A 37-Year-Old Woman with Long-Term Worsening Back Pain
December 4, 2019
A 37-year-old woman presented with right-sided low back pain of 5 years’ duration. One month before admission, she developed bilateral leg pain and numbness, which was more prominent on the right side. The pain became worse at night and forced her to be confined to bed. No history of trauma was reported. The family history was unremarkable. Conservative treatment, including the use of nonsteroidal anti-inflammatory drugs and bracing, failed.
Physical examination revealed tenderness over the right paravertebral area of L4. The spinal range of motion was impaired. The straight leg raise test was positive at 40° on the right side and 50° on the left side. Sensation to pinprick was diminished between the L4 and L5 dermatomes on both sides, but especially on the right side. There were motor deficits. No endocrinological dysfunction or skin pigmentation was present. Deep tendon reflexes were symmetrical. Laboratory investigation, including total blood-cell count, hormone levels, erythrocyte sedimentation rate, C-reactive protein level, cancer marker (alpha-fetoprotein [AFP], CA10, carcinoembroyonic antigen [CEA]) levels, electrolytes, and alkaline phosphatase levels were all within normal range.
Radiographs of the lumbar spine showed an isolated, well-defined, radiolucent lesion of the L4 vertebra, with mild collapse of the vertebral plate (Fig. 1). Computed tomography (CT) demonstrated a round lytic lesion with a thinned but intact sclerotic margin localized in the anterior right paramedian region of the L4 vertebral body (Fig. 2). Magnetic resonance imaging (MRI) exhibited hypointensity of the L4 vertebra on the T1-weighted image (Fig. 3-A) and heterogeneous signal intensity on the T2-weighted image (Fig. 3-B). Moreover, a hypointense halo surrounding the lesion was evident on both the T1-weighted image (Fig. 3-A) and the T2-weighted image (Fig. 3-C). In addition, we found a high-intensity zone (Fig. 3-B) and disc herniation on the left side at the L4-L5 level (Fig. 3-D).
Because the patient did not receive any effective reduction of pain after conservative treatment, she decided to undergo surgery. We believe that the symptoms resulted from a combination of an L4 vertebral lesion with mild collapse and disc herniation at the L4-L5 level. Consequently, a laminectomy was performed at L4; additionally, because the patient was found to have compression of the nerve root on the left side at the L4-L5 level, a left-sided discectomy was performed. Because of the right-sided neurological deficit, exploration of the right side also was performed; however, no disc protrusion or abnormality of ligaments was observed. Next, the L4 vertebral lesion was curetted as much as possible through the right pedicle of L4 and filled with autogenous bone graft. A posterolateral fusion was performed from L3 to L5 with a pedicle screw system and autogenous bone grafts to prevent possible pathological fractures.
The histology of the excised tissue is shown in Figures 4-A and 4-B.
The histology showed a fibro-osseous lesion with irregular spicules of partially woven bone, many in the shape of the letters C or S. The final pathological diagnosis was fibrous dysplasia.
The patient experienced a substantial reduction of pain. Before surgery, the visual analog scale score was 9 of 10; after surgery, the score was 0. The neurologic status improved rapidly and was normal at 1 month postoperatively. At the 3-month follow-up, she was back to full activities without pain. At 2 years, she remained asymptomatic, and CT and MRI confirmed no involvement of the adjoining bone or progression to encompass the bone grafts, although there was a residual cystic area in the anterior part of the vertebra (Fig. 5).
Proceed to Discussion >>Reference: Yu B, Wu D, Lin Y, Zhao W, Zhu J, Huang Y, Shen B, Han Y, Qi D. Monostotic fibrous dysplasia of the lumbar vertebra. A case report and review of the literature. JBJS Case Connect. 2014 Jan;4(1):e9.
Fibrous dysplasia is a rare developmental disorder that was first described by Lichtenstein in 1938. The etiology of this anomaly has been linked to activating mutations of the GNAS gene that encodes the alpha subunit of stimulatory G protein located at chromosome 20q13.2-13.3. According to the number of affected bones, it is classified in two forms: monostotic and polyostotic. The monostotic form occurs more frequently (80%) than the polyostotic variant (20%); however, spinal involvement is more common with polyostotic fibrous dysplasia (7% to 24%) than with monostotic fibrous dysplasia (1%). Monostotic lumbar spinal manifestation is exceedingly rare; to the best of our knowledge, only 15 cases of lumbar monostotic fibrous dysplasia have been published previously.
