A 31-year-old, right-hand-dominant woman with a noncontributory medical history was referred to us because of 6 years of progressive discomfort in the right shoulder. Throughout this time period, she had mentioned the symptoms to her doctor; several radiographs had been made, but these never revealed any abnormalities. Subjectively, she reported pain and discomfort located mostly in the anterior aspect of the shoulder and the axilla, which radiated into the neck and down the right arm with an associated tingling sensation in the right hand. Using the 0 to 10 pain scale, she described 3 of 10 pain at rest, occasional 3 of 10 pain at night, and 10 of 10 pain with activity. She reported full range of motion with very mild limitation in function, characterized by difficulties with overhead activity and tasks that required external rotation of the shoulder. She did not report any constitutional symptoms.
On physical examination, the right axillary region, which is best examined when the patient is in the supine position with the arm overhead, showed substantial fullness, and there was a palpable nontender mass. Nearly complete range of motion of the affected shoulder was observed, with 180° of forward flexion and 160° of abduction. External rotation was limited slightly (<5°) when compared objectively to the left shoulder. The muscular strength was 5 of 5, except for some minor strength reduction in external and internal rotation of the right shoulder. The lift-off and belly-press tests demonstrated slight weakness. There were no signs of rotator cuff impingement. Sensation to light touch was diminished in the radial nerve distribution but was intact in the ulnar, median, medial and lateral antebrachial cutaneous, and axillary nerve distributions. The radial and ulnar pulses were palpable. The patient also had a separate soft mobile mass on the lateral aspect of the right shoulder, which later was excised and determined to be a lipoma.
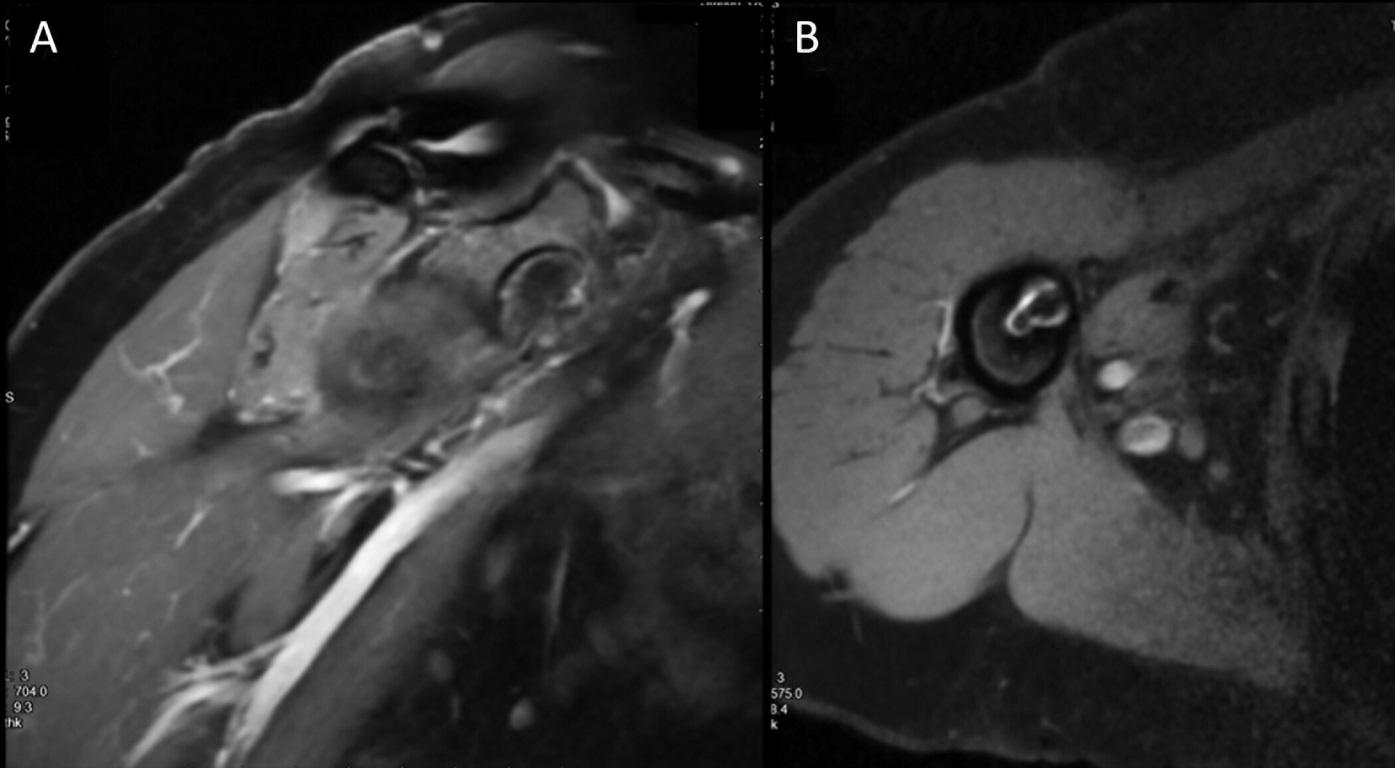
Initial radiographs demonstrated a lytic lesion in the scapular body and the shadow of a large soft-tissue mass (Fig. 1). Computed tomography (CT) confirmed a large soft-tissue mass intimately associated with the subscapularis muscle. Subsequent magnetic resonance imaging (MRI) demonstrated a soft-tissue mass (hypointense on T1-weighted images and hyperintense and heterogeneous on T2-weighted images) that was located in the anterior aspect of the scapula (Fig. 2). The mass appeared to either involve the scapula or originate from the periosteum. There were no areas of substantial necrosis. The lesion was relatively infiltrative, displacing musculature around the axillary region. Contrast enhancement was homogeneous throughout.
