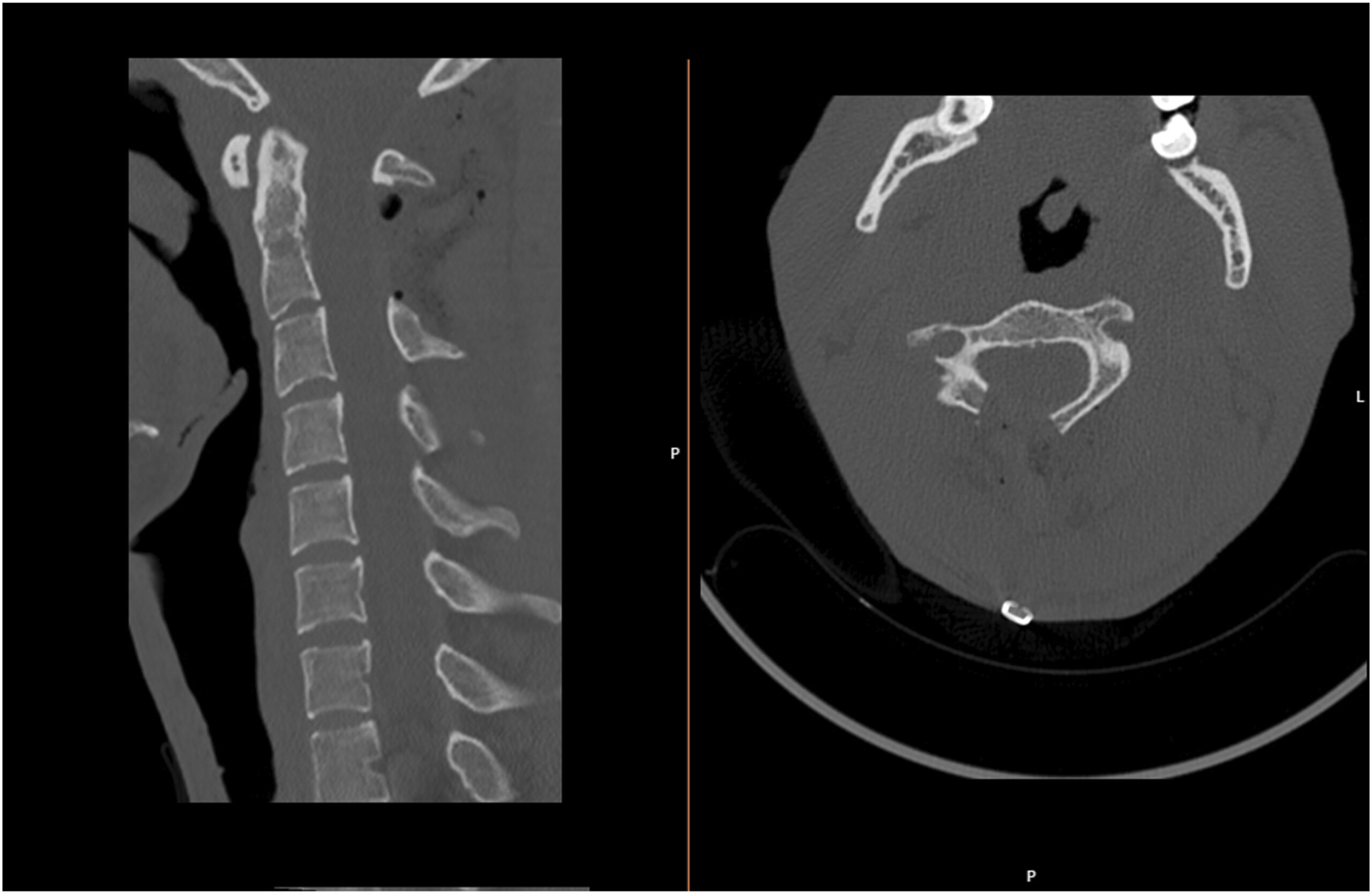
A 19-year-old man presented with cervical axial pain. His medical history included exostoses of both femora. At the neurological examination, he showed no muscle weakness, paresthesia, or sensory deficits. His reflexes were normal, and no clinical signs of myelopathy were present. The cervical spine radiograph was normal, but the computed tomographic (CT) scan presented a pedunculated bony lesion of 15 × 11 mm originating from the right C2 lamina, occupying approximately 40% of the medullary canal. The magnetic resonance imaging (MRI) scan revealed a heterogeneous expansive lesion with a hypersignal in T2-weighted images with a hyposignal halo in T1-weighted and T2-weighted images. This lesion pushed the spinal cord, which presented a thin hypersignal in T2-weighted and STIR-weighted images (Fig. 1). After discussion with the patient, a decision was made to excise the lesion.
