A 60-Year-Old Man with a Mass Following Hip Surgery
September 2, 2020
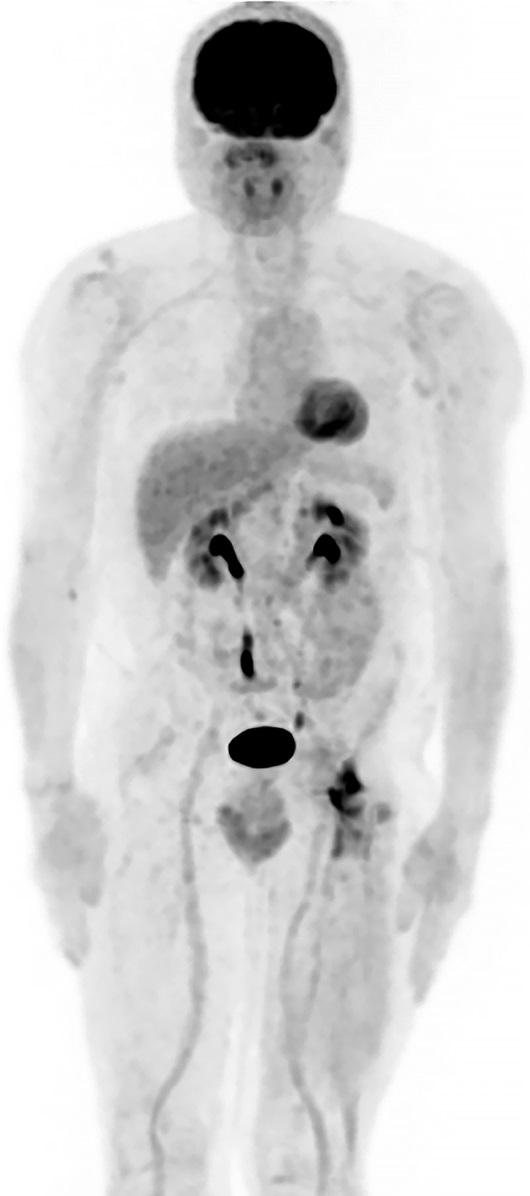
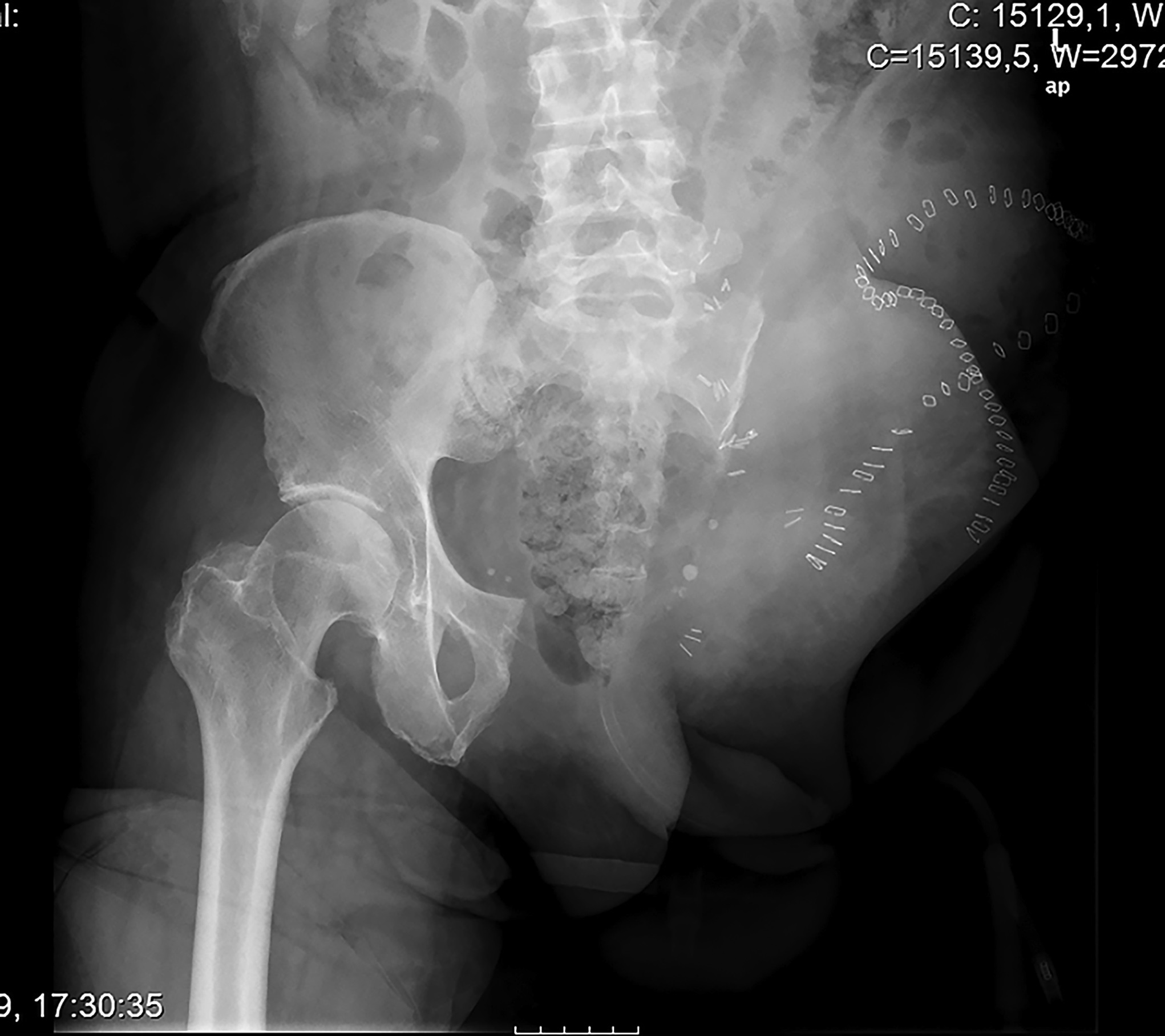
A 60-year-old man, with no relevant medical history, underwent total hip arthroplasty at another institution for left hip pain that was interpreted as hip arthritis (Figs. 1-A and 1-B). During the surgical procedure, the orthopaedic surgeon noted an abnormal mass in the medial aspect of the proximal part of the left femur. At this point, the femoral neck osteotomy had already been performed and the acetabular cup had been implanted. In addition, no mass was visualized in the femoral canal. After identification of the proximal femoral mass, a biopsy was obtained. No frozen section was performed, and the decision was made to finish the total hip replacement (THR) (Fig. 2). After the patient was discharged, a referral was made to our institution.
The patient was admitted to our institution, where bone scintigraphy, hip computed tomography (CT) (Fig. 3-A), and hip magnetic resonance imaging (MRI) (Fig. 3-B) were obtained. No evidence of distant disease was discovered. A wide proximal femoral resection was performed with reconstruction (Fig. 4) with a proximal femoral arthroplasty, maintaining the original acetabular cup (Fig. 5).
The surgical specimen was submitted to pathology (Figs. 6-A and 6-B).
The imaging results and histology illustrate a grade-2 chondrosarcoma.
Unfortunately, sacrifice of the femoral nerve was necessary because it was encased within the mass. During the postoperative period, there were no additional complications and the patient’s recovery was straightforward. However, after these procedures, the patient needed permanent assistance with crutches for walking because the femoral nerve injury removed all active knee extension.