Monostotic fibrous dysplasia usually presents with no sex predilection and is primarily observed during childhood or early adolescence; it generally becomes quiescent as puberty terminates. Including the present case, we studied a total of 16 cases of lumbar monostotic fibrous dysplasia. There were 5 men and 11 women, with a slight female preponderance (despite the fact that there is usually no sex predilection), and the age of the patients ranged from 12 to 61 years, with a median age of 36.1 years (the age of one patient was not available). It is uncertain whether our case represented de novo postpubertal monostotic fibrous dysplasia or perhaps prepubertal monostotic fibrous dysplasia; however, we think the latter is more likely. While reviewing the 16 patients, we found that every level of the lumbar spine had been affected, with L3 being the most common. There was involvement of the vertebral body in 12 cases, the pedicle in 5 cases, the transverse process in 5 cases, the lamina in 3 cases, the articular process in 2 cases, and the spinous process in 1 case. Apparently, the vertebral body was the most frequently affected location, probably because of the relatively large amount of cancellous bone. Some researchers have opined that fibrous dysplasia in the spine might start in the vertebral body and then continuously expand into the posterior elements via the pedicles.
The majority of monostotic fibrous dysplasia lesions are asymptomatic and are discovered incidentally on radiographs. Symptomatic cases may manifest pain, deformity, fracture, and nerve entrapment. The most common symptom in the 16 reviewed patients was localized pain; 4 cases had neurological impairment, and 3 cases had prior history of trauma. Proschek et al. stated that adult patients usually do not become symptomatic as a result of the fibrous dysplasia, but rather because of the degenerative changes of the affected motion segment. In our patient, there was a mild vertebral collapse of the affected segment and disc herniation of the adjacent level. The disc herniation sometimes can cause contralateral radiculopathy. The symptoms may have resulted from secondary weakening and degenerative changes of the affected segment. In addition, ectopic sprouting and formation of neuroma-like structures in sensory and sympathetic nerve fibers may occur in the dysplastic skeleton. Moreover, ligamentum flavum, dura mater, and arachnoid mater may all be denuded by fibrous dysplasia.
Radiologically, fibrous dysplasia typically exhibits ground-glass appearance with a variable degree of marginal sclerosis. CT is the best technique for demonstrating the radiographic features of fibrous dysplasia. However, radiographic findings are often not specific for fibrous dysplasia, as with our patient. On MRI, fibrous dysplasia shows variable characteristics, typically intermediate-to-low signal intensity on T1-weighted images and variable signal intensity on T2-weighted images. Also, a surrounding hypointense halo on both sequences is often present, corresponding to sclerotic margins. The main differential diagnosis includes osteoblastoma, aneurysmal bone cyst, vertebral hemangioma, and giant-cell tumor. Histological examination is essential. The histological features of fibrous dysplasia are characterized by a fibrous stroma containing irregularly shaped trabeculae of woven bone that lack osteoblastic rimming.
Because of its rare occurrence and the short-term follow-up of the reported studies, the ideal treatment of lumbar monostotic fibrous dysplasia remains a challenge. Management options vary from conservative methods such as observation and bisphosphonate pamidronate to surgical intervention. The only medications that have shown any efficacy for fibrous dysplasia are the bisphosphonates. Because fibrous dysplasia is a disease with excessive osteoclastic activity, bisphosphonate pamidronate, which inhibits osteoclasts, has been advocated, especially in the polyostotic type and following surgery. Although pamidronate has been shown to decrease pain intensity, it has no effect on the natural history of the disease.
