal.
Proceed to Discussion >>Reference: Gunderson A, Abraham VM, Li AD, Lorimer SD, Rocchi V. Infantile myofibromatosis of the femoral neck: a case report. JBJS Case Connect. 2024 Feb 16;14(1).e23.00478.
Solitary infantile myofibromas are rare, with only a few case reports detailing its occurrence in bone and even fewer reports detailing the surgical management. This report details a novel case of infantile myofibroma of the proximal femur causing gross motor developmental delays and the surgical method used for prophylactic fixation resulting in the resolution of the motor delays.
Infantile myofibroma is a fibrous lesion most commonly found on the skin or in visceral organs, subcutaneous tissues, or bone. The etiology of this lesion is not well understood, and previous case reports have described the solitary type of infantile myofibroma in the diaphysis of the femur, distal ulna, humeral shaft, and distal tibia. As far as we know, this case report is the first to describe infantile myofibroma occurring in the femoral neck causing gross motor developmental delays.
The solitary form of infantile myofibroma typically regresses spontaneously within the first 2 years. However, when nonoperative management fails, surgical intervention is indicated to stabilize these bony lesions. In the presented case, surgical stabilization was especially important, given the gross motor developmental delays in the patient compared with his twin brother.
Previously described surgical interventions include curettage alone and curettage and stabilization with implants. In the presented case, the treatment team believed that curettage alone was not a