The surgical intervention consisted of a posterior median approach with a right hemilaminectomy with an en bloc excision of the lesion. A subperiosteal dissection was made until the spinous processes of the C2 and C3 vertebrae were exposed. Using an ultrasonic burr, a C2 laminotomy was performed and dorsal traction was applied to the lamina. The lesion was carefully dissected from the ligamentum flavum to enable a safe excision. A right laminectomy and a ligamentum flavum exertion were performed with a Kerrison punch, resulting in a wide medullary decompression. The monitoring of motor and somatosensory-evoked potentials and a microscope were used.
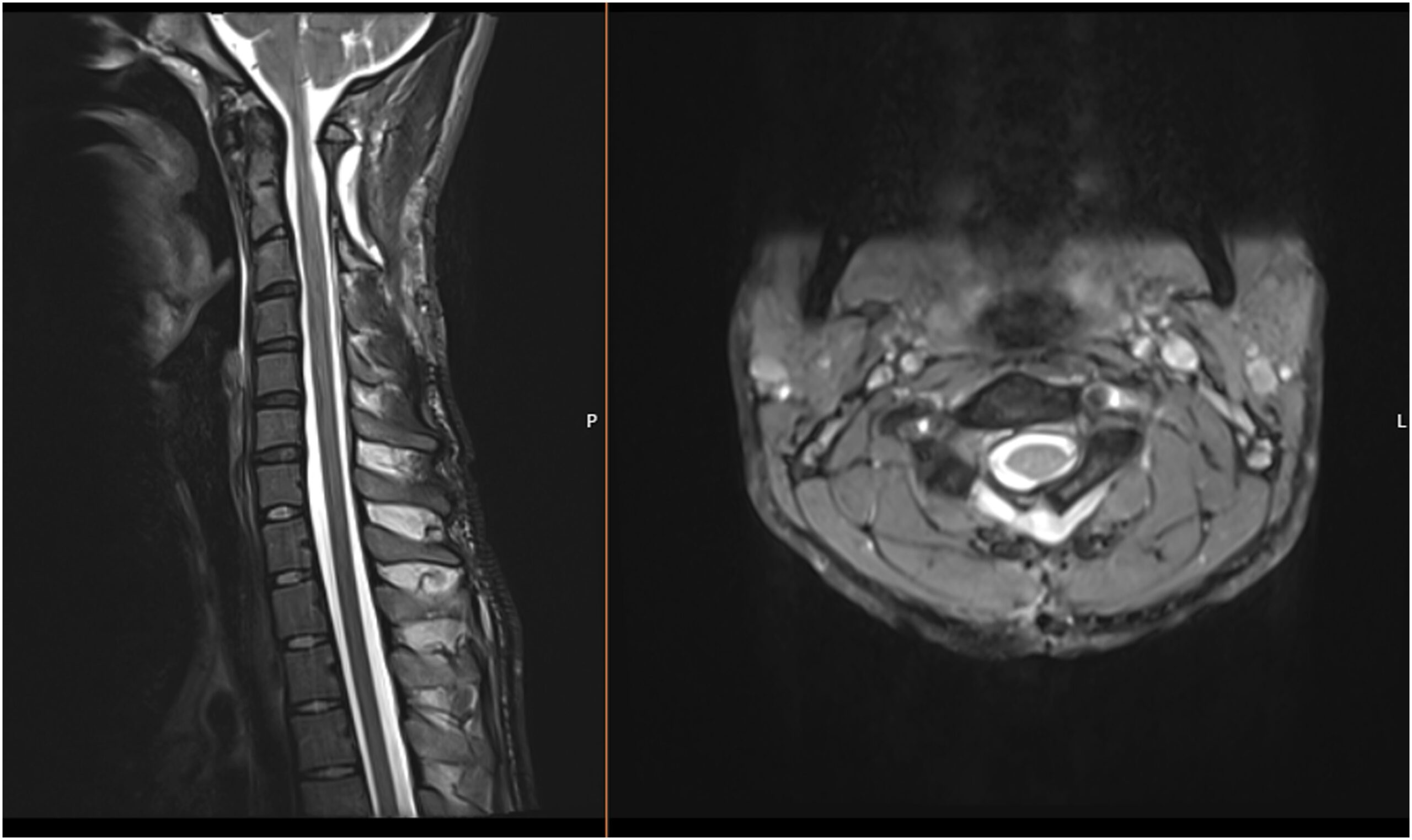
The patient had no complications in the postoperative period, and he was discharged home with a protective soft neck collar on postoperative day 4. The histology of the lesion is shown in Figure 2.
