A 64-year-old active warehouse worker presented for an evaluation of progressive medial left knee pain. The pain that he experienced was refractory to conservative care including physical therapy, nonsteroidal anti-inflammatory drugs, and activity modification. On physical examination, he demonstrated passively correctable genu varum, passive range of motion from 0° to 120°, and tenderness to palpation of the anteromedial joint line. His cruciate ligament examination was normal. Radiographs (Figs. 1-A and 1-B) were consistent with isolated medial compartment osteoarthritis. Stress radiographs performed with a valgus force demonstrated a complete correction of the varus deformity. Given that the patient had isolated medial compartment osteoarthritis, passively correctable varus deformity, and an inability to obtain satisfactory pain relief with conservative care, he elected to proceed with a unicompartmental knee arthroplasty (UKA). The surgical procedure was performed with Mako robotic-arm assistance and Restoris multicompartmental knee partial knee replacement (Stryker).
A mini-medial parapatellar arthrotomy was used and intraoperative inspection of the patellofemoral and lateral compartments confirmed healthy chondral surfaces and intact lateral meniscal and cruciate ligaments. Postoperative radiographs demonstrated a well-positioned unicompartmental replacement without fracture (Fig. 2-A and 2-B). The patient was allowed to bear weight as tolerated on postoperative day 1 with the guidance of the physical therapist and was discharged without incident. At his first postoperative visit (postoperative day 27), the patient had minimal pain and demonstrated a well-healed incision and range of motion of 0° to 115°.
On postoperative day 42, the patient presented with acute-onset lateral knee pain and popping after feeling an acute pop while walking backwards in physical therapy. Later that evening when stepping down to get out of bed, this pain acutely worsened, and the patient had substantial difficulty with ambulation. On physical examination, he walked with an antalgic gait without evidence of swelling or erythema. His range of motion was maintained at 0° to 115°. He described tenderness to palpation on the lateral side of the knee deep to the iliotibial band just distal to the lateral femoral epicondyle. There was no asymmetric laxity to varus stress at 0° or 30° of flexion or increased external tibial rotation on dial testing.
Given the nonspecific findings on physical examination, the patient was advised to continue his normal activities within the limitations associated with the UKA. Physical therapy was prescribed, and the patient used topical diclofenac gel but did not obtain any sustained relief. Subsequent radiographic evaluation demonstrated an ill-defined ossific density over the lateral epicondyle, which was not present preoperatively or on immediate postoperative radiographs (Fig. 3-A). Conservative care was initiated, including 8 weeks of physical therapy and an intra-articular corticosteroid injection for the treatment of synovitis and suspected lateral meniscal tear, and a magnetic resonance imaging (MRI) study was performed to better characterize the ossific fragment and status of the lateral meniscus. Although the patient experienced temporary, partial improvement after the corticosteroid injection, symptoms quickly recurred.
The MRI scans are shown in Figures 3-B and 3-C. A diagnostic injection of 5-mL 1% lidocaine was performed at the location identified by maximal tenderness of examination, distal to the palpable lateral epicondyle. After 5 minutes, the patient had no further tenderness and had restoration of normal gait with pain relief. After a thorough discussion, the patient elected to proceed with excision of the fragment.
Radiographic imaging studies and temporary pain relief after lidocaine injection led to the patient being diagnosed with avulsion fracture of the popliteal tendon.