Surgery is indicated for confirmatory biopsy, correction of the deformity, prevention of pathological fracture, and/or eradication of symptomatic lesions. Some practitioners recommended aggressive resection and stabilization for patients with monostotic fibrous dysplasia of the spine. This approach may be a result of concern about the risk of malignant transformation of the residuum. However, malignant transformation of fibrous dysplasia is uncommon, occurring in only about 0.5% of patients with monostotic fibrous dysplasia. Curettage with bone-grafting may work in smaller monostotic lesions. Although grafting materials of any type are often absorbed and replaced with fibrous dysplasia, which has occurred in 50% of patients with polyostotic fibrous dysplasia, it has been rare in patients with monostotic fibrous dysplasia. Stephenson et al. found that 86% of patients obtained satisfactory results when internal fixation was used in conjunction with open curettage and bone-grafting. The long-term prognosis for monostotic fibrous dysplasia is generally good, regardless of the therapy used, even with invasion of the graft by fibrous dysplasia. In our review, of the 12 cases for which the outcome of treatment was reported, 9 cases that had been managed with any kind of method received a good outcome. In our case, the patient remained asymptomatic, although there was a small residuum in the anterior part of the vertebra at the 2-year follow-up.
Reference: Yu B, Wu D, Lin Y, Zhao W, Zhu J, Huang Y, Shen B, Han Y, Qi D. Monostotic fibrous dysplasia of the lumbar vertebra. A case report and review of the literature. JBJS Case Connect. 2014 Jan;4(1):e9.
What is the diagnosis?