feasible treatment option, given the risk of collapse of the femoral neck with no stabilization. Thus, the goal of treatment was to stabilize the femoral neck to allow for weight-bearing. Although there are different implant options available, the team believed that a proximal femoral locking plate would provide enough support to the femoral neck for load-bearing, thus allowing the patient to bear weight on the involved extremity in the postoperative period.
Overall, the prognosis of solitary infantile myofibroma of the bone is favorable. One case series demonstrated no recurrence of the lesion after operative intervention in 6 cases. However, there has been a report of recurrence in the ulna after operative management with curettage. In the presented study, no evidence of recurrence was present in the 1-year postoperative period.
Reference: Gunderson A, Abraham VM, Li AD, Lorimer SD, Rocchi V. Infantile myofibromatosis of the femoral neck: a case report. JBJS Case Connect. 2024 Feb 16;14(1).e23.00478.
What is the diagnosis?
Fibrous dysplasia
Osteofibrous dysplasia
Adamantinoma
Infantile myofibroma
Non-ossifying fibroma

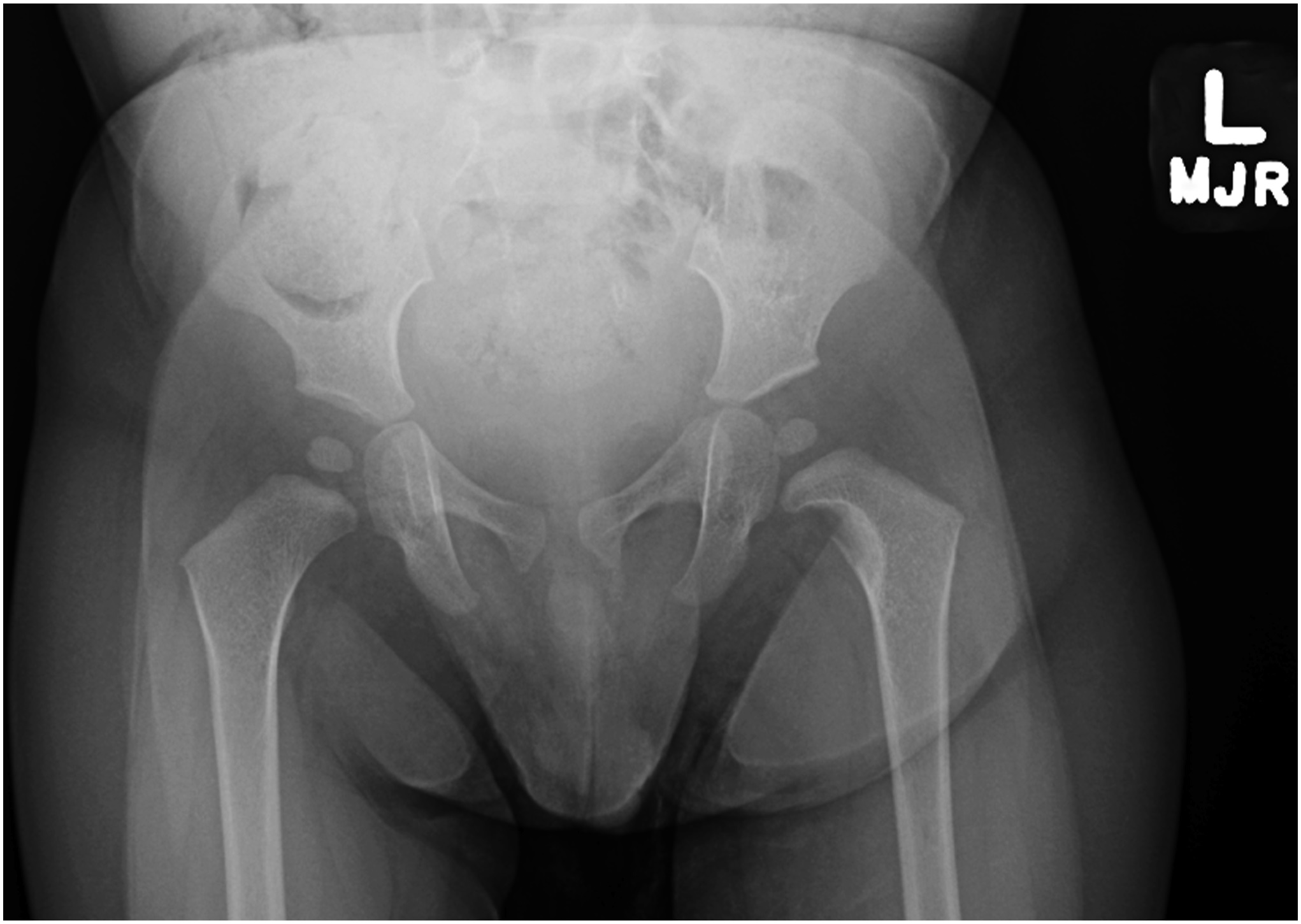

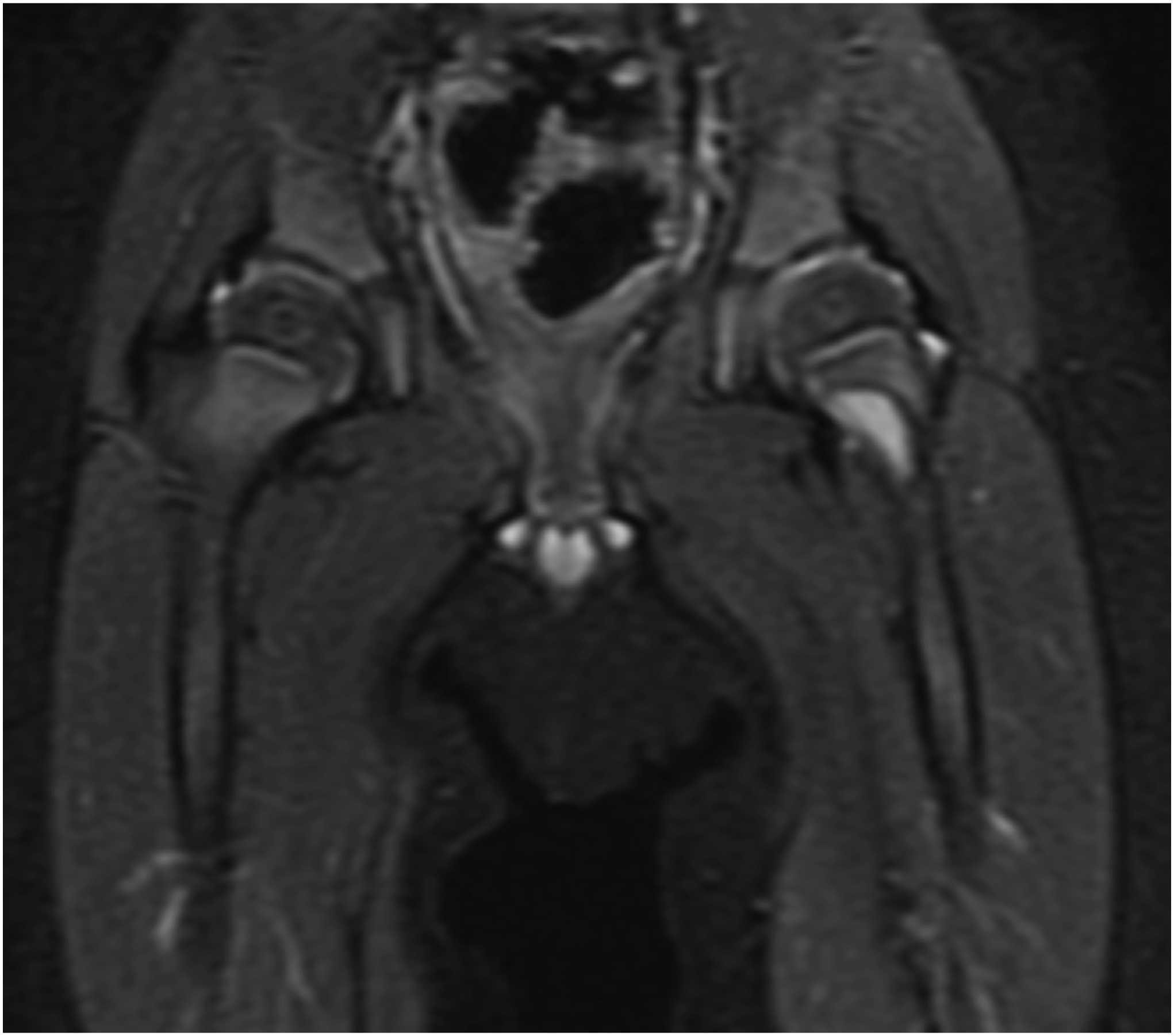
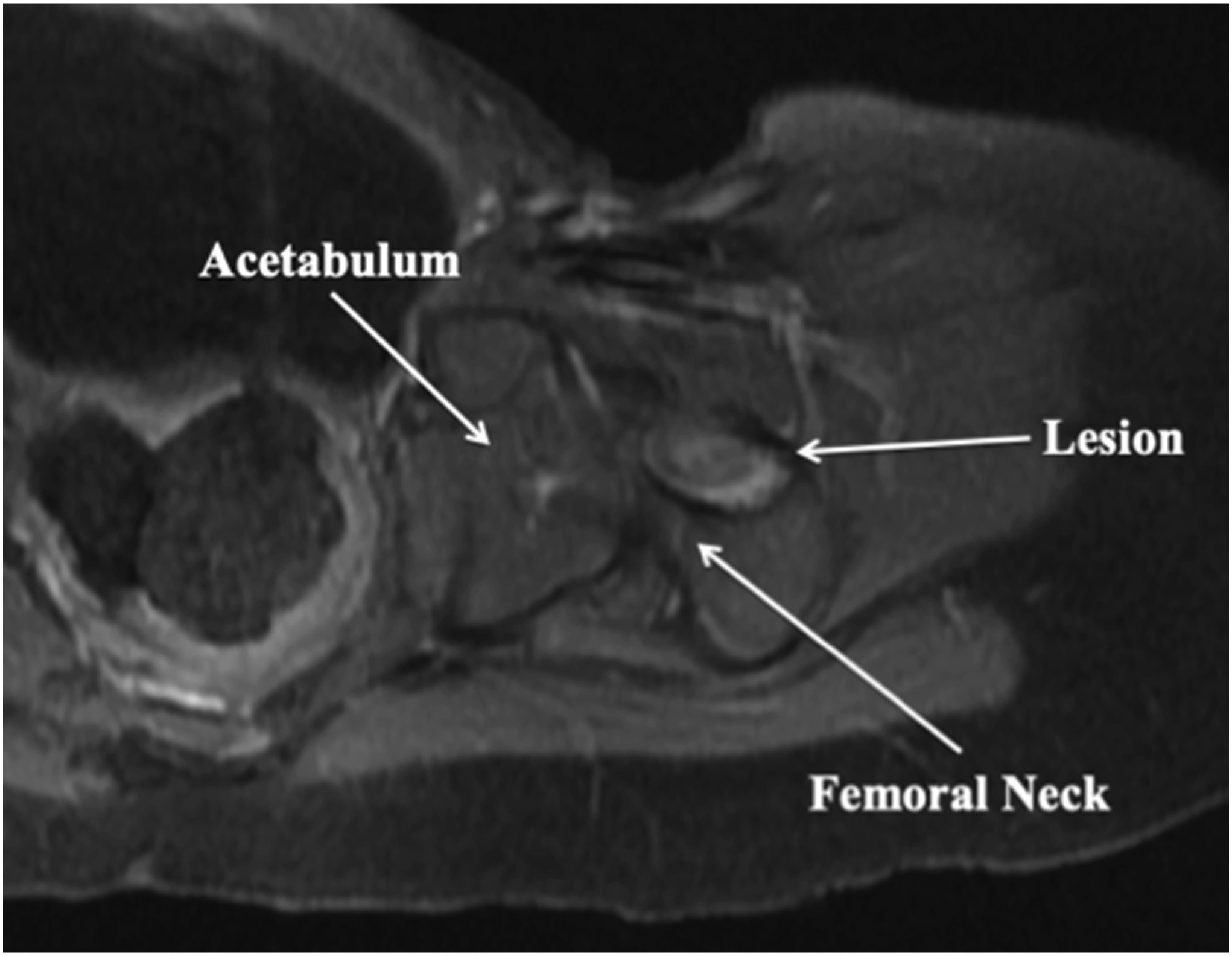
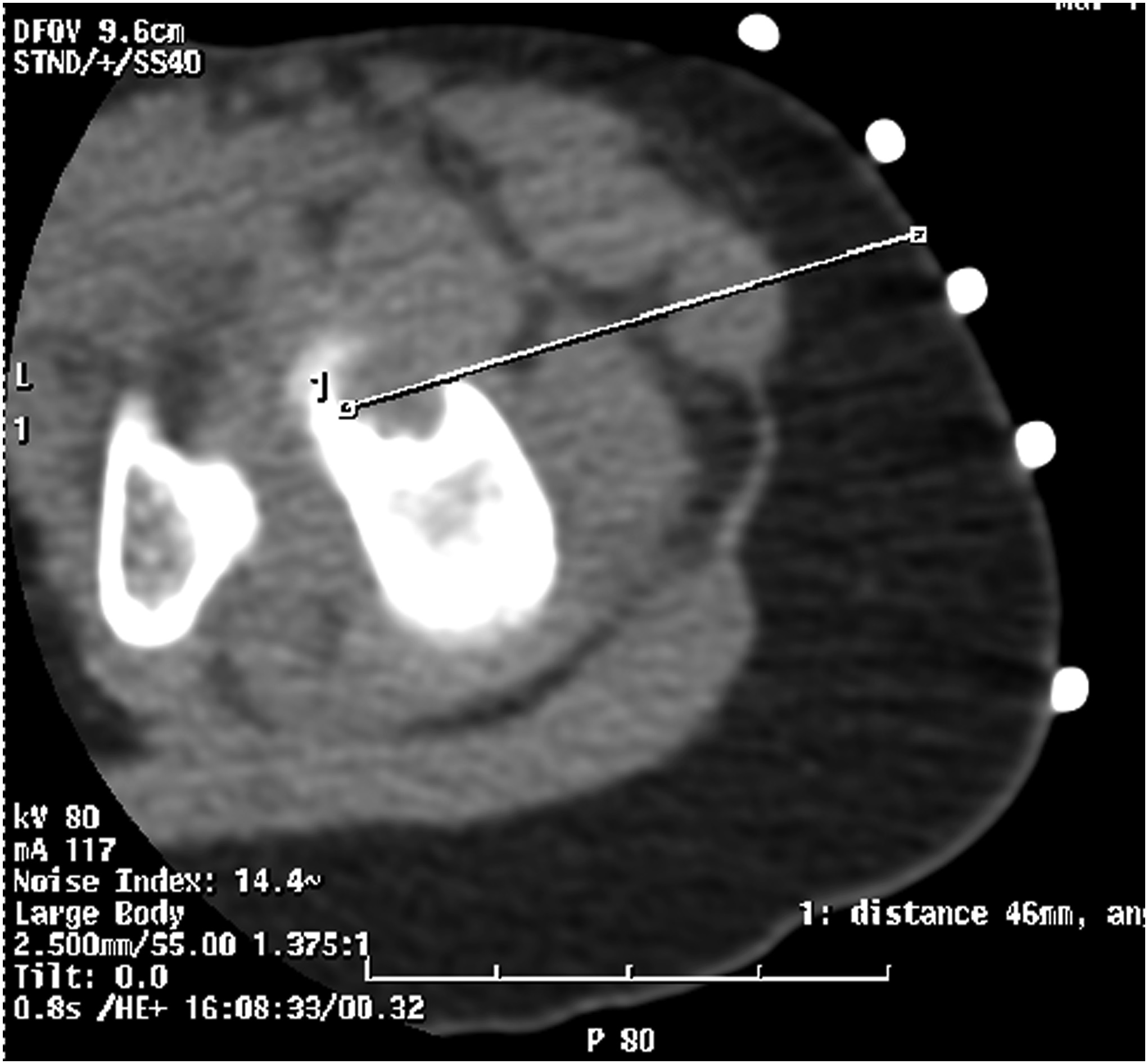
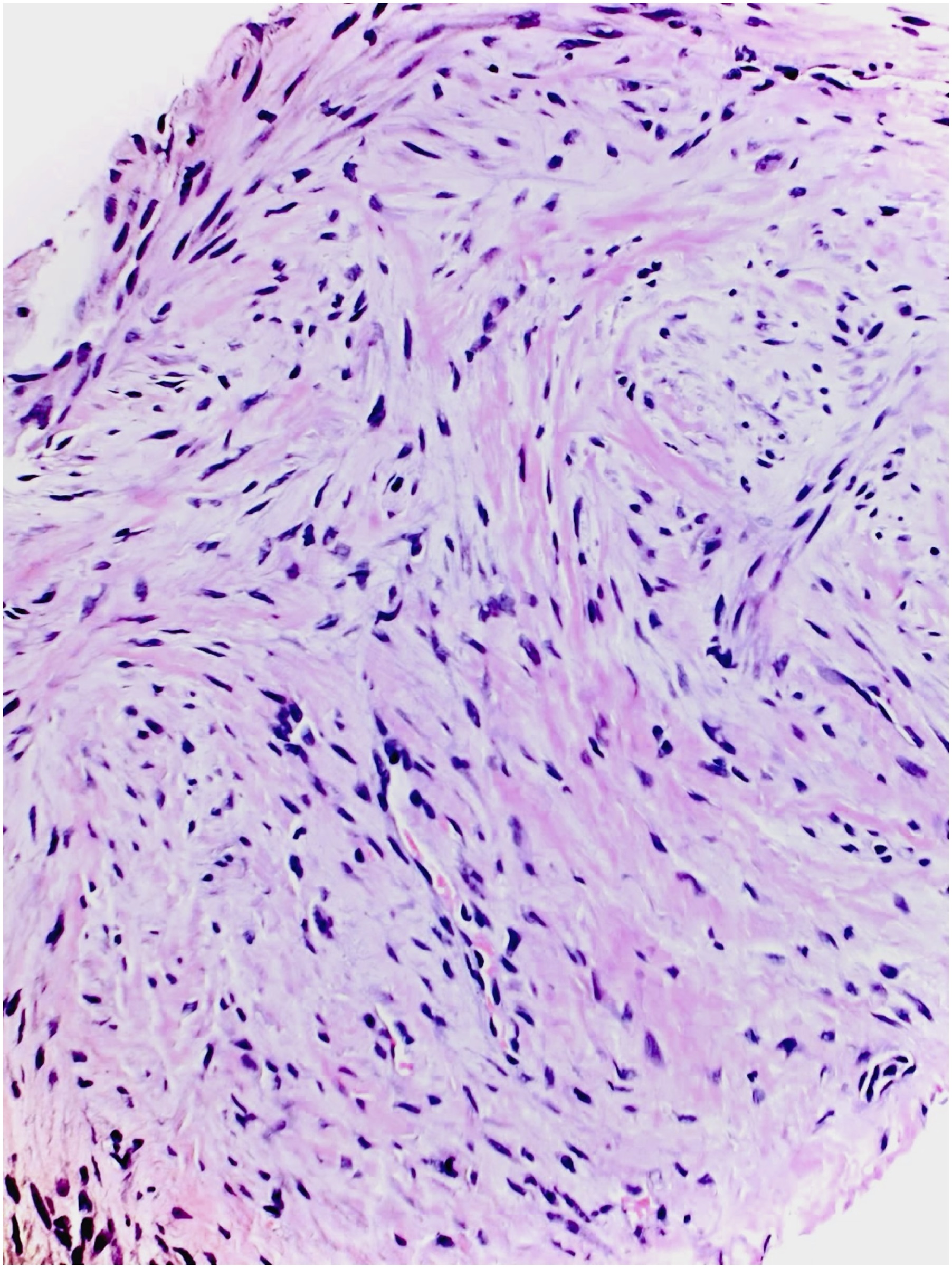
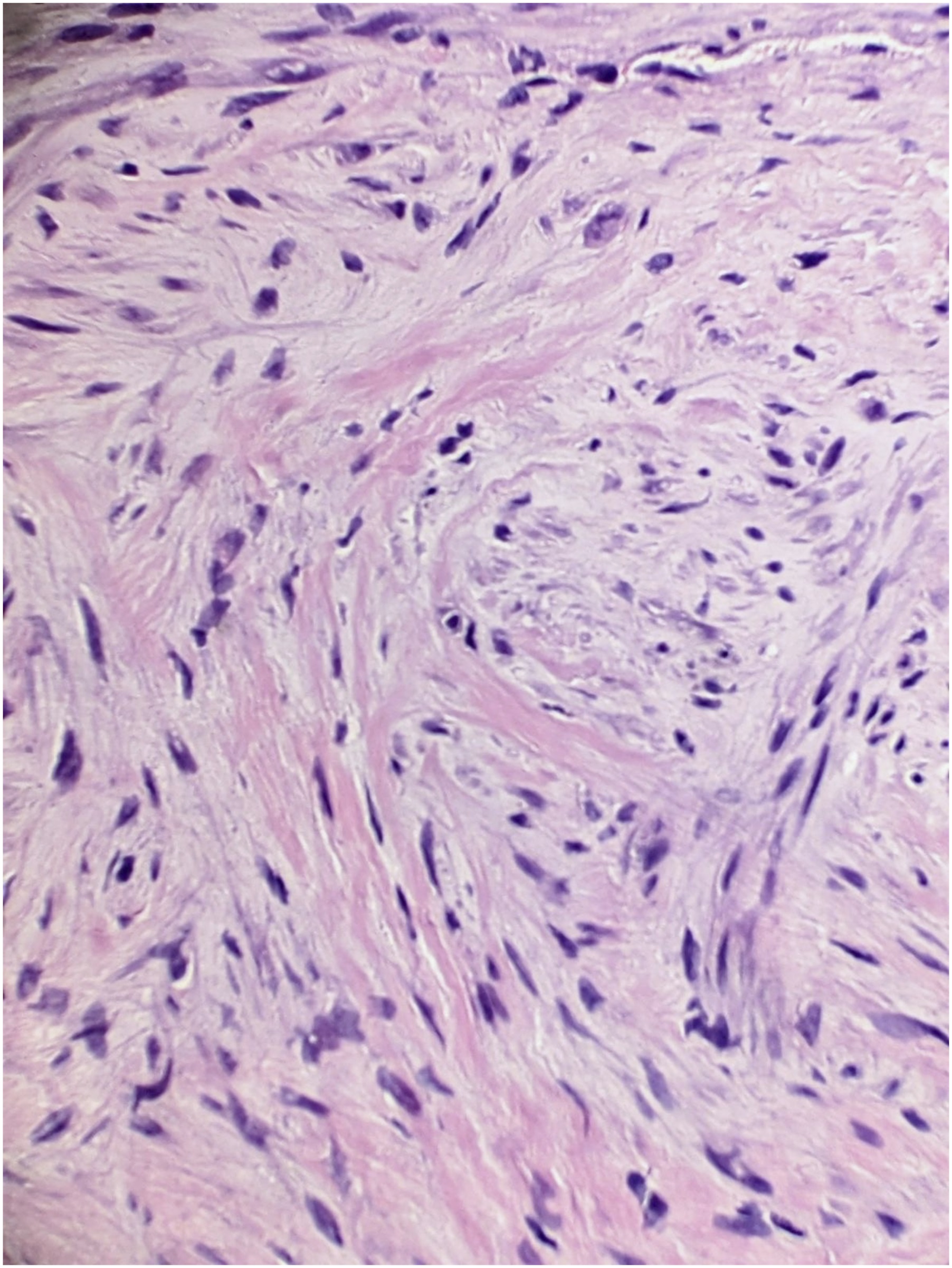
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3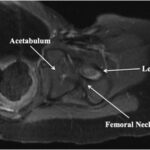 Fig. 4
Fig. 4 Fig. 5
Fig. 5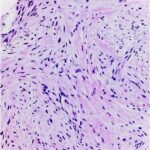 Fig. 6
Fig. 6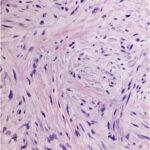 Fig. 7
Fig. 7 Fig. 8
Fig. 8 Fig. 9
Fig. 9 Fig. 10
Fig. 10

