A 33-Year-Old Man with Activity-Induced Wrist Pain
November 6, 2019
A 33-year-old man, a right-handed plumber/electrician, presented to our clinic reporting dull pain in his right ulnar wrist, especially during work. He also reported an intermittent night pain of the right wrist. There were no injury events reported. The symptoms had lasted for 3 months, and he also noted local swelling at his right ulnar wrist. Physical examination revealed a prominence at the ulnar head area with local tenderness. There were no pulsatile mass, no soft-tissue mass, and no signs of local inflammation. Active range of motion of the involved right wrist showed almost full motion with flexion 80°, extension 80°, pronation 80°, and supination 80°. Radiographs showed an expansile and osteolytic bone lesion in his right ulnar head (Fig. 1). Magnetic resonance imaging (MRI) revealed an osteolytic lesion at the ulnar head, which expanded and extended proximally to the metaphyseal level (Fig. 2). The ulnar head was expanded, but the cortex did not break, which was graded as Campanacci grade 2. Whole-body scintigraphy showed an abnormal uptake of contrast medium at the ulnar head, with no other parts involved (Fig. 3).
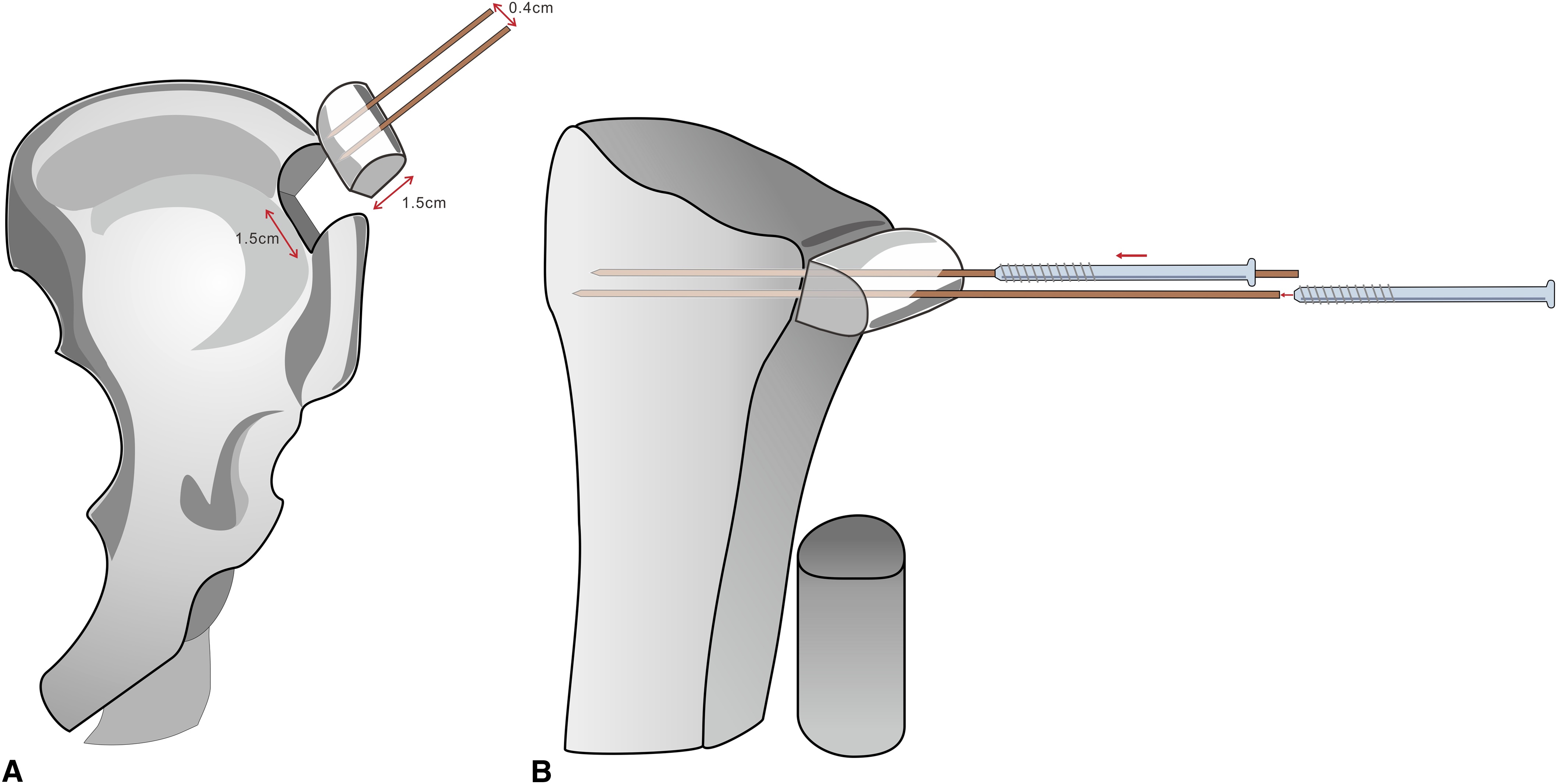
The patient then underwent excision of the ulnar head and restoration of distal radioulnar joint function using a modified Sauvé-Kapandji procedure with an iliac bone graft as ulnar support. The procedure was performed with the patient under general anesthesia and pneumatic tourniquet with the patient in the supine position and a hip roll under the pelvis to accentuate the anterior iliac crest anatomy. The incision was carried out along the interval between the flexor carpi ulnaris and the extensor carpi ulnaris tendon. A frozen section was obtained, and the lesion was resected en bloc with the proximal cutting level ensured in the preoperative MRI identification by increasing the distance from the proximal margin by 1.5 cm (Fig. 4). The distal part was resected with preservation of the triangular fibrocartilage fovea insertion together with ulnar head attachment of the volar/dorsal radioulnar ligament and ulnar collateral ligaments.
The histology of the resected lesion is shown in (Fig. 5).