The margins of resection were free of tumor, but after 2 years of postoperative follow-up, the patient developed new left hip and thigh symptoms. The staging positron emission tomography (PET)-CT scan identified what seemed to be local recurrence of the chondrosarcoma (Fig. 7), requiring an external hemipelvectomy, which confirmed the local recurrence of a grade-2 chondrosarcoma (Fig. 8). The pathology report confirmed again a safe surgical margin with an R-0 resection. In addition, highly suspicious pulmonary nodules were also identified in the PET-CT. Six months after hemipelvectomy, the patient was doing well, without any pain, and was working in his old job, despite the persistent need for crutches.
Proceed to Discussion >>Reference: Soares do Brito J, Spranger A, Almeida P, Presa D, Fernandes I, Portela J. Proximal femur chondrosarcoma misdiagnosed as hip arthritis: a case report. JBJS Case Connect. 2020 Jan-Mar;10(1):e0324.
Hip arthritis is a common cause for pain and disability among older adults and a major reason for THR. In the United States, projections indicate that, by 2030, more than half a million THRs will be performed annually, the majority due to osteoarthritis. However, bone sarcomas are rare, accounting for only <0.2% of all malignant tumors.
Among primary bone tumors, chondrosarcoma is the most frequently occurring bone sarcoma of adulthood. The incidence is about 0.2/100,000 per year, with the most common age at diagnosis being between 30 and 60 years. The main feature of this neoplasm is the presence of cartilage-forming malignant cells without direct osteoid formation. It is a difficult tumor to treat, mainly because of its resistance to chemotherapy and radiotherapy. Chondrosarcomas are themselves a very rare heterogeneous group; in addition to conventional central, peripheral, and periosteal chondrosarcomas, 5 different histological subtypes are described: juxtacortical, mesenchymal, myxoid, dedifferentiated, and clear cell. This type of tumor can be categorized as primary or secondary, depending on the initial presentation as a de novo chondral malignancy, or because of a change in the biological behavior of a formerly benign chondral lesion such as an enchondroma or osteochondroma. In addition, chondrosarcomas can be classified as axial or appendicular, depending on the anatomical site where the neoplasm arises; however, almost 50% are found around the hip.
In general, the standard treatment for chondrosarcoma is surgical, but there is no consensus on the surgical margin needed for each grade of chondrosarcoma, especially for grade-1 cases. Nonetheless, most authors agree on the need for wide resection in all tumors of grades 2 and 3. The prognosis depends on the histological grade, but the histological classification is often subjective and there is a wide spectrum of outcomes. Not even grade-1 tumors have a 100% survival rate, mainly because of local recurrence or progression to a higher grade on recurrence. Inoperable, locally advanced, and metastatic high-grade chondrosarcomas—particularly, dedifferentiated chondrosarcomas—have a poor prognosis.
Medical textbooks always include tumors as a differential diagnosis for hip pain, but malignant disease is still a rare finding. Although the proximal part of the femur and pelvis are common sites for cartilaginous neoplasms, hip osteoarthritis is a much more frequent diagnosis. However, some case reports have described malignant neoplasms that mimic arthritis or even benign bone tumors. Therefore, primary malignant disease should be kept in mind as a possible diagnosis for any patient with hip symptoms, especially when imaging studies are not typical for hip osteoarthritis.
Radiographs in this case lacked the usual sclerosis, erosions, and osteophytosis that are usually present in osteoarthritis (Fig. 1). In addition, there were suspicious calcifications medial to the proximal segment of the femoral bone. In this scenario, we should point out that radiographs in the pelvic area are more difficult to read because of the anatomy of the overlying structures. Therefore, in the absence of typical and characteristic findings for arthritis, physical examination, and additional imaging studies may be needed to exclude malignancy, including primary bone tumors or metastatic diseases.
Patients with a chondrosarcoma diagnosis should be further evaluated for complete staging as early as possible. Surgical treatment is the optimal choice for all patients, particularly for those who can undergo complete resection with acceptable morbidity. In our case, after the biopsy revealed a grade-2 chondrosarcoma, we had to perform a wide surgical excision of the proximal femur, but this approach included the serious complication of femoral nerve sacrifice. The previous surgical procedure made our surgical resection more difficult. We were able to achieve complete excision with negative margins, but the patient experienced local recurrence 2 years later, leading to external hemipelvectomy.