Osteomalacia
Fibrous dysplasia
Paget disease
Erdheim-Chester disease
Granulomatous inflammation consistent with mycobacterial infection

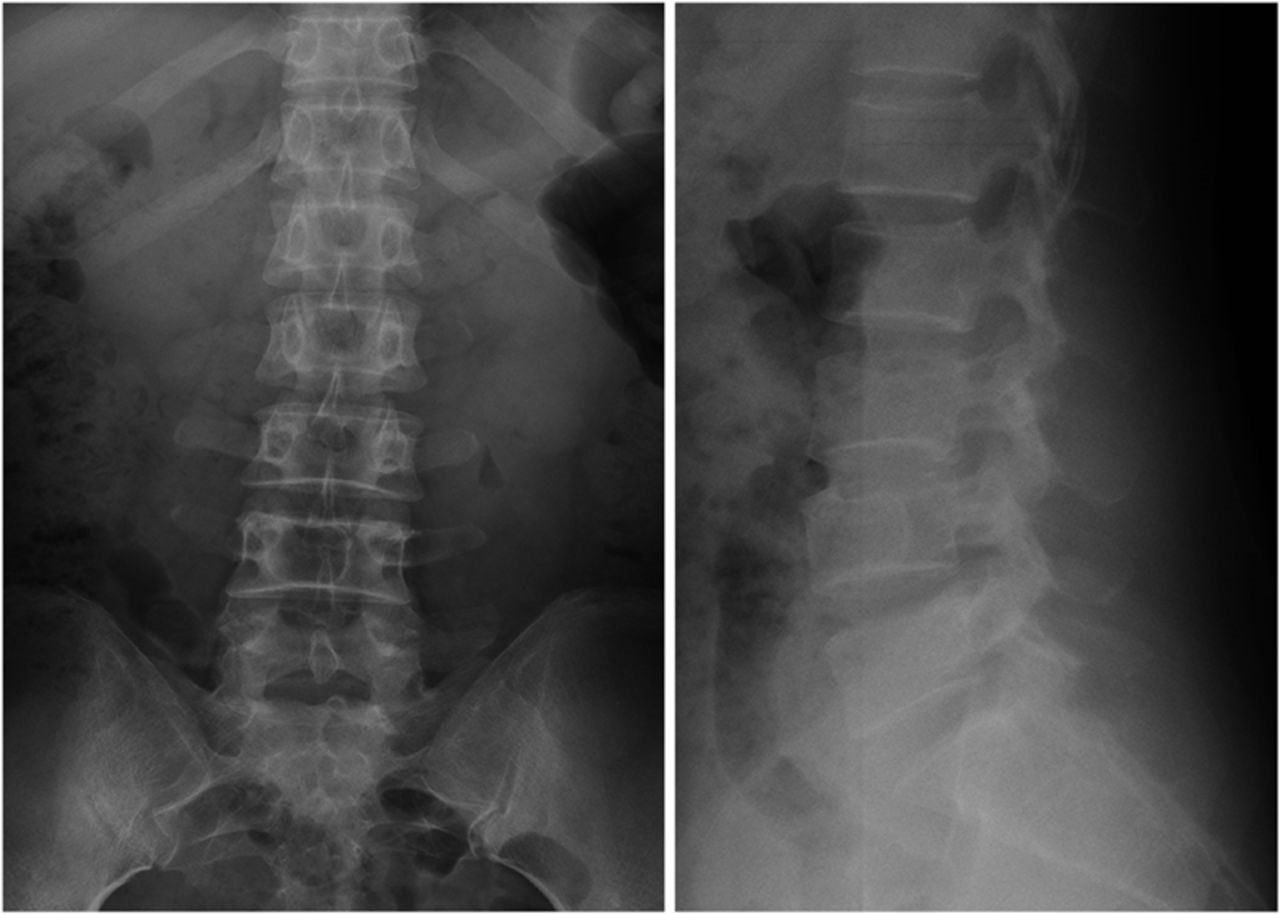
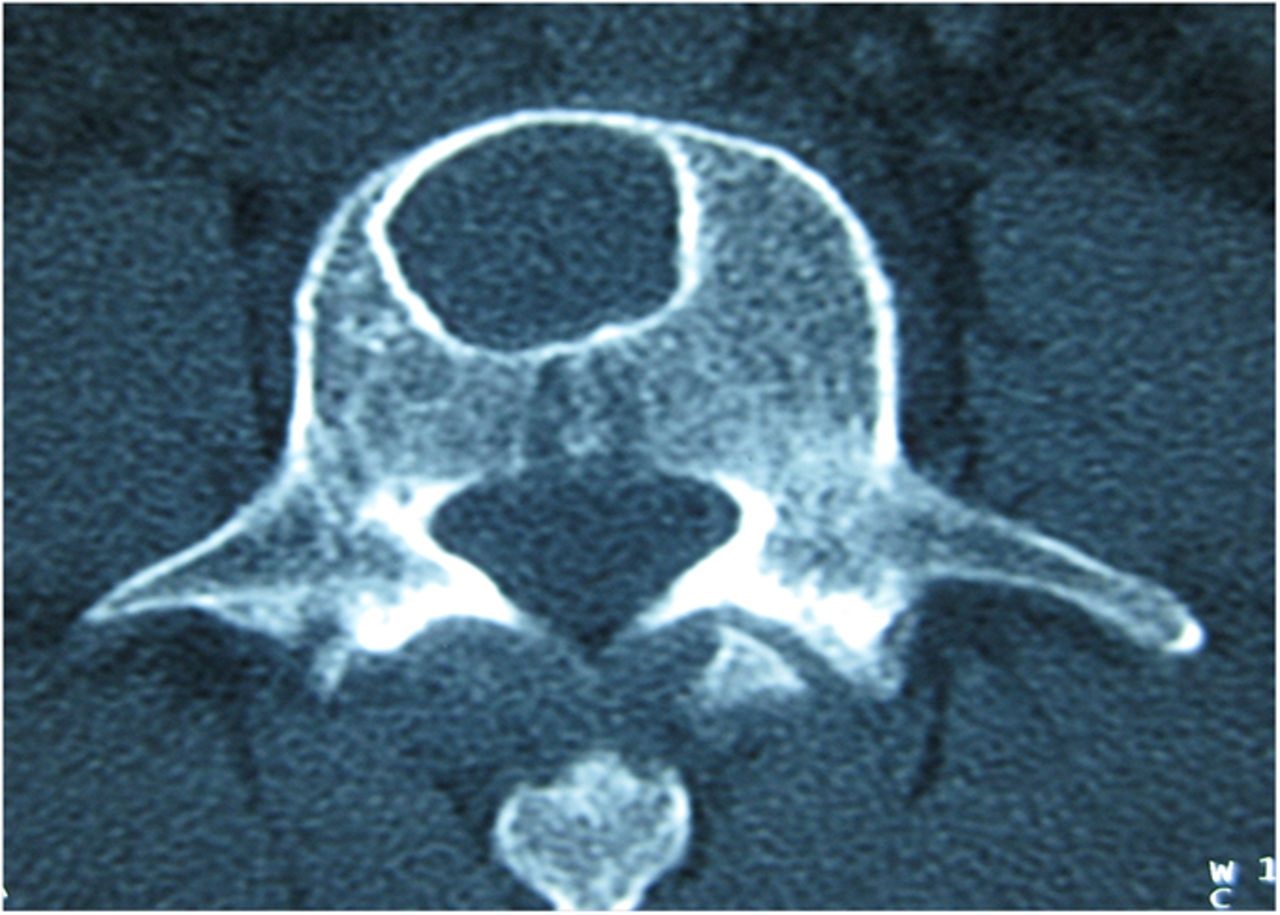

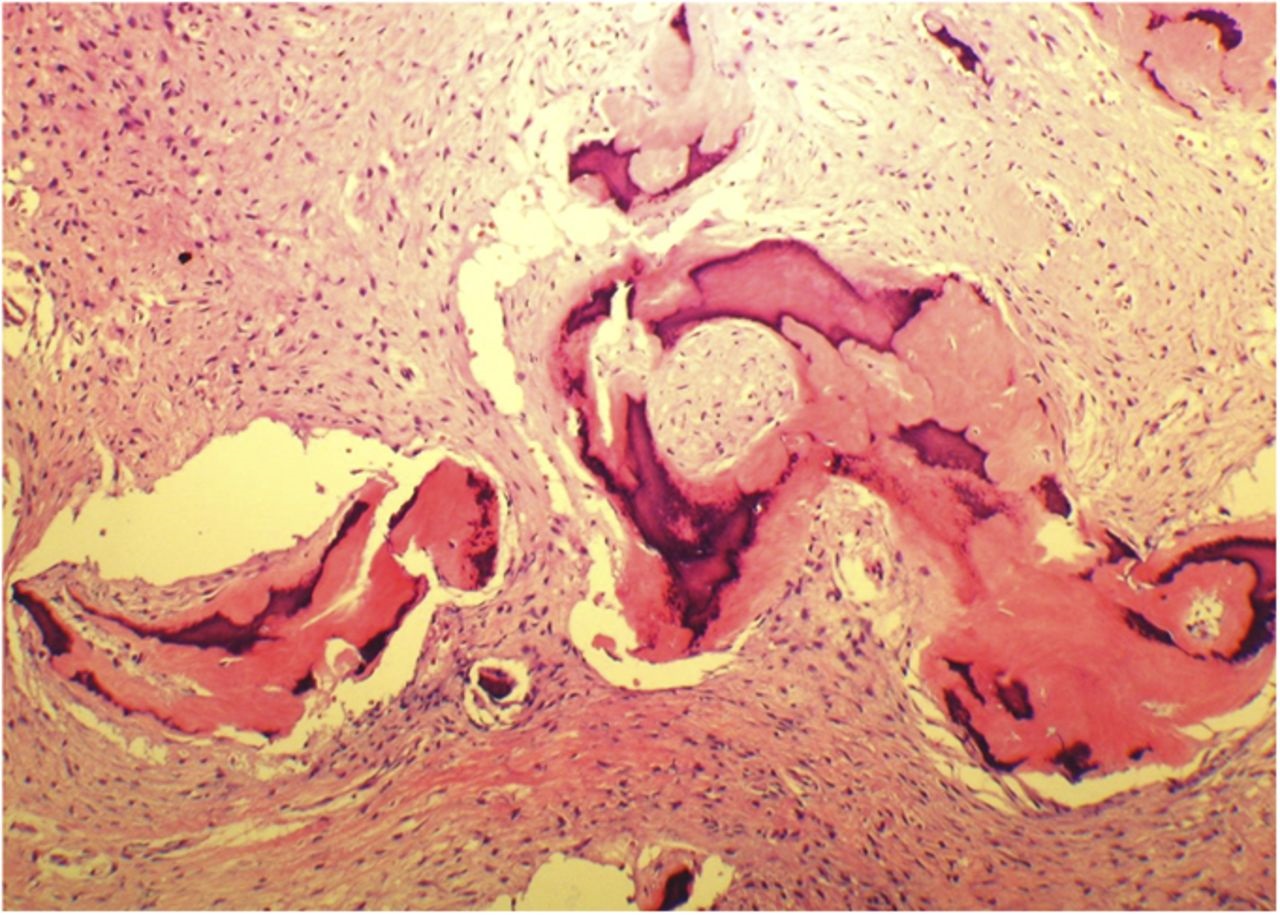
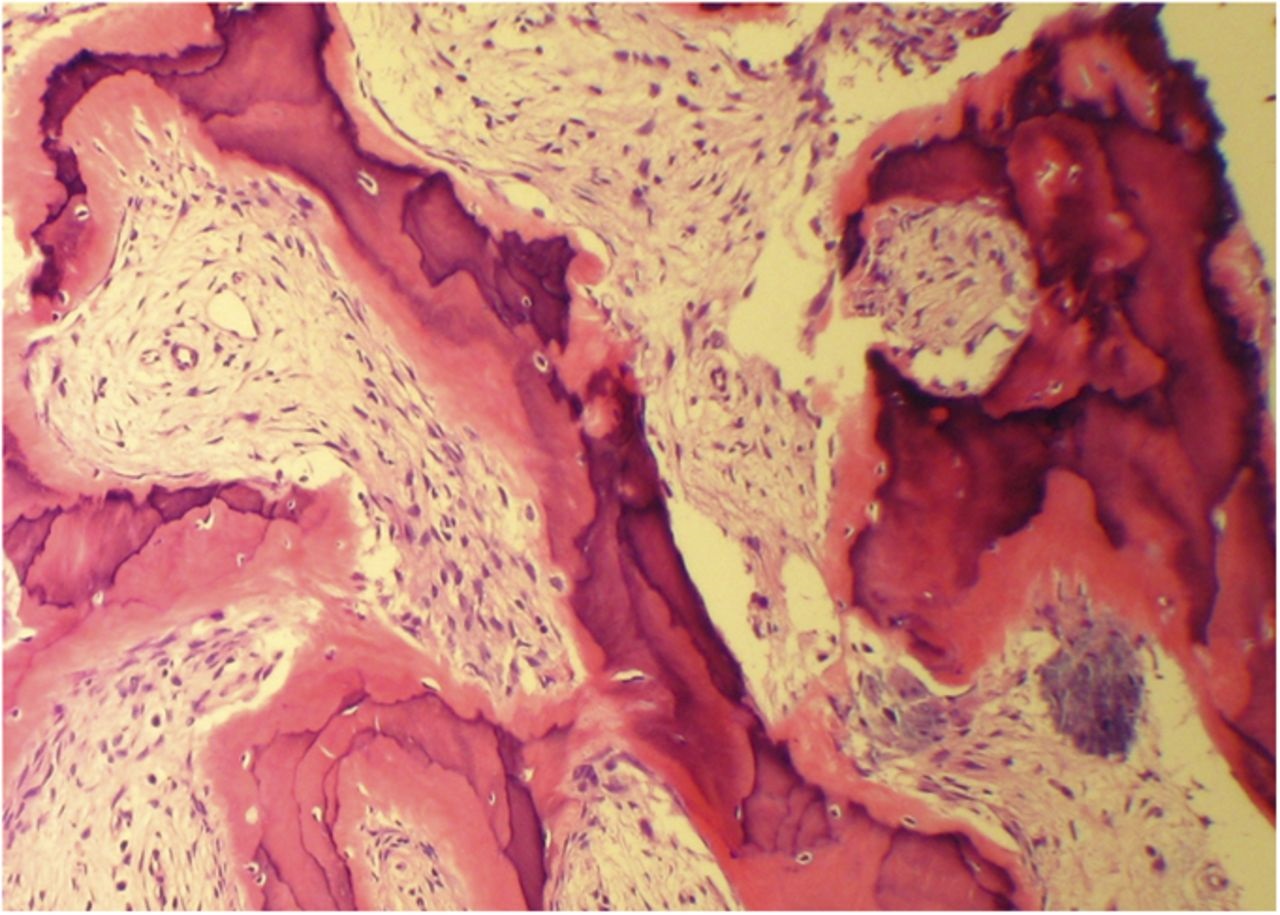
 Fig. 1
Fig. 1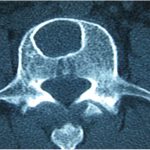 Fig. 2
Fig. 2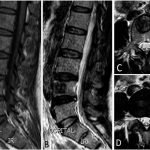 Fig. 3
Fig. 3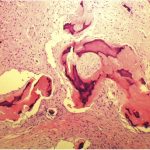 Fig. 4-A
Fig. 4-A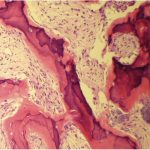 Fig. 4-B
Fig. 4-B Fig. 5
Fig. 5