A 28-Year-Old Man with Long-Term Increasing Knee Pain
September 4, 2019
A 28-year-old man self-referred to our clinic after experiencing 3 years of right knee pain after using a kneeling desk. He originally had pain at night, but this progressed to all times of the day. The pain was initially relieved with nonsteroidal anti-inflammatory drugs (NSAIDs), but he remained limited in athletic and daily activities. His medical history was otherwise negative.
On physical examination, there was no effusion, moderate quadriceps atrophy, and tenderness of the medial femoral condyle. The knee range of motion was from −2° to 140°, symmetric to the contralateral knee. The examination of the patellofemoral joint was normal.
A radiograph demonstrated disuse osteopenia and a focal lucency in the medial femoral condyle (Fig. 1). Computed tomography (CT) and magnetic resonance imaging (MRI) further characterized a well-circumscribed, 8 to 10-mm, round, lucent lesion in the anterior medial femoral condyle with central mineralization and associated marrow edema (Figs. 2 and 3).
Arthroscopy revealed an intact chondral surface with softening over the far medial aspect of the medial femoral condyle corresponding to preoperative imaging measured to be 8 mm in size. A small arthrotomy was made, and the lesion was cored out as an osteochondral plug. Adequate resection was confirmed by fluoroscopic localization and visual inspection of the excised plug and recipient bed. Due to patient choice, osteochondral allograft was used as a donor plug (Fig. 4). The excised osteochondral plug was sent for pathology (Figs. 5 and 6).
The radiographic features and histology were diagnostic of an intra-articular osteoid osteoma.
Postoperatively, the patient’s pain was completely resolved. He regained full preoperative range of motion and was able to return to full activity at 6-month follow-up. A radiograph demonstrated excision of the lesion and replacement with an osteochondral graft (Fig. 7).
The patient was allowed to weight-bear as tolerated with crutches in a long hinged knee brace locked in extension for 6 weeks after surgery. A continuous passive motion machine was used for 2 weeks postoperatively. Running was initiated at 4 months once good quadriceps and core strength were demonstrated. The patient advanced to full activity by 5 to 6 months under the guidance of a physical therapist.
Proceed to Discussion >>Reference: Monroe EJ, Chambers CC, Davoodian A, Cho SJ, Motamedi D, Allen CR. Intra-articular osteoid osteoma of the distal femur treated with osteochondral grafting: a report of 2 cases. JBJS Case Connect. 2019 Apr-Jun;9(2):e0211.
Intra-articular osteoid osteoma has most commonly been described in the hip joint affecting the proximal part of the femur but has also been found within the knee, ankle, elbow, hand, subtalar, and metatarsophalangeal joints. Standard radiographs do not readily identify intra-articular osteoid osteoma, with the characteristic sclerotic rim absent in the majority. MRI assists in differentiating from osteochondral defect, subchondral cyst, infection, or stress fracture. MRI demonstrates the out-of-proportion marrow edema on T2-weighted images that is unlikely to be seen with focal chondral fissure or subchondral cyst. MRI conversely lacks the effusion, metaphyseal location, and striking sclerosis associated with the infection. Bone scans demonstrate a double density sign due to internal nidus but are not as routinely performed. CT is the preferred diagnostic imaging modality, preferably using 3-mm or thinner cuts to identify a small nidus.
Although NSAIDs are the first-line treatment of osteoid osteoma, intra-articular osteoid osteoma is less receptive to conservative care as joint involvement with synovitis can cause more morbidity. Computed tomography-guided radiofrequency ablation (CT-RFA) of classic, extra-articular osteoid osteoma is considered the gold-standard interventional treatment, with success rates upward of 90%. This technique for treating intra-articular osteoid osteoma has a theoretical risk of chondrocyte death due to thermal injury. Previous cadaveric and animal studies have demonstrated a 1-cm diameter of damage in CT-RFA. Despite this, several studies have described their experience treating intra-articular osteoid osteoma with CT-RFA with similar results to those of osteoid osteoma in diaphyseal locations. Notably, ablation technique is performed avoiding a transarticular approach most commonly for hip intra-articular osteoid osteoma, with few in directly subchondral locations. Some studies noted no apparent chondral injury at 2 years of follow-up, which may not allow adequate time for articular damage to be elucidated. Furthermore, radiographic follow-up in these studies was not pursued, and only subjective symptoms were used as a surrogate for assessing resultant articular damage. Thus, the duration of follow-up and outcome measure may inadequately quantify the subsequent articular damage.