Both frozen section and tissue processed for permanent sections showed clusters of osteoclast-like giant cells in a background of mononuclear cells. Dilated vascular spaces are not evident. These findings are typical of a giant cell tumor of bone.
The width of the radial sigmoid notch was 1.5 cm. The measurement of the medial-lateral distance of the ulnar head, at the most distal cortex that was not deformed by the tumor, was also 1.5 cm. So the plan was to harvest the bone graft from the anterior iliac crest as a whole width, with a length of 1.5 cm and a height of 1.5 cm (Fig. 6). We used the area, 1.5 cm × 1.5 cm, of the bone graft to take the place of the ulnar head area in the axial plane with the hyaline cartilage cap as the most ulnar side.
After resecting the tumor, it is very important to use different instruments and gloves when we proceed to the next procedure, to avoid cross-contamination. In performing the Sauvé-Kapandji procedure, we preferred to fix the ulnar-supporting bone with 2 screws, which could possibly make the fixation more stable and prevent rotation of the bone fragment. So our method is that we set 2 guide pins (1.1 mm in size) of 3.0-mm cannulated screws (Synthes) on the iliac bone graft before cutting the bone graft. Because the head of the 3.0-mm cannulated screw is 4.0 mm in diameter, the guide pins should be set in the center of the bone graft but at a distance of at least 4 mm away from each other in the longest axis of the bone graft to avoid the screw head overlapping. The 2 guide pins were set with a 6-mm distance between them. It is important not to drive the guide pins more than 1.5 cm into the iliac crest, because the osteotomy at the bottom will be performed 1.5 cm from the top of the iliac crest. Then we can perform the osteotomies (Fig. 6).
The bone graft can then be seated. Before that, the sigmoid notch was prepared with the removal of the cartilage and was flattened out to fit the bone graft. After the fitness was confirmed, the guide pins were driven directly forward into the radius. The graft was set to be at a mild ulnar-minus variance of 1 mm. The guide pins were then shifted to cannulated screw fixation using drilling and tapping procedures (Fig. 6).