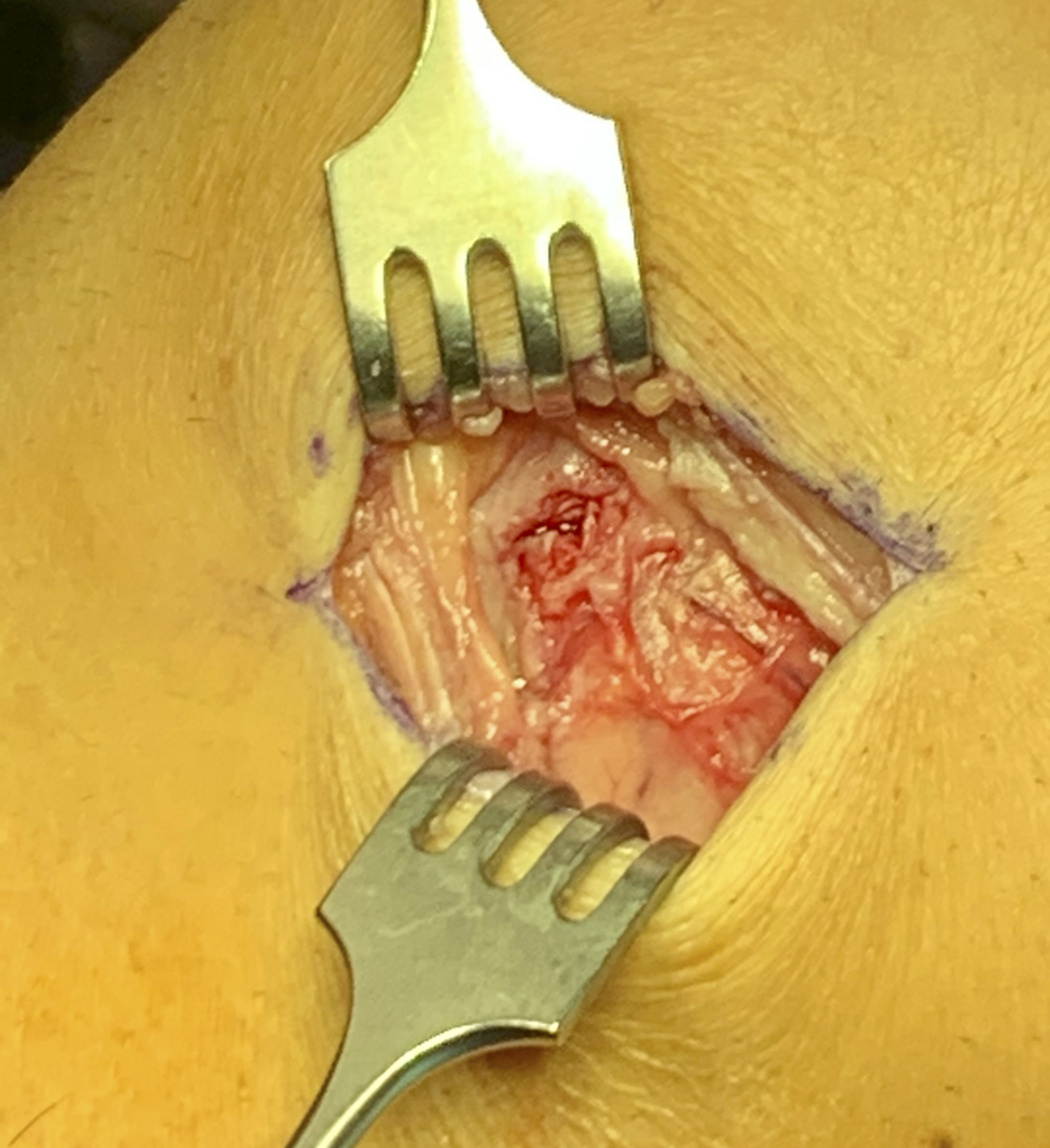
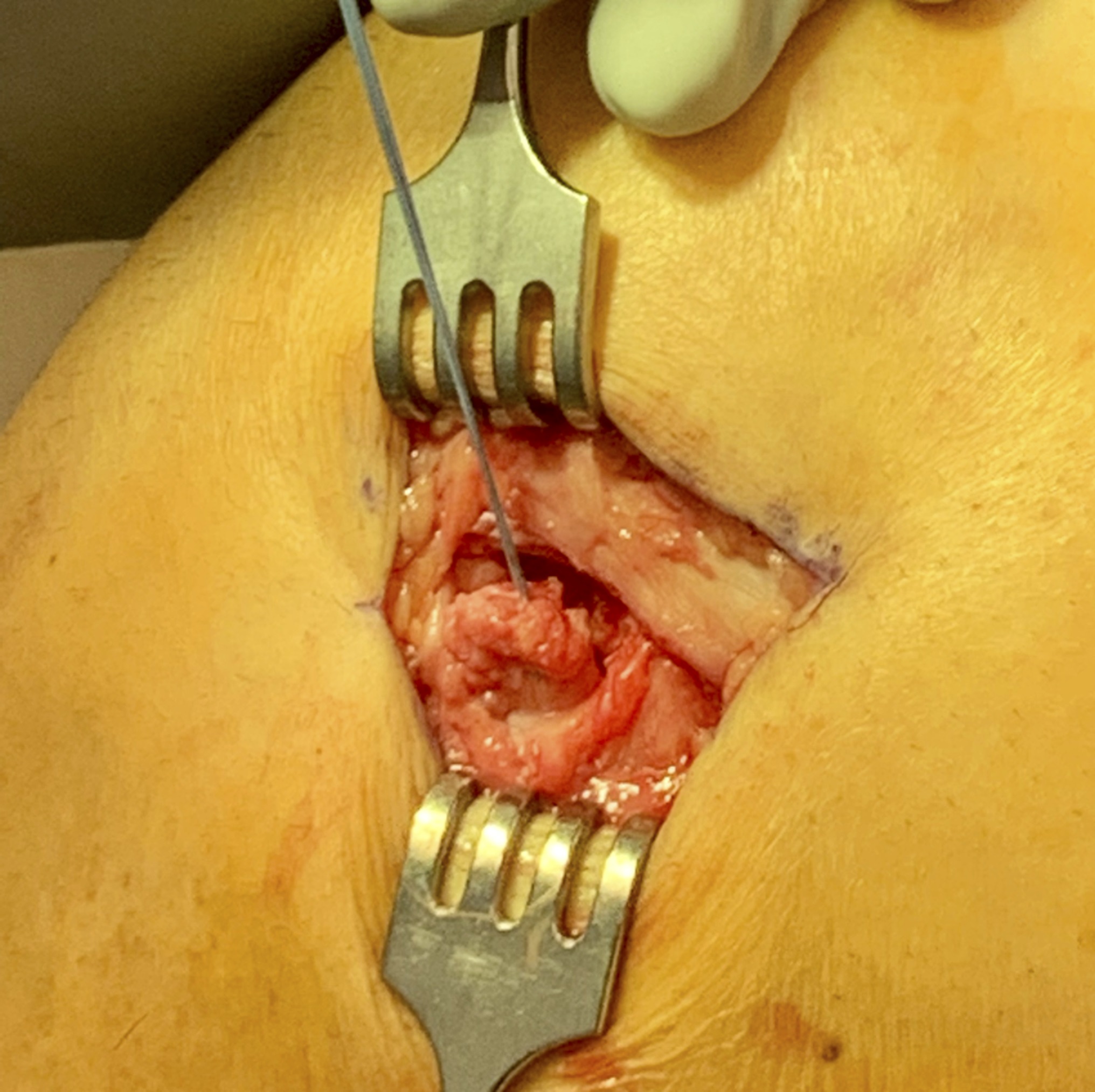
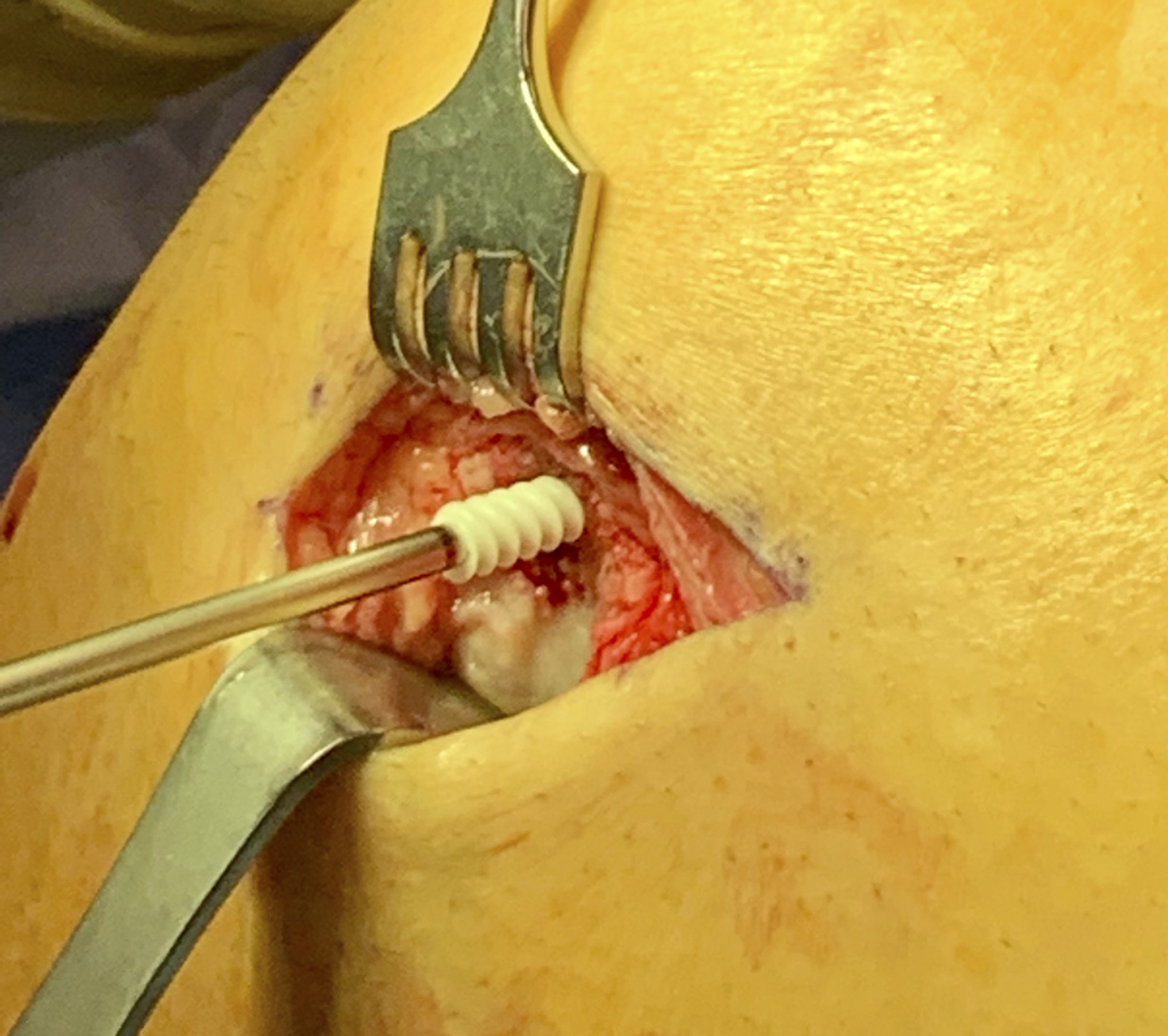
On the date of surgical procedure, 5 months after the initial UKA, the location of the lateral knee tenderness that the patient was experiencing was localized and marked in the preoperative holding area. The patient was positioned in the supine position, and a nonsterile tourniquet was applied to the operatively treated extremity. A 4-cm incision was made along the lateral aspect of the knee over the previously noted location of the symptoms that the patient was experiencing (Figs. 4-A through 4-E). Sharp dissection was carried to the iliotibial band, which was split in line with the incision. The popliteal tendon was identified within the popliteal hiatus. Partial-thickness tearing of the popliteal tendon at the location of the ossific fragment was noted. The tendon was sharply dissected from the femoral insertion site because the piece of bone was