The combination of imaging and histologic findings is diagnostic of a benign osteochondroma. With additional similar lesions involving multiple other sites, the patient was diagnosed as having osteochondroma (multiple hereditary osteochondromas [exostoses], formerly known as multiple hereditary exostoses, a term that the authors used throughout this report).
At the 1-year follow-up, the patient presented with resolved cervical pain and hypesthesia, with a normal neurological examination. He had resumed his normal activities without limitations. There were no signs of disease recurrence on postoperative imaging (Figs. 3 and 4). C2-C7 lordosis remained identical in the postoperative radiograph (11.5° preoperatively compared with 12° postoperatively), and there was a slight loss of segmental C2-C3 lordosis, from 6.6° preoperatively to 2.3° postoperatively. There were no signs of instability in the dynamic images.
Proceed to Discussion >>Reference: Lixa J, Pinho A, Vieira P, Vieira da Silva N, Silva MR, Marques A, Veludo V. Medullary compression by a cervical osteochondroma in a patient with multiple hereditary exostoses: a case report. JBJS Case Connect. 2024 Jan 11;14(1):e23.00429.
The incidence of multiple hereditary osteochondromas is estimated to be 1:50,000 persons, but solitary osteochondroma is expected to be 6 times more frequent. The incidence seems to be higher in male patients (1.5:1), probably due to a milder phenotype in female patients. The syndrome is caused by mutations in the EXT1 and EXT2 genes that are responsible for the production of exostosin-1 and exostosin-2, both involved in the processing of heparin sulfate, although it is not understood how the lack of that protein is linked to osteochondroma development. Multiple hereditary exostoses and solitary osteochondromas are histologically indistinguishable. The diagnosis can be made clinically and by radiographic imaging, and it can be confirmed using genetic testing. The mean age at diagnosis is 30 years, usually earlier in cases of multiple hereditary exostoses. This patient presented with a high clinical suspicion for osteochondroma as a cause of cervical pain because of his positive history of multiple hereditary exostoses.
Most spinal osteochondromas (50% to 58%) are found in the cervical spine, and C2 is usually the most affected level, probably due to the higher mobility of the upper cervical segment. However, Fowler et al. found in a meta-analysis that, in cases of solitary exostosis, the most common level was C5. Solitary exostoses usually arise in the posterior arch as the spinous processes or lamina where ossification centers are located. This location is typically asymptomatic because solitary exostoses grow outward from the spinal canal. However, in the case reported, the lesion originated in the anterior part of the C2 lamina, growing inward into the medullary canal. In cases of compression of the neurological structures, symptoms such as cervical myelopathy, radiculopathy, irradiating pain, and sensitivity alterations can occur, with an incidence of 0.5% to 1%. Imaging studies involve CT scans to identify the bony lesions. The typical finding is a lesion with direct continuity with the cortex and medullary cavity of the underlying bone. MRI scans are used to exclude neurological compression or involvement of the surrounding tissues and usually show a hypointense cartilaginous cap in T1-weighted images.