The triangular fibrocartilage complex, volar/dorsal radioulnar ligaments, and ulnar collateral ligament were sutured to the ulnar margin of the bone graft, using 2-0 Ethibond (Ethicon) sutures. Drilling small holes with a 1.0-mm diameter drill bit or Kirschner wire on the ulnar margin of the bone graft can facilitate the fixation of the sutures. The proximal ulnar stump stabilization was performed using the distal-based half-slip of the extensor carpi ulnaris as tenodesis. The patient used a sugar-tong splint for 1 month postoperatively. Then weight-bearing and wrist rotation rehabilitation were begun. The patient was allowed to return to his previous activities and work at 3 months after the surgery. In the final 12-month follow-up, the radiographs showed good healing of the bone graft to the radius (Fig. 7). No recurrence of the tumor was noticed on a computed tomography scan. The patient had regained almost full active wrist range of motion with flexion 80°, extension 80°, pronation 70°, and supination 70° and did not report any symptoms around the proximal ulnar stump. The abbreviated Disabilities of the Arm, Shoulder and Hand Questionnaire (QuickDASH) score improved from 16 preoperatively to 4.5 postoperatively. The patient was able to return to his previous full level of manual work without pain or limitation. Also, despite the screw heads looking somewhat prominent on radiographs, the patient did not have any symptoms related to these and the screws had not been removed.
Proceed to Discussion >>Reference: Tsai TC, Chen CC, Huang HK, Wang JP. Modified Sauvé-Kapandji procedure using iliac bone graft for giant cell tumor of the distal ulna: stabilizing with two-screw fixation: a case report. JBJS Case Connect. 2019 Apr-Jun;9(2):e0299.
Wide excision for the removal of the tumor and the Sauvé-Kapandji procedure for restoring distal radioulnar joint function are good ways to solve both problems together. The use of the iliac crest for the reconstruction of the ulnar head after resecting a giant cell tumor has been reported. The iliac bone graft was adopted as ulnar support in the Sauvé-Kapandji procedure with the screw or Kirschner wire fixation. The use of 2 screws for ulnar support bone fixation in the Sauvé-Kapandji procedure is reasonably more stable than the use of 1-screw fixation. But when dealing with a small piece of bone, fixation with 2 screws in the bone may not be so easy. Some authors like to use 1-screw fixation and an additional Kirschner wire to achieve more stabilization, if needed. However, there could be more complications associated with Kirschner wire fixation, including Kirschner wire loosening or irritation of the skin or of the dorsal branch of the ulnar nerve, especially in young, active patients.
Therefore, we present this method using 2 preset guide pins when harvesting the bone graft. It will be easier to handle the bone graft, and the guide pins can be transfixed into the proper location of the sigmoid notch as a temporary fixation for the bone graft. The guide pins can then be shifted to the cannulated screw. In this manner, the location of the bone graft and screws can be set precisely and smoothly. Also, the headless compression screws would be another option for fixation in this procedure, but they were not used in this case because the patient could not financially afford them.
The Sauvé-Kapandji procedure has a potential risk of painful instability of the proximal ulna stump. The need for stabilizing the proximal stump after the Sauvé-Kapandji procedure is controversial. Although our case did not report of the symptoms of the unstable proximal ulna, long-term follow-up is still needed.
In conclusion, for a giant cell tumor in the ulnar head, wide resection followed by the modified Sauvé-Kapandji procedure using an anterior iliac bone graft could be a choice of treatment. The 2 guide pins preset in the iliac crest before harvest could help to perform the procedure more smoothly.
Reference: Tsai TC, Chen CC, Huang HK, Wang JP. Modified Sauvé-Kapandji procedure using iliac bone graft for giant cell tumor of the distal ulna: stabilizing with two-screw fixation: a case report. JBJS Case Connect. 2019 Apr-Jun;9(2):e0299.
What is the diagnosis?