In a case report by Bosschaert and Deprez, an intra-articular osteoid osteoma of the hip joint acetabular roof treated with CT-RFA had evidence of cartilage loss at the mid-term follow-up. The authors do acknowledge that causation cannot be determined, because the joint may have been damaged by the procedure or weakened by the presence of the tumor. In the case presented above, the articular cartilage overlying the intra-articular osteoid osteoma appeared abnormal and softened at the time of surgery, which both reinforced the senior author’s decision to treat operatively and corroborates Bosschaert and Deprez’s theory that the intra-articular tumor may affect the health of the involved articular cartilage.
Simple excision of intra-articular osteoid osteoma has been the mainstay of surgical treatment using open and arthroscopic techniques. All reports of distal femoral lesions had good pain relief and function with excision, although all described subsynovial lesions that would not result in a defect in the weight-bearing zone cartilage. Thus, in select patients, osteochondral grafting offers several advantages. With a differential diagnosis that may include osteochondral defect, this allows appropriate treatment in either scenario. Definitive diagnosis after complete excision is facilitated due to adequacy of the biopsy sample, because only 73% in a large series of osteoid osteoma had confirmative pathology results. Osteochondral grafting is routinely performed for distal femoral cartilage defects, making this a reasonable treatment choice for this location. Osteochondral grafting has also been used for intra-articular