Surgical treatment is reserved for symptomatic lesions or osteochondromas with potential neurological compression. Although neurological symptoms were absent, the lesion presented showed clear invasion of the medullary canal and medullary hypersignal on MRI scans. Given the age of the patient, lesion growth was unlikely, but the risk of eventual neurological deterioration was likely, whether because of cervical spondylosis from the aging process or by a cervical or head trauma, which may provoke a central cord syndrome or even tetraplegia.
Treatment consists of an en bloc resection with complete excision of the cartilage cap to prevent recurrence. Incomplete resection such as intralesional excision of the exostoses is associated with a high recurrence rate. Given the posterior location usually found, laminectomy is generally performed with or without fusion. In a meta-analysis by Fowler et al., in 67% of >200 cases, the patients were submitted to surgical decompression without fusion. Although specific studies for fusion after laminectomy for osteochondroma have been lacking, the role of cervical fusion after single-level laminectomy has not been clearly defined in the literature for other causes such as cervical myelopathy. Preoperative cervical spine alignment, the amount of facet joint resection, and the ligament laxity should be considered. Instability and kyphosis after laminectomy can be attributed to several factors, such as the loss of the posterior tension band and damage to the posterior cervical musculature. Although the short-term outcomes for laminectomy with or without fusion appear similar, the incidence of late deterioration is reduced with associated fusion, especially in the presence of neck instability, axial pain, or loss of cervical lordosis. Symptomatic and progressive kyphosis risk after laminectomy is higher in younger patients, more frequently requiring deformity correction surgery. Atlantoaxial fusion is a complicated procedure, associated with more morbidity, and may sacrifice the craniocervical junction if the fusion needs to be extended cranially to ensure a more secure fixation and a larger area to which to graft bone. In cases in which the tumor originates from the facet joint, fusion should be considered as the potential for instability after resection is greater.
In our case, a right hemilaminectomy was performed with complete excision of the lesion. Spinal fusion was not performed, as it was estimated that cervical spine stability was maintained because the articular facets were left intact, as only a hemilaminectomy was performed, with preservation of the musculoligamentous attachments conserving the posterior tension band. In addition, fusion was not performed to avoid the morbidity of a reduced craniocervical range of motion. At 1 year after the surgical treatment, the patient experienced pain relief and had no signs or symptoms of instability.
Recurrences are rare, with studies showing a recurrence rate of 2% to 4% in spinal osteochondromas. The mean interval of the recurrence reported was 4.2 years, suggesting that the follow-up period for these patients should be longer than 5 years.
A long clinical follow-up in this case is also mandatory to exclude the signs of cervical instability such as progressive kyphosis, neurological symptoms, and disease recurrence.
The worst complication of this lesion is the development of secondary chondrosarcoma by transformation of the cartilage cap. The estimated risk is approximately 1% in solitary osteochondromas and 10% of multiple hereditary exostoses cases. Signs such as tumor growth after skeletal maturity, irregular margins, or cartilage cap thickness >3 cm raise the concern of malignant transformation. In this case, the relatively thin cartilage cap and skeletal maturity favored a lower risk of malignant transformation. The spinal osteochondroma was completely excised, so we do not anticipate local recurrence.
In conclusion, cervical osteochondroma is a rare benign tumor that is usually asymptomatic. The risk of neurological compression and differentiation to chondrosarcoma are the main concerns relating to this lesion. Surgical en bloc excision allows the local cure of the disease and is usually performed without fusion.
Reference: Lixa J, Pinho A, Vieira P, Vieira da Silva N, Silva MR, Marques A, Veludo V. Medullary compression by a cervical osteochondroma in a patient with multiple hereditary exostoses: a case report. JBJS Case Connect. 2024 Jan 11;14(1):e23.00429.
What is the diagnosis?
