A 56-Year-Old Woman with Progressive Shoulder Pain
May 5, 2021
A 56-year-old woman presented to our clinic with a 3-week history of atraumatic, progressive left shoulder pain with insidious onset. She had a medical history of hyperhomocysteinemia, heterozygous methylenetetrahydrofolate reductase (MTHFR) C677T polymorphism discovered through genetic screening for cardiovascular risk, and hyperlipidemia. She reported no use of oral steroids, family history of osteonecrosis, alcohol abuse, or traumatic injury. She had a surgical history positive for a fracture of the left tibia and fibula treated with an intramedullary rod, a left bunionectomy, 2 cesarean sections, a hysterectomy, and an appendectomy. She had recently started taking methylated B2, fish oil, vitamin D, and a multivitamin, and she had allergies to Ceftin (cefuroxime axetil), codeine, and Dilaudid (hydromorphone). Before presentation, she had received acupuncture treatments to address the shoulder pain. She had a noncontributory family history and reported not having any relatives with Gaucher disease or sickle cell anemia. She worked as a transplant nurse and did not smoke or abuse alcohol.
On physical examination, the patient was found to have normal scapular posture and motion. She had a normal examination on the contralateral unaffected shoulder with intact forward elevation to 160°, abduction, external rotation, and internal rotation to the thoracolumbar junction. On the left side, she had forward elevation to 155°, intact abduction, external rotation, and internal rotation to the lumbosacral junction. Furthermore, she had difficulty with the abdominal compression test and also