osteoid osteoma of the tibial plateau and could be considered for other anatomic locations conducive to osteochondral grafting such as the talar dome or femoral head. Although our patient was skeletally mature, this technique could hypothetically be applied to pediatric patients with adequate epiphyseal size to accommodate resection without violation of the physis.
We present a patient with a subchondral intra-articular osteoid osteoma within the distal part of the femur. In this example, radiofrequency ablation has the potential for destruction of the overlying cartilage and undertreatment of pathologically soft cartilage. Simple excision may be pain-relieving but fails to address the resultant loss of articular cartilage. We present an alternative treatment for this rare case consisting of excision and osteochondral grafting, resulting in good pain relief and restoration of the articular surface.
Reference: Monroe EJ, Chambers CC, Davoodian A, Cho SJ, Motamedi D, Allen CR. Intra-articular osteoid osteoma of the distal femur treated with osteochondral grafting: a report of 2 cases. JBJS Case Connect. 2019 Apr-Jun;9(2):e0211.
What is the diagnosis?
Brodie abscess
Periosteal chondroma
Langerhans cell granuloma (eosinophilic granuloma)
Intra-articular osteoid osteoma
Osteosarcoma


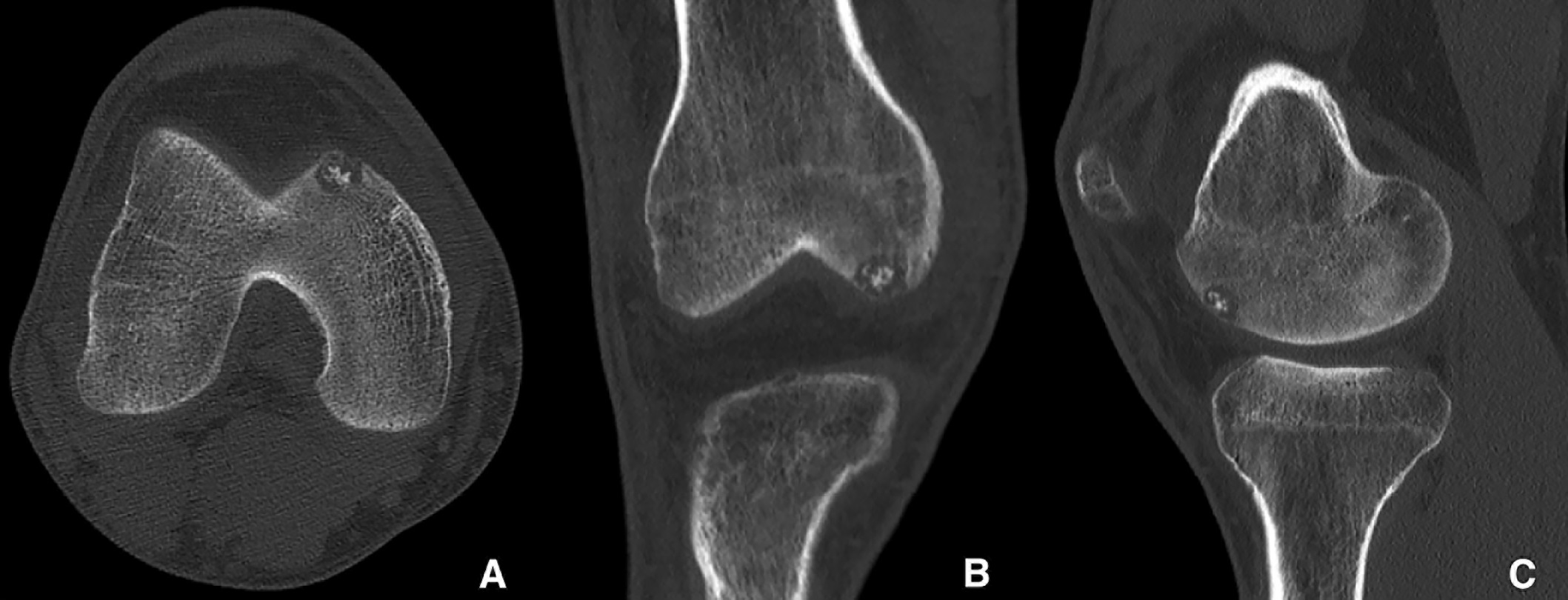
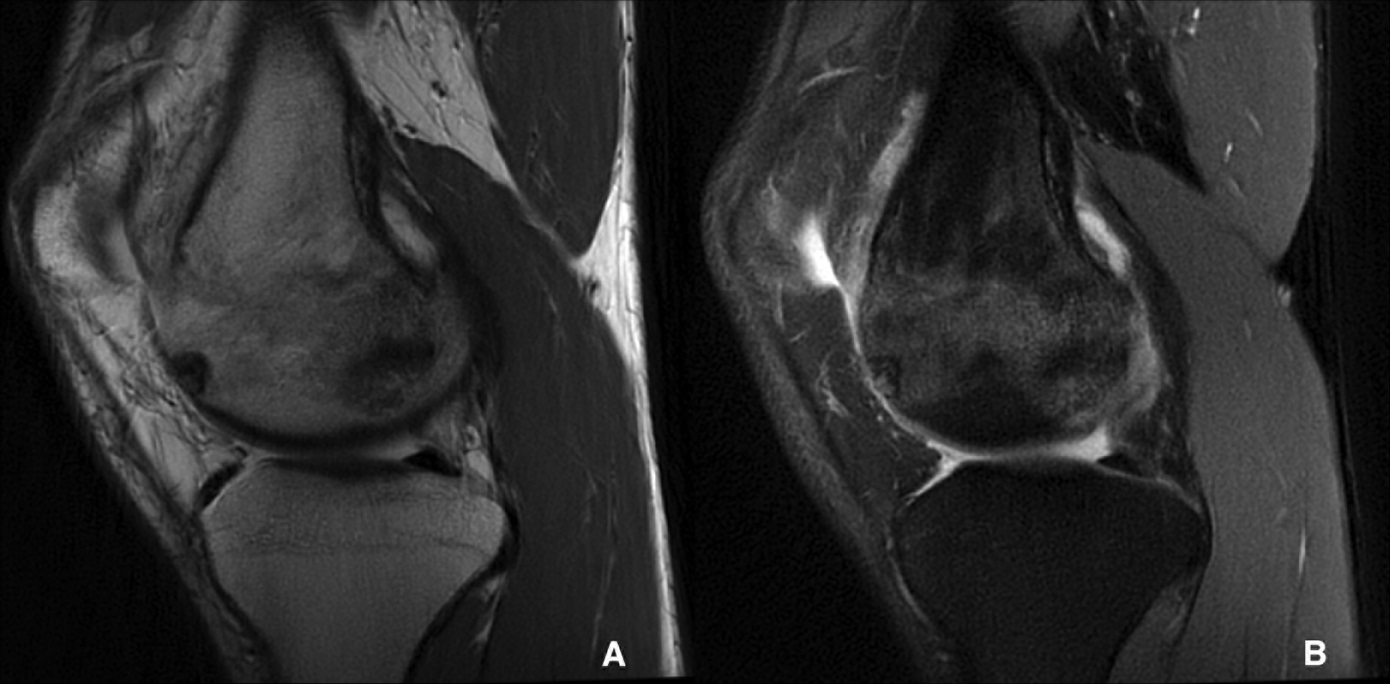
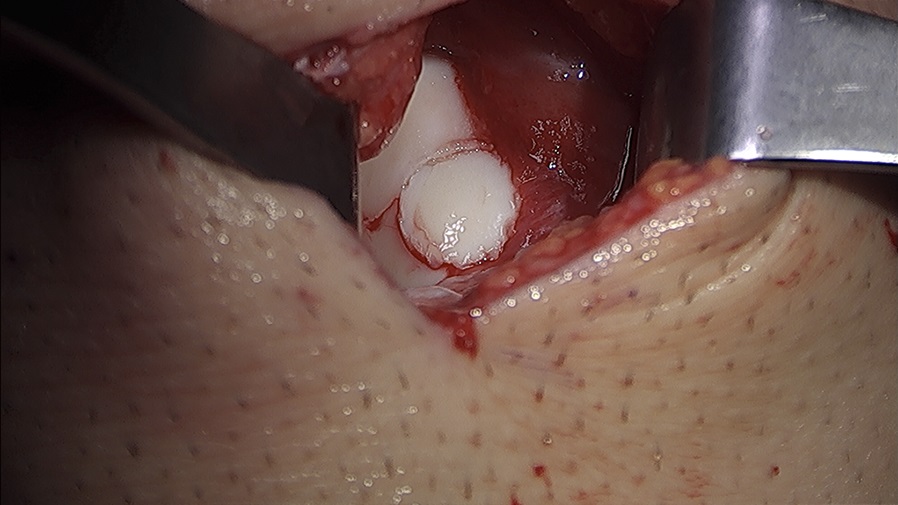
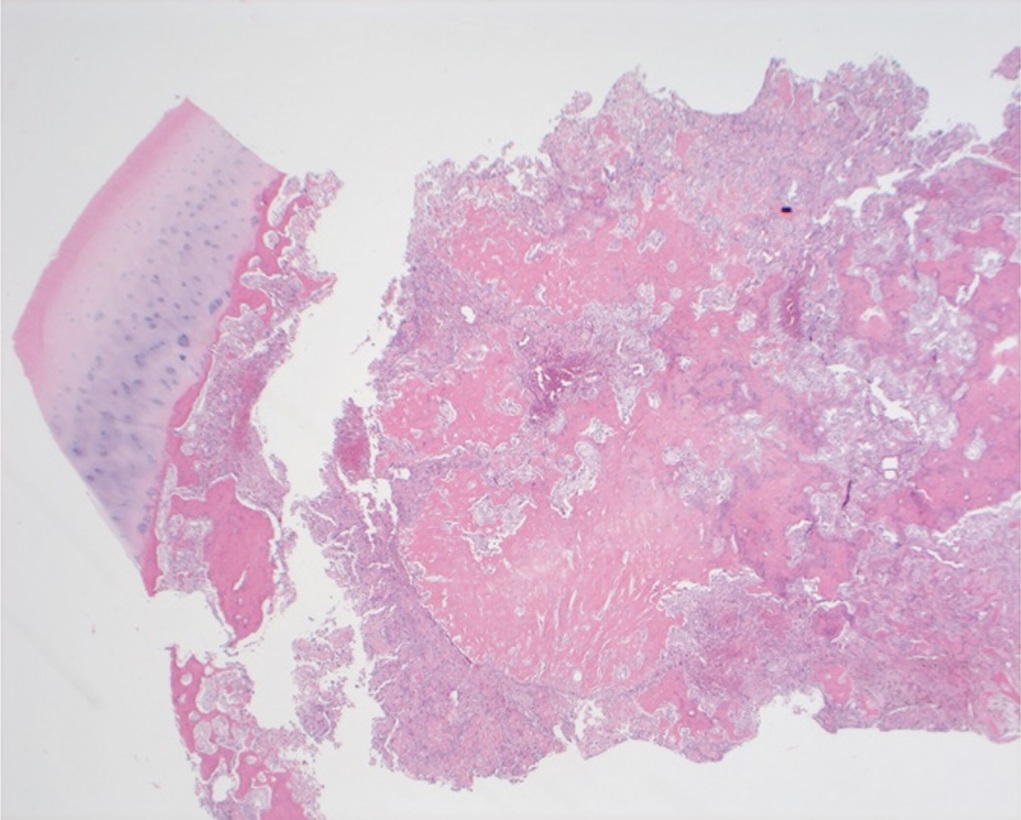
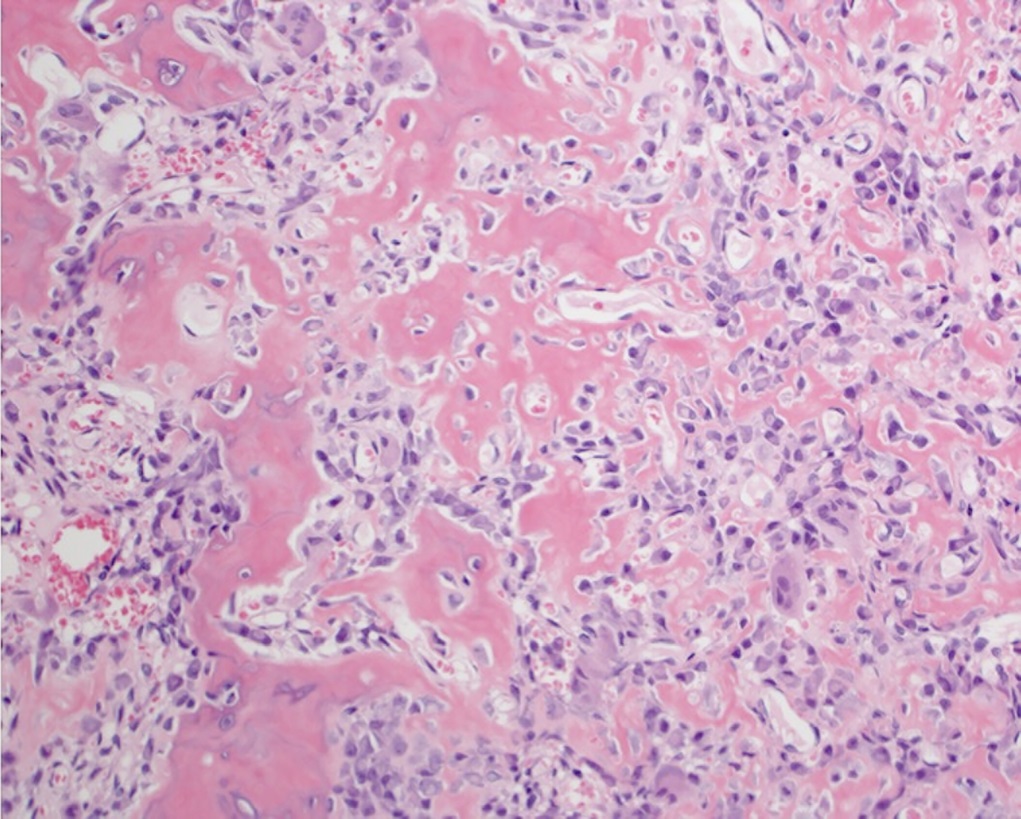
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4 Fig. 5
Fig. 5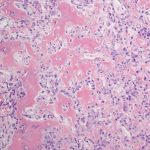 Fig. 6
Fig. 6 Fig. 7
Fig. 7