Osteochondroma (multiple hereditary osteochondromas [exostoses])
Chondrosarcoma in cap of an osteochondroma
Lymphoproliferative disorder
Periosteal chondroma
Bizarre parosteal osteochondromatous proliferation (Nora’s lesion)

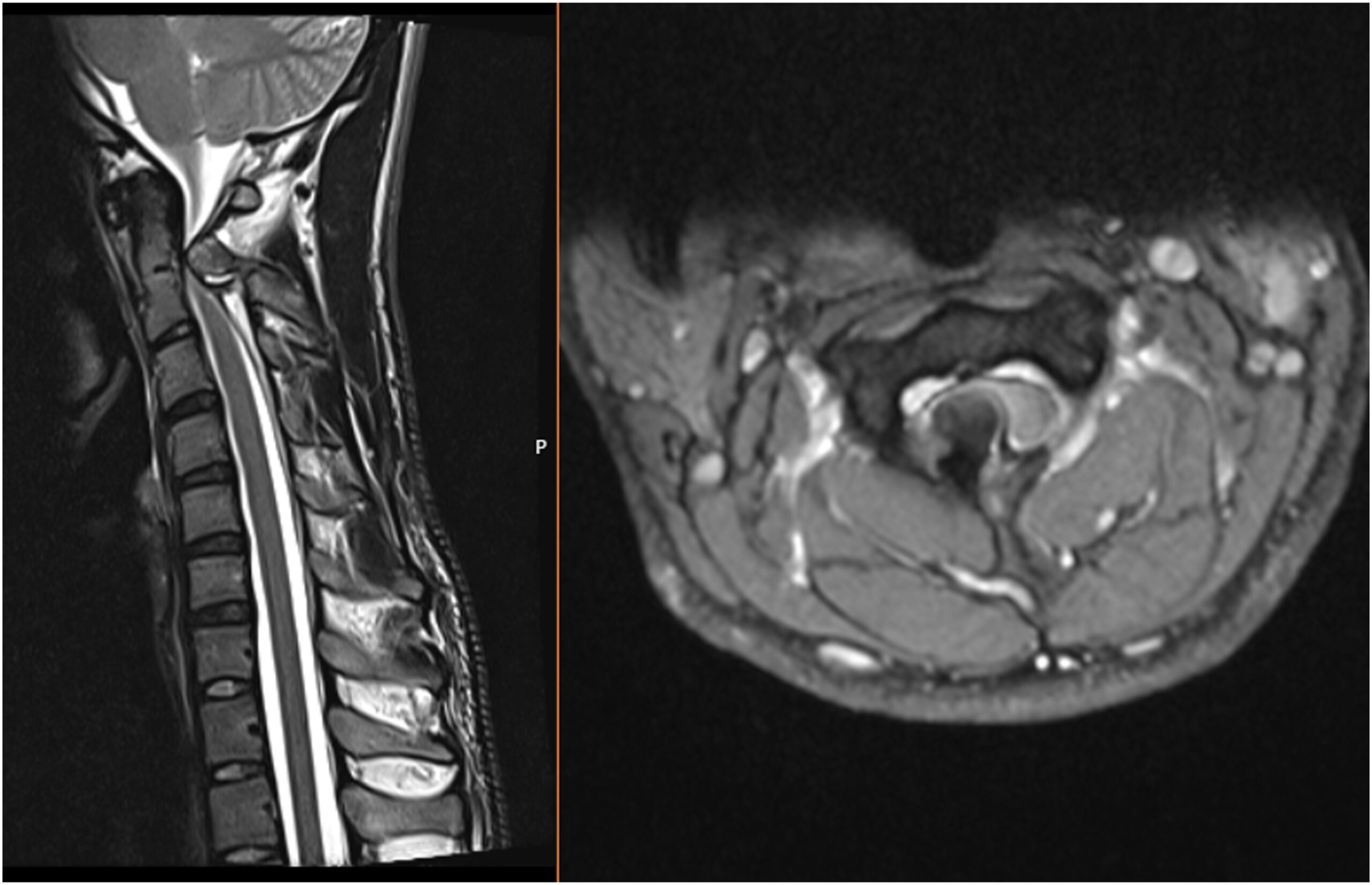