Because of concerns for malignancy, the patient underwent positron emission tomography (PET)/CT that demonstrated mild activity (SUVmax [maximum standardized uptake value] of 3.4) in the axillary region and no metastatic disease.
Because of the progression of the symptoms, the increased size of the mass, and the concern for malignant disease, the decision was made to surgically excise the lesion with a subtotal scapulectomy. Detachment of the pectoralis major was required for exposure. The lesion was excised as a single unit, with the attempt to achieve negative margins. The scapular spine, the coracoid, and the acromion were reattached to the remaining scapula with a 2.0 cable wire. A myodesis was performed between the periscapular muscles for closure. Primary closure of the skin was completed after 2 drains had been left in place. The arm was placed in a sling, and external rotation was restricted for 6 weeks.
The surgical specimen measured 13.4 × 9.4 × 8.3 cm with an attached 11.1 × 7.0-cm fragment of scapula. Serial sectioning revealed a white-tan well-circumscribed mass measuring 13.0 × 6.9 × 4.8 cm. The mass invaded muscle and bone, and it came within <1 mm of all margins and appeared to abut the superior resection margin. The mass demonstrated multiple cystic degenerative and myxoid areas with scattered hemorrhage. The lesion cells were negative for S100, desmin, CK (cytokeratin), MNF-116 (an anti-CK antibody), SMA (smooth muscle actin), and EMA (epithelial membrane antigen). Beta-catenin showed patchy nuclear expression (Fig. 3).
On the basis of the histology and immunocytochemical staining, the lesion excised from the patient was diagnosed as a desmoid-type fibromatosis.
Two years after the resection, the patient was doing well, with a EuroQol visual analog scale score of 90, a Toronto Extremity Salvage Score (TESS) of the upper extremity of 99, a Patient-Reported Outcomes Measurement Information System (PROMIS) Pain Interference T-score of 40.7 (on which the mean is 50 and the standard error [SE] is 5.9), a PROMIS Physical Function T-score of 55.8 (SE, 3.9), a PROMIS Physical Function Upper Extremity T-score of 50.9 (SE, 4.5), and a Musculoskeletal Tumor Society (MSTS) score of 29. The range of motion had continued to improve with the assistance of physical therapy, she remained neurovascularly intact, and she had no pain. She had 160° of forward flexion, 150° of abduction, 30° of adduction, 45° of internal rotation, and 15° of external rotation. MRI of the shoulder demonstrated no evidence of recurrent disease (Fig. 4). She will continue surveillance with MRI at 5 and 10 years if asymptomatic, or sooner if she presents with any symptoms.
Proceed to Discussion >>Reference: Ballatori SE, Hecht JL, Lozano-Calderón SA. A desmoid tumor involving the subscapularis muscle: a case report. JBJS Case Connect. 2019 Mar;9(1):e3.
Desmoid tumors of the subscapularis muscle are very rare, with few cases reported in the literature. Our case demonstrates unique symptomatology for such tumors because our patient presented with discomfort and neurologic symptoms rather than the previously described isolated limitation of external rotation. Therefore, this case report serves to highlight a distinct clinical presentation of these tumors and provides a review the available literature.