had a tight posterior capsule. On examination, she was motor sensory intact distally and did not have any focal motor sensory deficits. She reported mild discomfort with deep palpation of the long head of the biceps tendon in the bicipital groove and experienced no crepitus with range of motion of the shoulder.
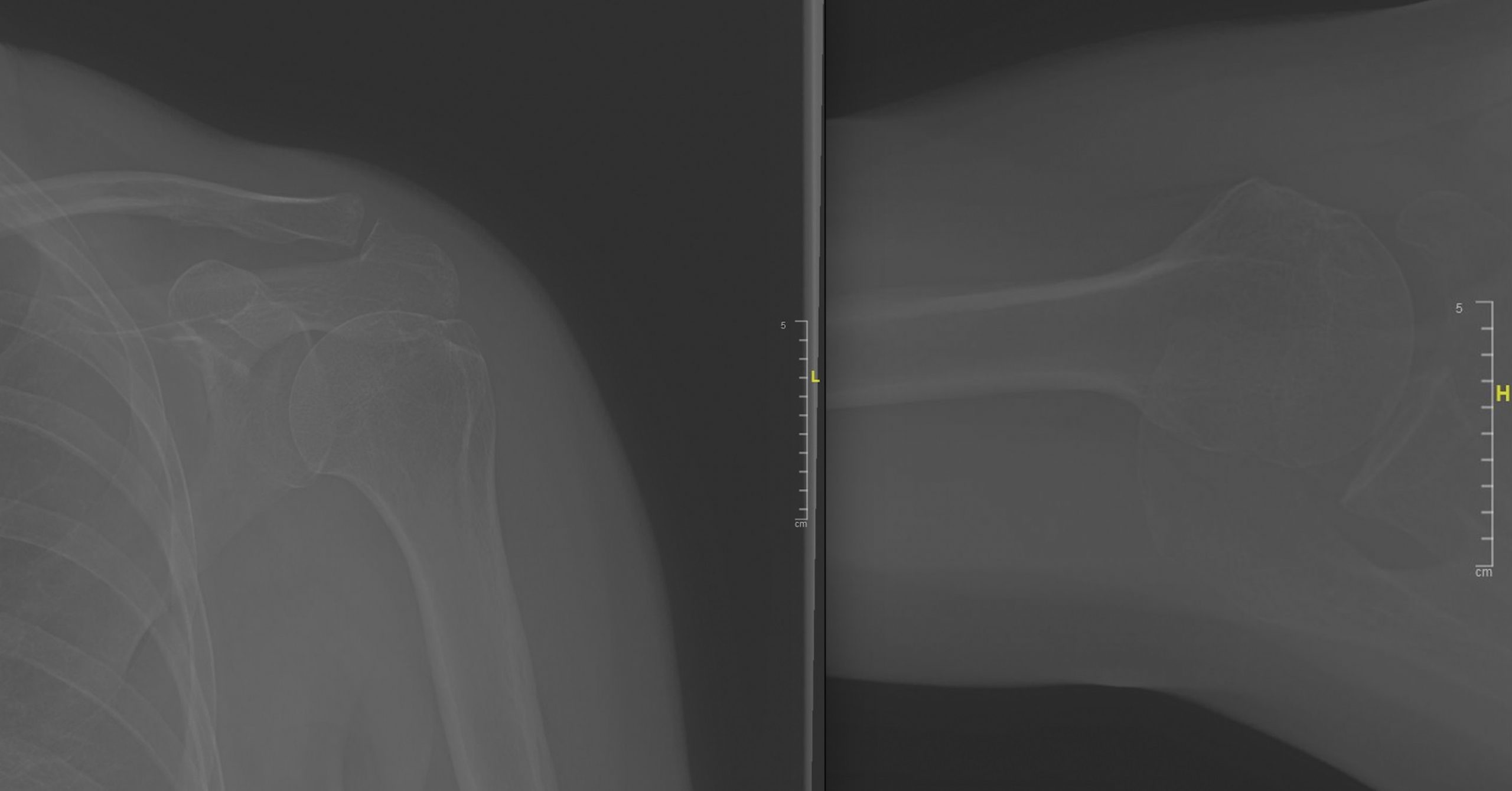
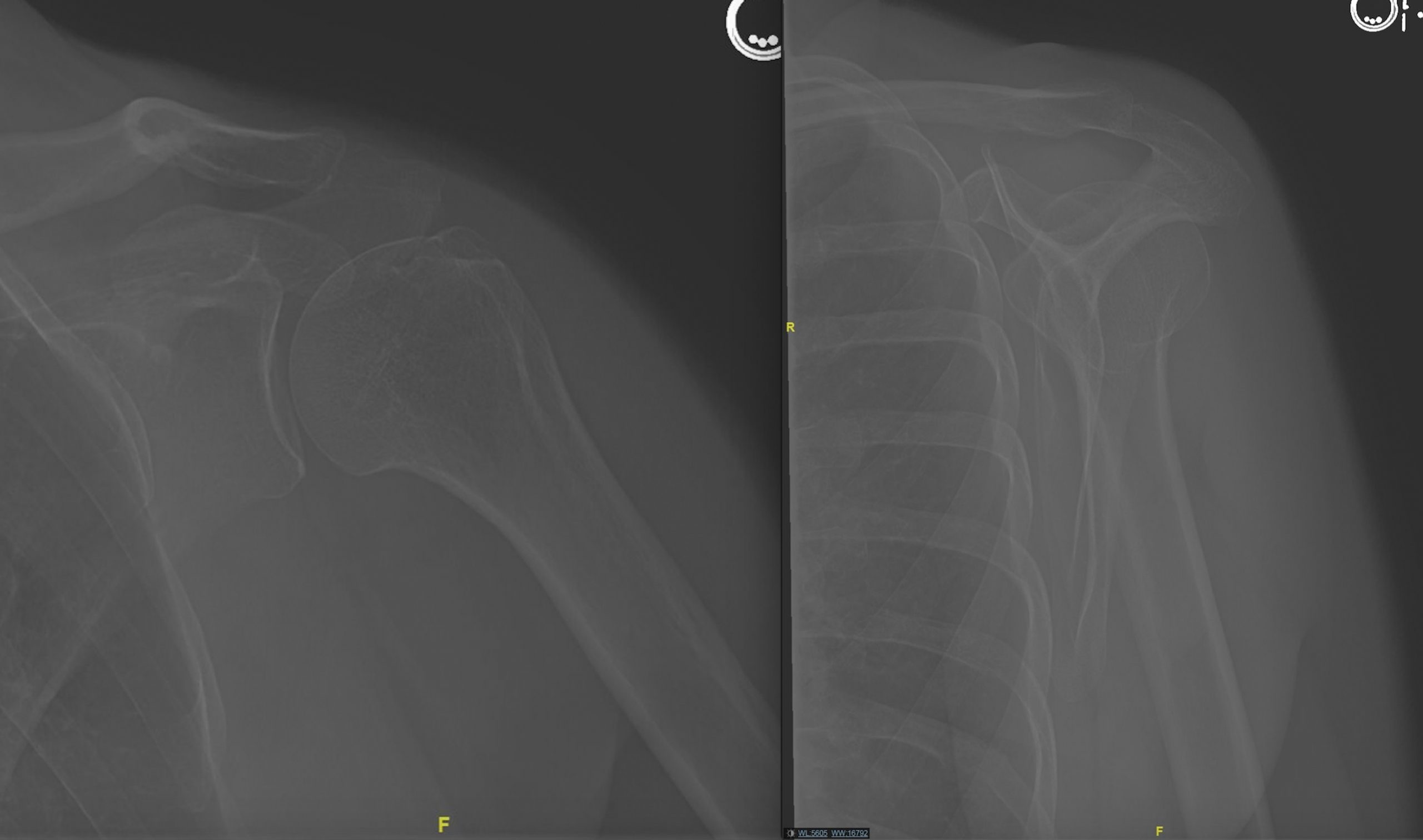
Her initial radiographs, taken at the initial clinic visit, demonstrated mild arthrosis of the acromioclavicular joint (Figs. 1 and 2). Her magnetic resonance imaging (MRI) scans, which were performed at another institution about 2 weeks before presentation at our institution, are shown in Figures 3 through 8.
The clinical and imaging findings were interpreted as Cruess stage-II osteonecrosis (avascular necrosis).
We discussed nonoperative treatment options with the patient including observation, physical therapy, nonsteroidal anti-inflammatory medications, and corticosteroid injection. We also discussed operative options, including arthroscopically assisted core decompression and subchondroplasty, and the natural history of the disease process, outlining the resurfacing and arthroplasty options for the treatment of post-collapse avascular necrosis. The patient was ultimately given a localized intra-articular corticosteroid injection as a first-line therapy for the pain, as well as for the diagnostic purpose of confirming the source of pain.