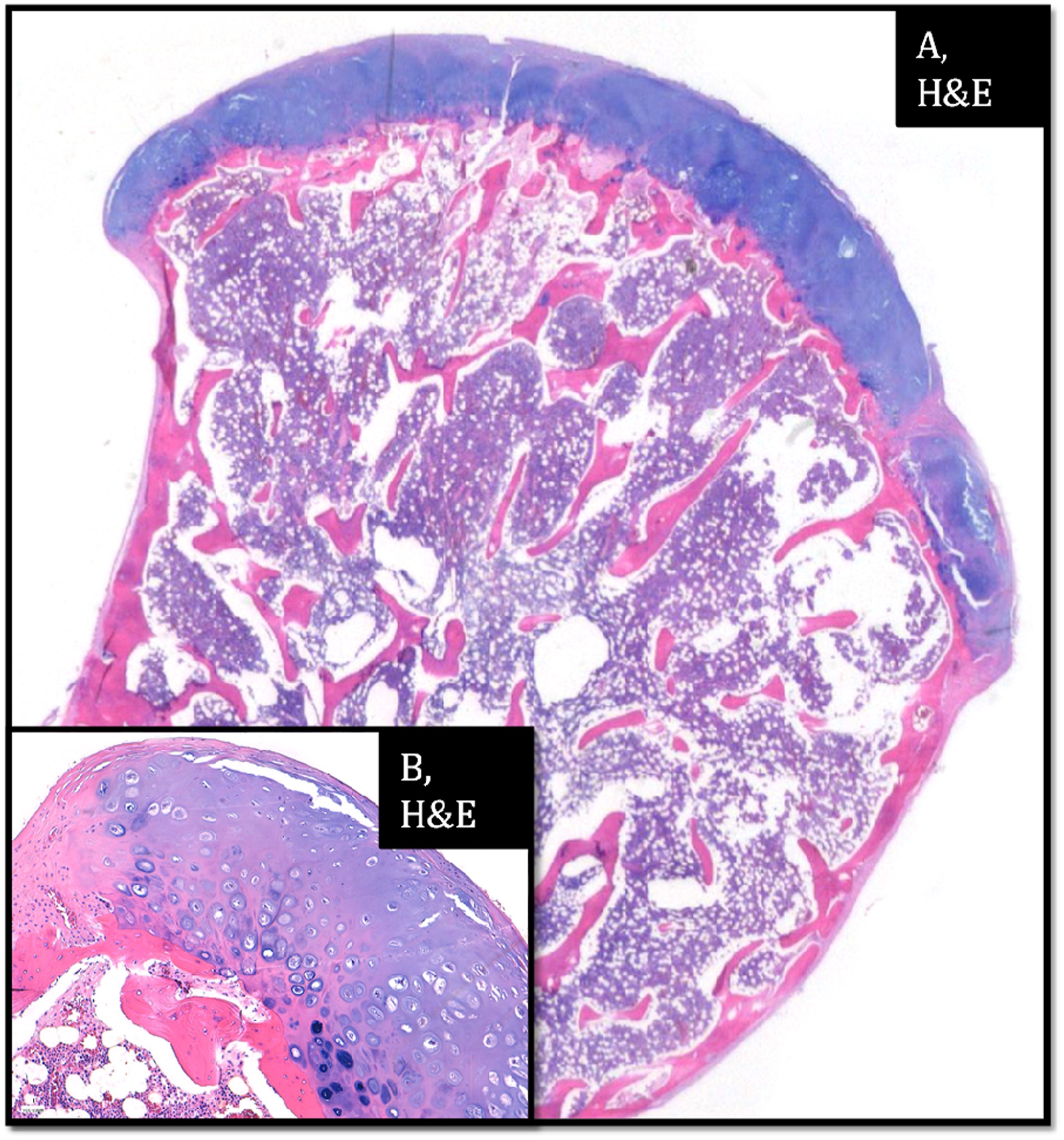
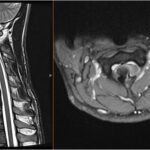 Fig. 1
Fig. 1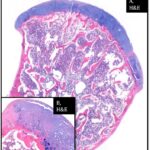 Fig. 2
Fig. 2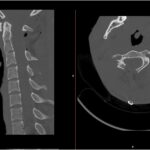 Fig. 3
Fig. 3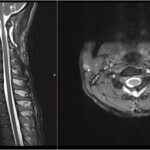 Fig. 4
Fig. 4