In our patient, the tumor was large and had caused progressively worsening symptoms, likely secondary to radial nerve or posterior cord compression; thus, surgical intervention was necessary. Desmoid tumors have no propensity to metastasize; nonetheless, they are capable of causing substantial morbidity through invasion of neighboring vital structures. Additionally, desmoid tumors are associated with high rates of local recurrence, especially in younger patients, which renders definitive treatment difficult to achieve. Further complicating treatment guidelines is the unpredictable behavior of desmoid tumors because some progress rapidly while others remain indolent.
Despite controversy regarding optimal desmoid tumor management, several concepts are universally accepted. For example, it is well-established that MRI is the most useful imaging modality for diagnosing and monitoring extra-abdominal desmoid tumors. MRI enables physicians to determine tumor size, location, association with neurovascular structures, and resectability. Imaging must be followed with a biopsy for a histologic diagnosis.
If the biopsy confirms the diagnosis of a desmoid tumor, the current treatment guidelines recommend an initial surveillance period to monitor the rate and extent of tumor progression. Historically, surgical resection was the gold standard treatment for extra-abdominal desmoid tumors, and tumor excision remains useful in select cases that are rapidly progressing or causing substantial pain or functional deficits. In larger tumors, or when the location renders complete surgical resection challenging, adjuvant or neoadjuvant radiation therapy may play a role in prolonging the disease-free interval; however, radiation therapy might not reduce the absolute recurrence rate. Additional treatment options include hormonal therapy, nonsteroidal anti-inflammatory drugs (NSAIDs), chemotherapy, molecular targeted therapy, and high-intensity focused ultrasound. Often, a combination of these modalities is used.