On follow-up, the patient reported that the treatment led to relief of 90% of the initial pain. Post-treatment physical examination revealed 160° of active forward elevation and 75° of adducted external rotation and internal rotation to the lumbosacral junction. At the 18-month follow-up, the patient had pain relief and full range of motion of the shoulder with 160° active forward elevation and 60° of adducted external rotation and internal rotation to the thoracolumbar junction. Her 1-year follow-up radiographs demonstrated unchanged mild arthrosis of the acromioclavicular joint and unchanged cortical irregularity of the central portion of the humeral head (Figs. 9 and 10). At the last follow-up, she continued to take the methylated supplements and maintained strict dietary restrictions, which decreased the inflammation and pain.
Proceed to Discussion >>Reference: Shakir I, Kim A, Salazar D. Avascular necrosis of the humeral head in a patient with methylenetetrahydrofolate reductase 1 gene polymorphism: a case report. JBJS Case Connect. 2020 Jul-Sep;10(3):e19.00486.
Nontraumatic osteonecrosis is an uncommon and challenging disease; thus, a proper knowledge of treatment is needed. To predict disease progression, severity, appropriate intervention, and outcomes, radiographic staging and measurement of lesion size are used. The most commonly used staging system for shoulder osteonecrosis is that of Cruess. Core decompression, resurfacing, and hemiarthroplasty are safe and effective treatments for low-grade to medium-grade osteonecrosis of the humeral head, whereas total shoulder arthroplasty seems to offer better outcomes for high-grade osteonecrosis of the humeral head. The etiology of osteonecrosis of the humeral head is hypothesized to be the disruption of the delicate blood supply to the proximal humeral head, although the exact blood supply is controversial.