The high morbidity and mortality related with bone sarcomas demand a correct diagnosis. As such, it is important to stress the need of considering other diagnoses for hip pain rather than the usual arthritis. A high index of suspicion is needed at all times to achieve a proper diagnosis in these rare cases to avoid compromising the patient’s oncologic outcome.
Reference: Soares do Brito J, Spranger A, Almeida P, Presa D, Fernandes I, Portela J. Proximal femur chondrosarcoma misdiagnosed as hip arthritis: a case report. JBJS Case Connect. 2020 Jan-Mar;10(1):e0324.
What is the diagnosis?
Chondromyxoid fibroma
Chordoma
Chondrosarcoma
Chondroblastic osteosarcoma
Chondroid syringoma


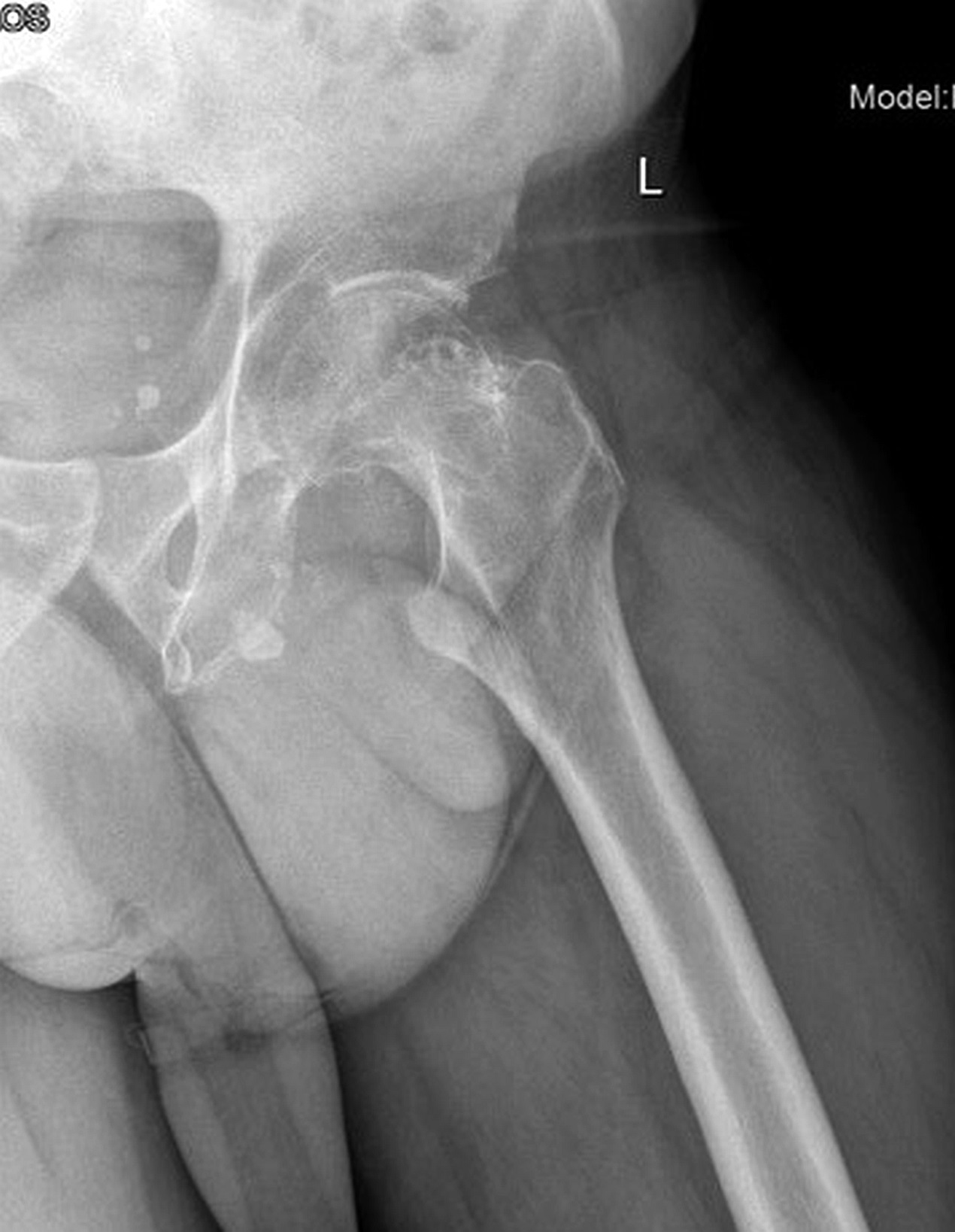

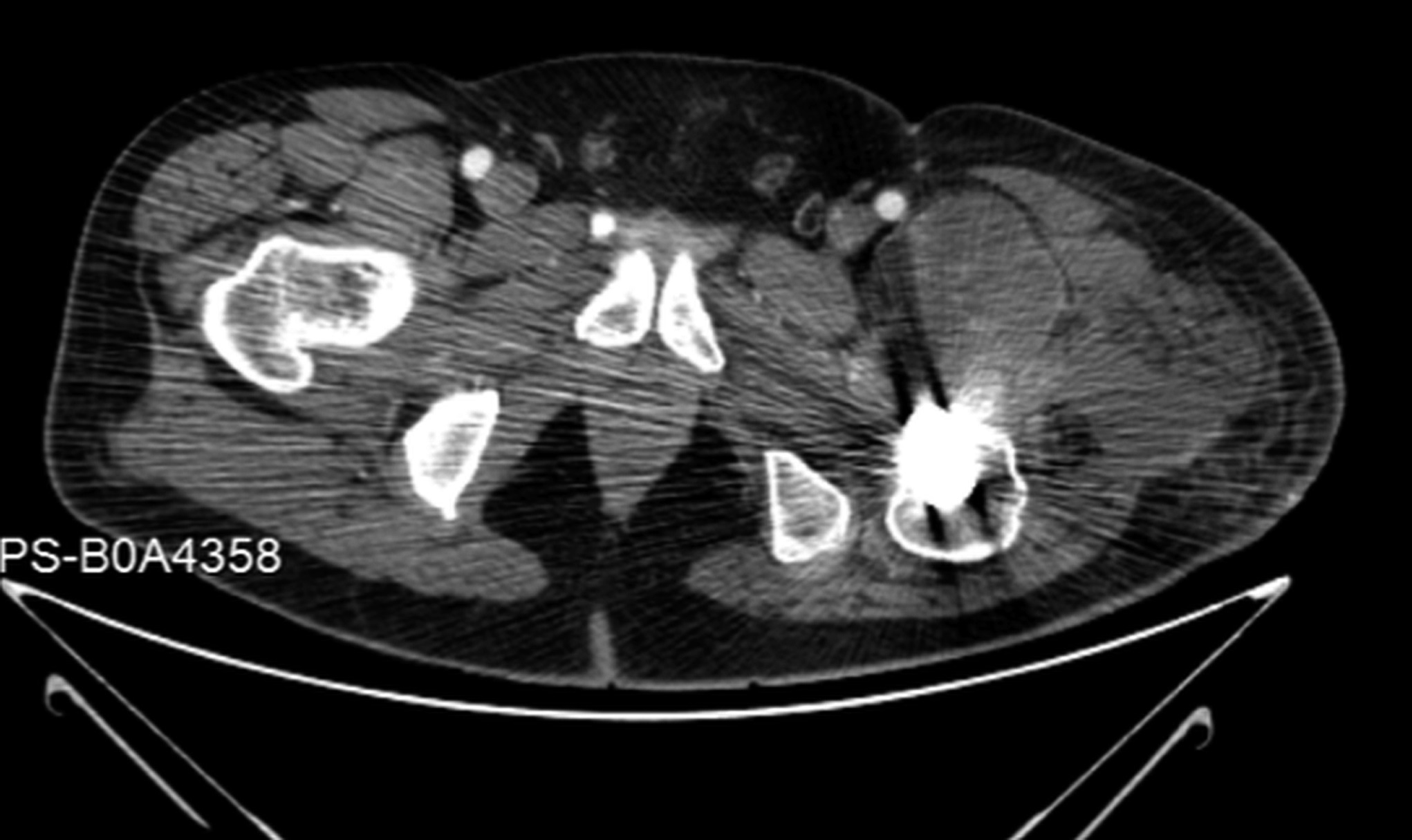
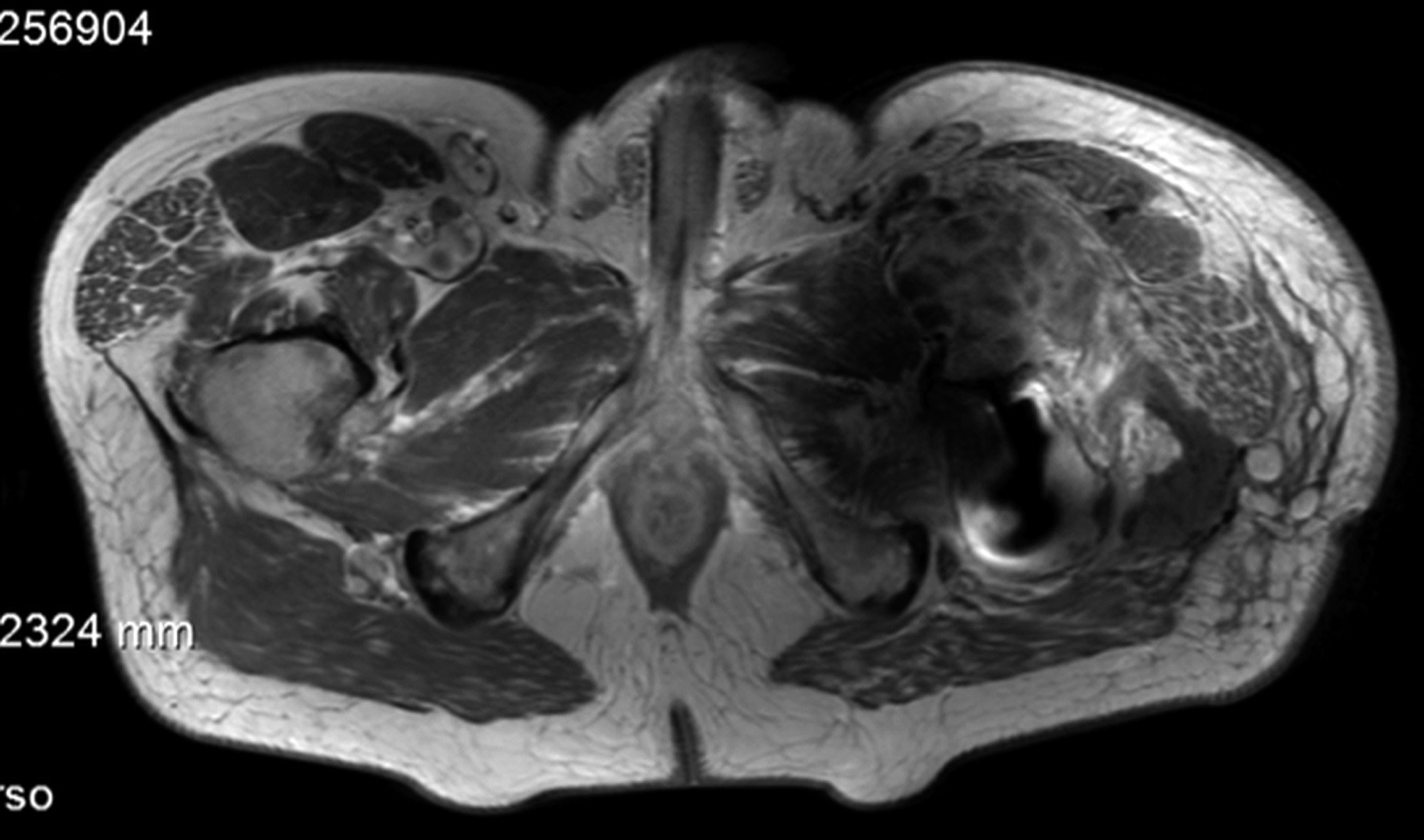


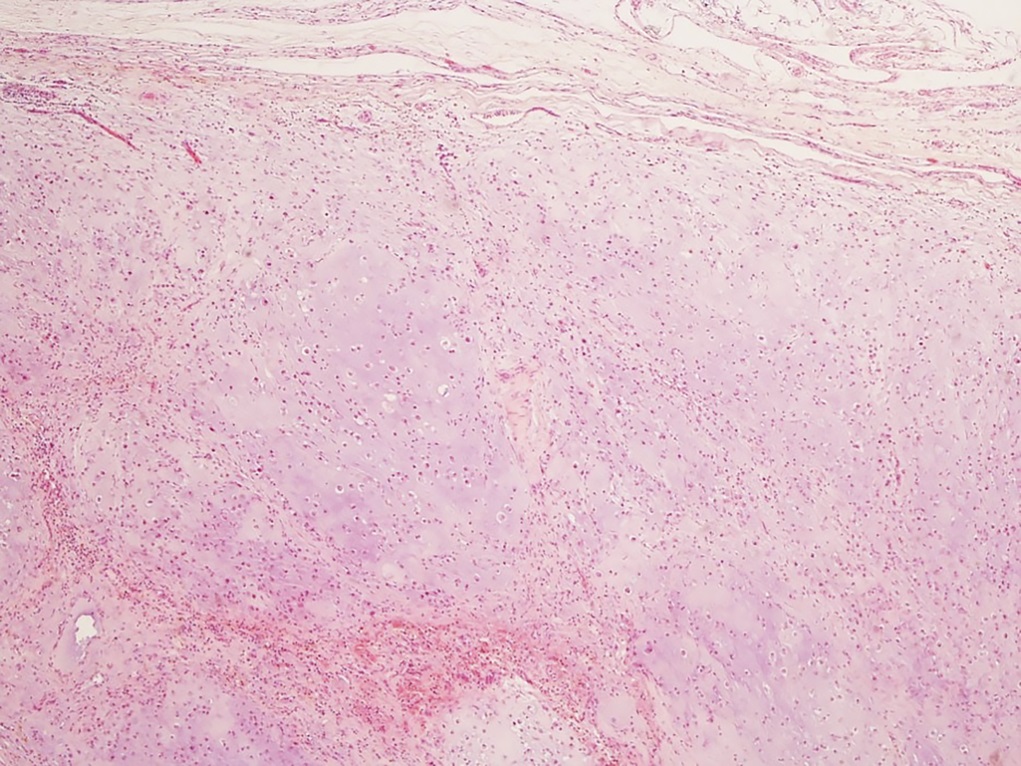

 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2
Fig. 2 Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 4
Fig. 4 Fig. 5
Fig. 5 Fig. 6-A
Fig. 6-A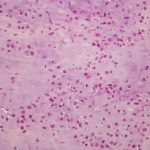 Fig. 6-B
Fig. 6-B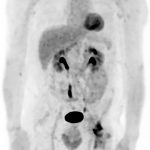 Fig. 7
Fig. 7 Fig. 8
Fig. 8