Based on a thorough review of the literature, we have found that subscapularis-associated desmoid tumors are exceedingly rare; therefore, there are no specific analyses of these tumors. Within the current literature, we found 4 confirmed cases of desmoid tumors involving the subscapularis muscle. Three of these cases described presenting symptomatology; 2 involved pain and isolated loss of external rotation of the shoulder, and the third reported no pain or associated symptoms. Of course, it is difficult to quantify the true number of subscapularis-associated desmoid tumors because many larger studies do not include specific case details.
This case report offers insight into the breadth of desmoid tumors and specifically details the presentation, diagnosis, and treatment of a rare subscapularis-involved desmoid tumor. Moving forward, it is important to keep in mind that although limited range of motion is the more common presentation for these tumors, they also can present with primarily neurologic symptoms. Larger patient cohorts are needed to improve our understanding of the different subsets of desmoid tumors.
Reference: Ballatori SE, Hecht JL, Lozano-Calderón SA. A desmoid tumor involving the subscapularis muscle: a case report. JBJS Case Connect. 2019 Mar;9(1):e3.
What is the diagnosis?
Elastofibroma
Schwannoma
Plexiform neurofibroma
Desmoid-type fibromatosis
Parosteal osteosarcoma

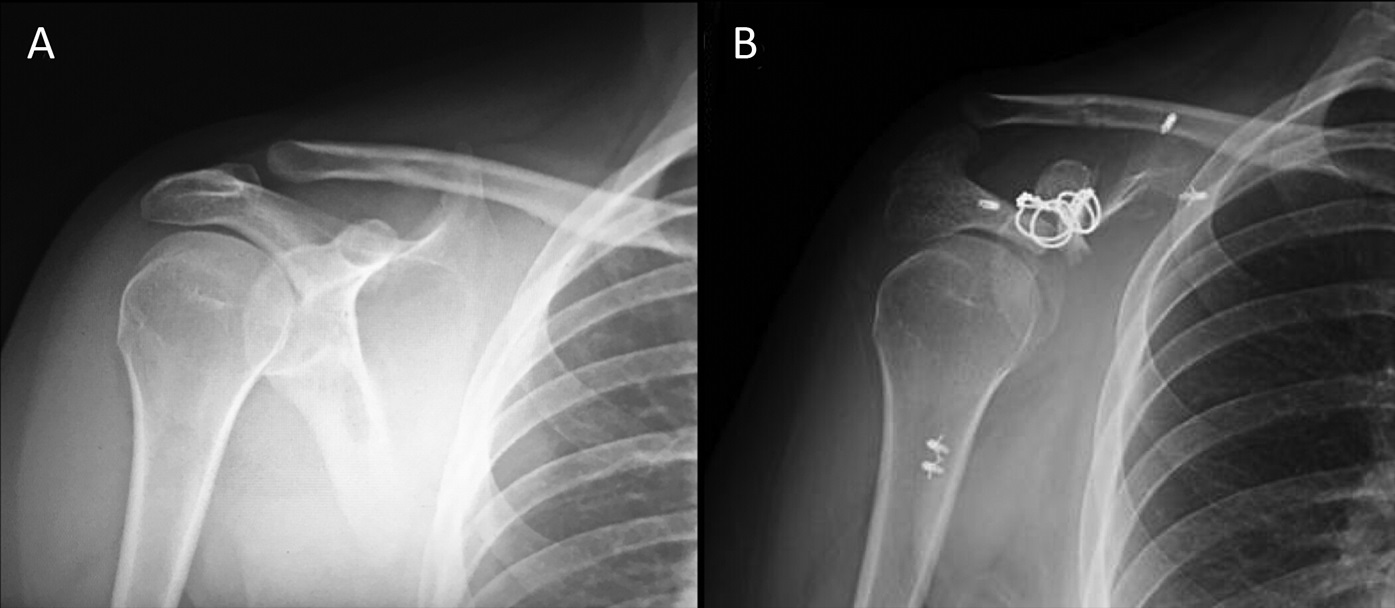
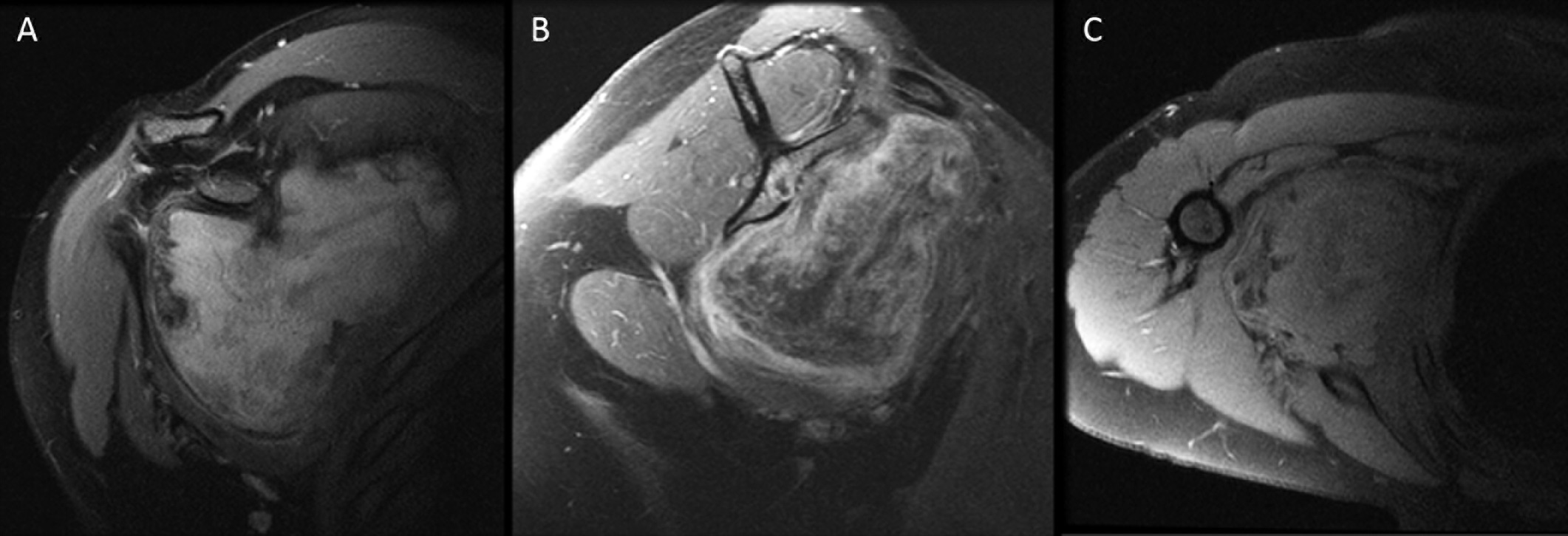

 Fig. 1
Fig. 1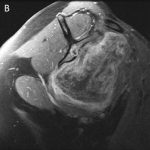 Fig. 2
Fig. 2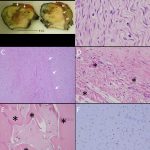 Fig. 3
Fig. 3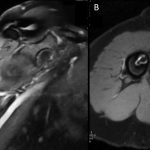 Fig. 4
Fig. 4