Consistent with a Creuss Stage-II lesion, the initial radiographs demonstrated only subtle subchondral irregularities of the humeral head, with maintained sphericity and no evidence of collapse. The patient’s MRI scans revealed osteonecrosis (avascular necrosis) of the humeral head as the etiology of the shoulder symptoms.
We hypothesized that this patient developed hyperhomocysteinemia due to MTHFR C677T polymorphism, which contributed to the development of osteonecrosis of the humeral head. A search using the MEDLINE/PubMed database was conducted using the search terms “methylenetetrahydrofolate reductase polymorphism AND osteonecrosis OR avascular necrosis.” Although previous evidence linked hyperhomocysteinemia with impaired vascular function and circulation, a large study by Bezemer et al. showed no association between this polymorphism and risk of venous thrombosis, and 3 other studies, one of them a meta-analysis, demonstrated no association between MTHFR polymorphisms and osteonecrosis of the femoral head. However, in the absence of other risk factors and clear etiology, we believe that this is a rare case in which hyperhomocysteinemia due to MTHFR polymorphism may have contributed to osteonecrosis of the humeral head via mechanisms other than venous thrombosis.
The heterozygous C677T MTHFR polymorphism in our patient caused methylation of homocysteine to methionine to be reduced, possibly leading to the development of hyperhomocysteinemia. Clark et al. reported that approximately 12% were homozygous for this polymorphism, indicating a relatively high frequency. Hyperhomocysteinemia is closely associated with an increased risk for a number of adverse outcomes and disease states including higher 5-year mortality in type-2 diabetes, diabetic retinopathy, dyslipidemia, ischemic stroke, and Lichtheim disease. It is important to note that, despite our patient’s history of hyperhomocysteinemia, we did not check her homocysteine levels because they would not have changed our clinical management of osteonecrosis of the humeral head.
Hyperhomocysteinemia may cause oxidative damage to endothelial cells and, therefore, impair vascular circulation. A secondary mechanism by which hyperhomocysteinemia may contribute to the onset of osteonecrosis of the humeral head is through direct reductions in bone strength and density via oxidative stress and disruption of collagen cross-linking. In addition, continuous or intermittent fat emboli caused by increased serum lipids and increased intraosseous pressure because of increased subchondral fat storage may also lead to osteonecrosis of the humeral head. Ultimately, all of these mechanisms lead to a common pathway via compromised circulation to the subchondral bone and subsequent ischemia and necrosis.
Limitations of this case report included a lack of generalizability to the general public and the lack of an established cause-effect relationship between the genetic polymorphism and the onset of the osteonecrosis of the humeral head. In assessing our management of this case, we believe that it would have been beneficial to quantify serum homocysteine over a period of time, possibly to reveal any association between homocysteine levels and symptomatic severity of osteonecrosis of the humeral head. The lack of quantifiable laboratory values for homocysteine was a major limitation of our case report.
We believe that this case represents an unusual presentation of osteonecrosis of the humeral head. Further study is needed to confirm this link between the C667T polymorphism and development of osteonecrosis of the humeral head, as well as into the role of hypercholesteremia in osteonecrosis of the humeral head. In this case example, we believe that the MTHFR polymorphism played a role in the development of osteonecrosis of the humeral head through elevated homocysteine. We conclude that in the absence of other risk factors and after other, more likely diagnoses have been excluded, osteonecrosis of the humeral head in the context of a MTHFR polymorphism and hyperhomocysteinemia could be considered a possible cause of atypical shoulder pain.
Reference: Shakir I, Kim A, Salazar D. Avascular necrosis of the humeral head in a patient with methylenetetrahydrofolate reductase 1 gene polymorphism: a case report. JBJS Case Connect. 2020 Jul-Sep;10(3):e19.00486.
What is the diagnosis?