Giant cell tumor of bone
Aneurysmal bone cyst
Giant cell reparative granuloma
Adamantinoma
Atypical megakaryocytes and fibrosis consistent with myelodysplasia



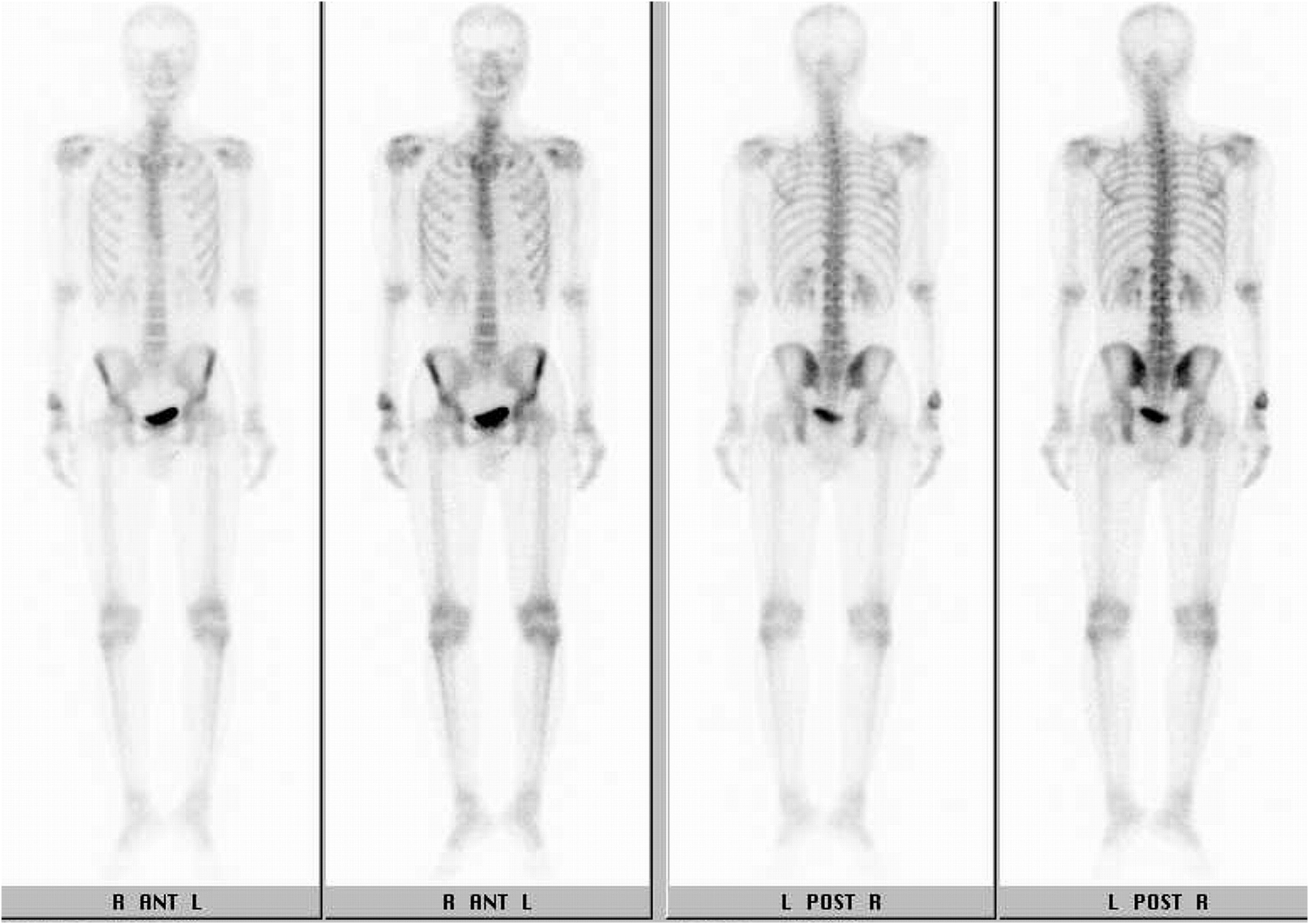

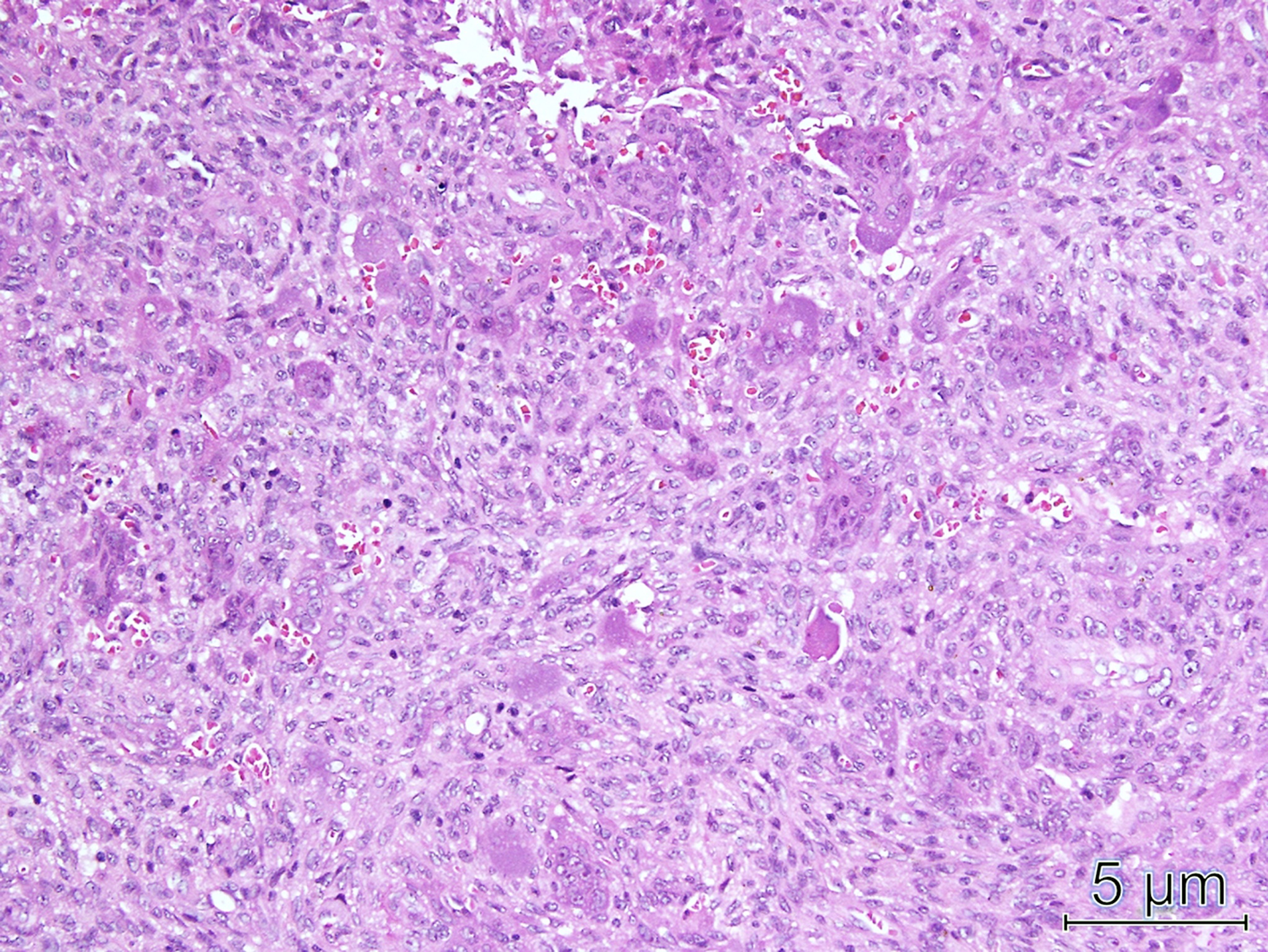
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4![Fig. 5 Fig. 5 Histology of the frozen and permanent sections of the lesion (hematoxylin and eosin [H&E] stain, ×200).](https://quiz.jbjs.org/wp-content/uploads/2019/11/iqnov19-21_fig5-150x150.jpeg) Fig. 5
Fig. 5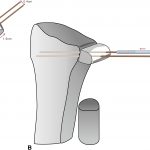 Fig. 6
Fig. 6 Fig. 7
Fig. 7