Aneurysmal bone cyst
Cartilage neoplasm, probably low grade
Osteonecrosis (avascular necrosis)
Probable hydroxyapatite deposition (Milwaukee shoulder syndrome)
Multiple bone islands (enostoses)

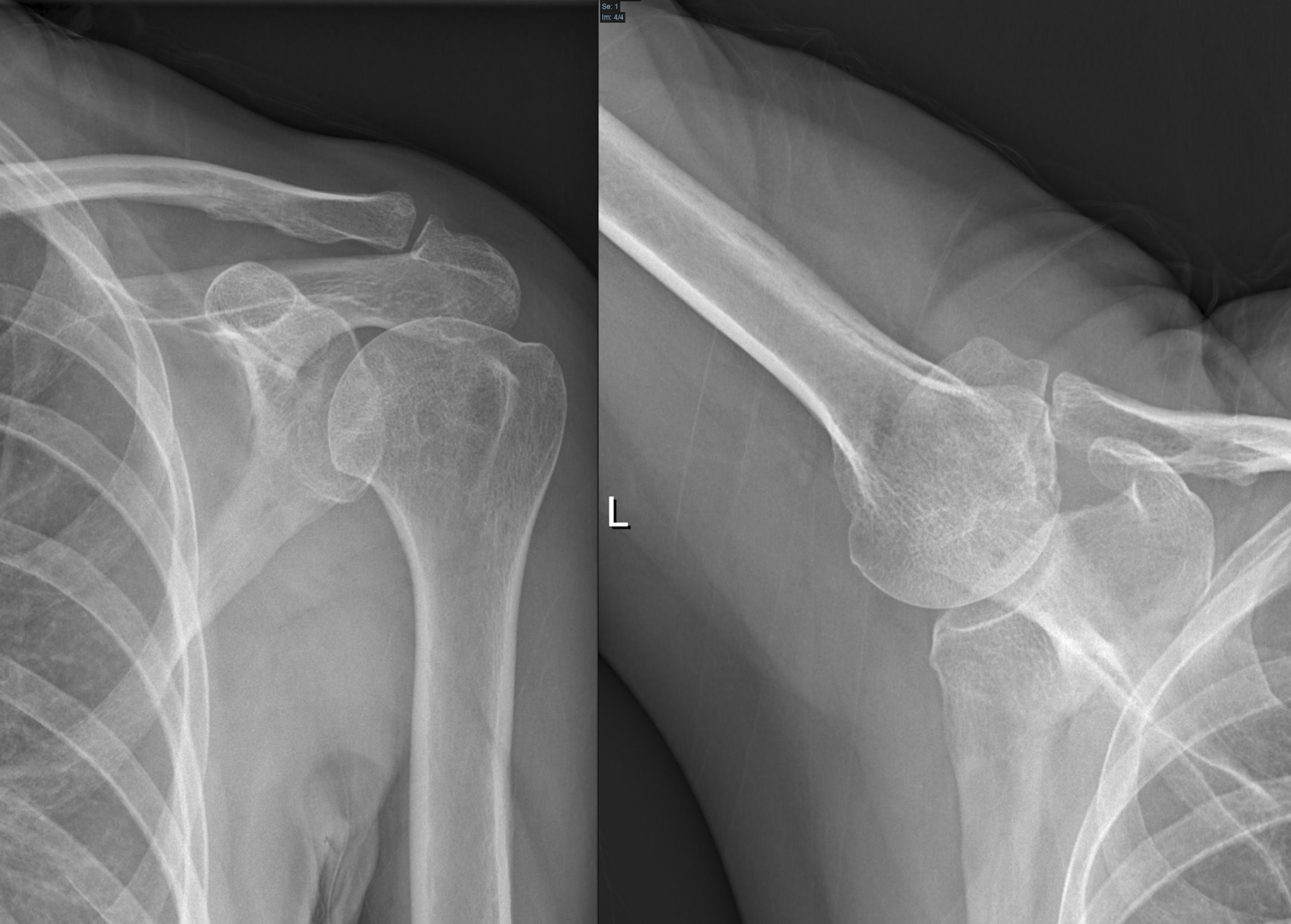




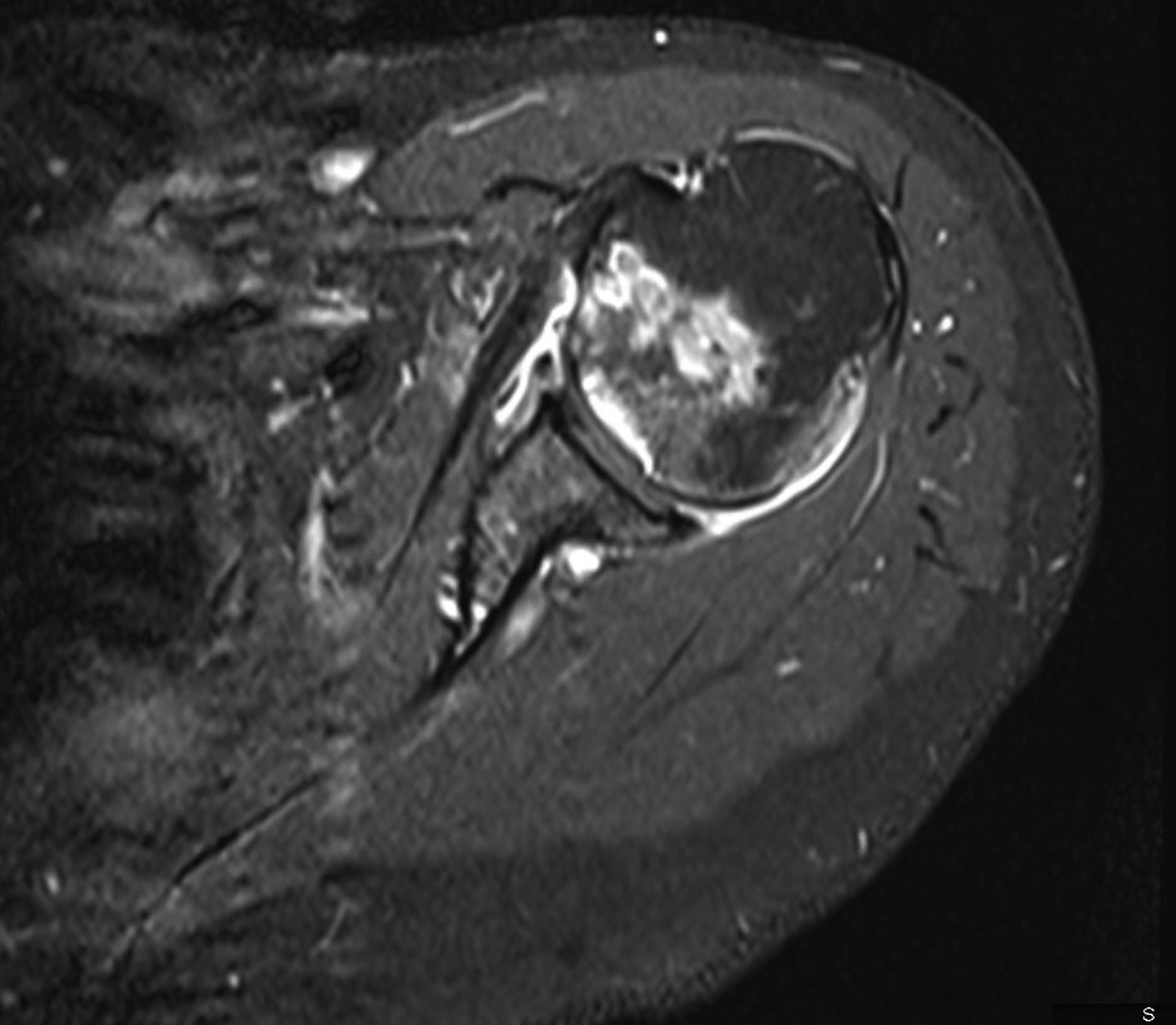
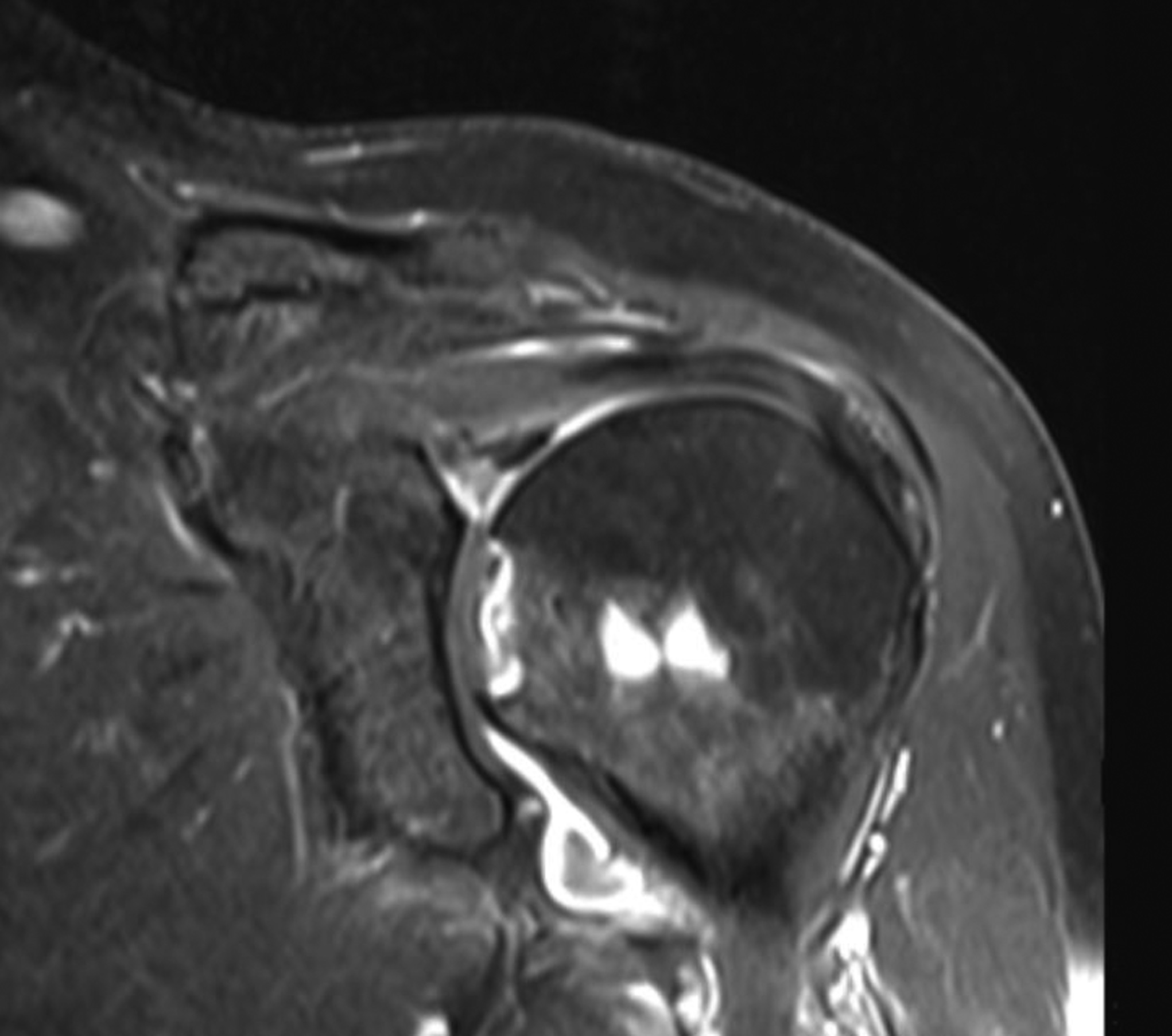
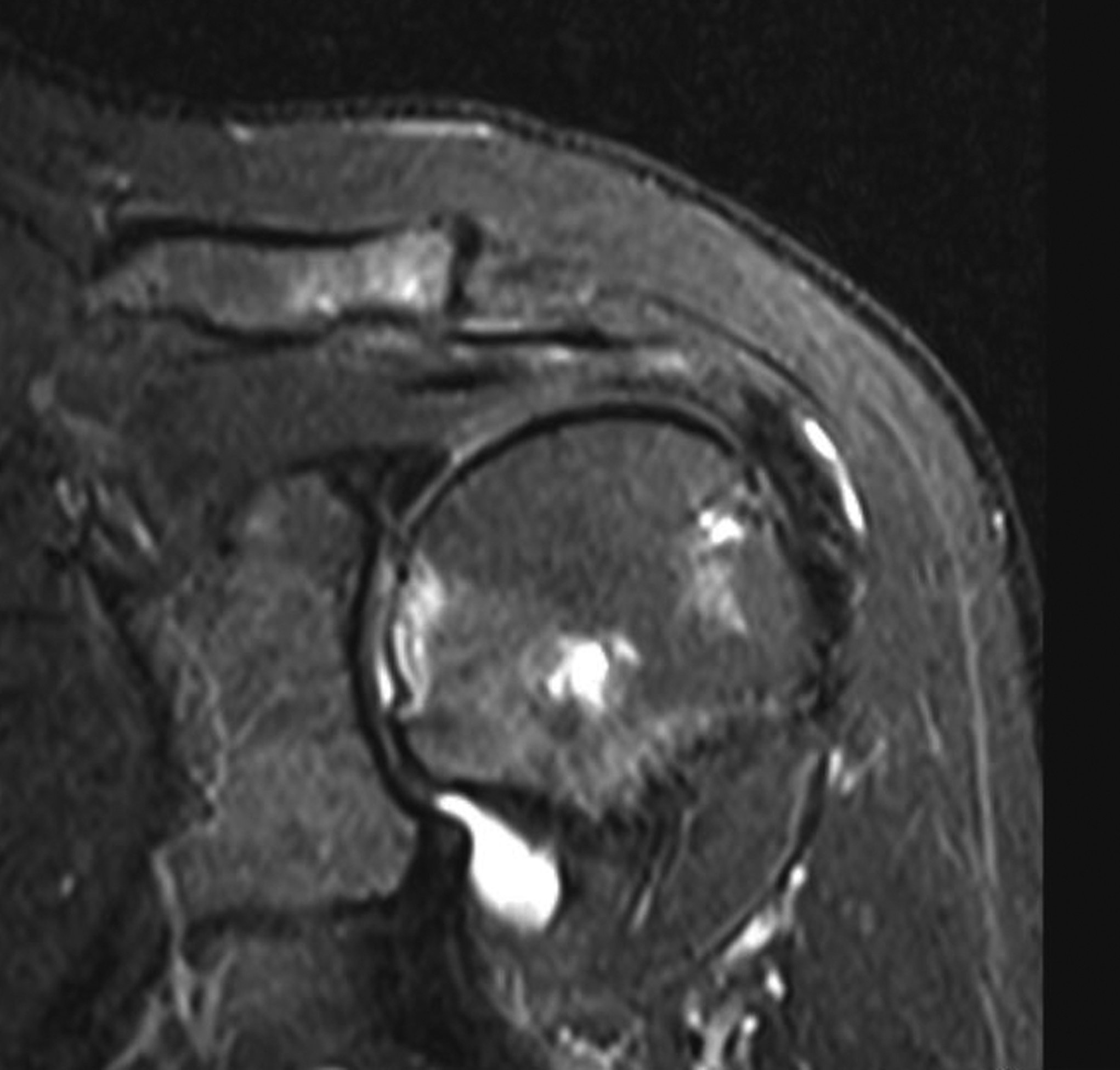
 Fig. 1
Fig. 1 Fig. 2
Fig. 2 Fig. 3
Fig. 3 Fig. 4
Fig. 4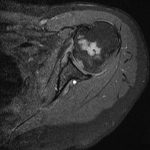 Fig. 5
Fig. 5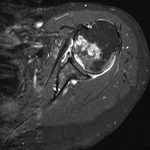 Fig. 6
Fig. 6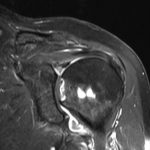 Fig. 7
Fig. 7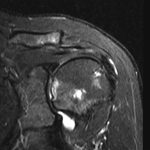 Fig. 8
Fig. 8 Fig. 9
Fig. 9 Fig. 10
Fig. 10