believed to be too small to accommodate any fixation implants. A traction stitch was placed in the popliteal tendon to allow for appropriate manipulation of the tendon. A single 5.5-mm biocomposite suture anchor (Corkscrew, Arthrex), preloaded with 2 multistrand, ultrahigh-molecular-weight, polyethylene, flat-braided sutures (SutureTape, Arthrex), was placed at the insertion site of the native popliteal tendon. Using 1 free limb of both flat-braided sutures and a free needle, a Krackow stitch was placed into the tendon from proximal to distal. The 2 sutures were then tied to each other. With the knee flexed to 45° and at neutral rotation, maximal tension was applied to the opposite free ends of the sutures that were pulled through the anchor, which reduced the free end of the popliteal tendon to its native footprint. The tendon was secured with 5 alternating half-hitch knots between the 2 sutures. The fixation was noted to be excellent with knee flexion, extension, and rotation. The wound was irrigated and the incision was closed in layers.
The patient was placed in a hinged knee brace that was locked in extension. At his first postoperative visit (postoperative day 13), the patient’s hinged knee brace was unlocked from 0° to 40°, with the range of motion increased by 10° per week. Varus stress, hyperextension, and external tibial rotation were not allowed for 6 weeks. The patient returned to light ambulatory work in a factory at 6 weeks with the hinged knee brace to protect the repair. At 12 weeks, he was able to work without restrictions and experienced complete pain relief. At 6 months postoperatively, the patient was able to return to pickleball without recurrence of pain or symptoms.
Proceed to Discussion >>Reference: Inclan PM, Barrack RL, Matava MJ. Popliteus avulsion fracture after unicompartmental arthroplasty: a case report. JBJS Case Connect. 2023 Jan 6;13(1).e22.00477.
We identified a unique cause of dissatisfaction after UKA, a popliteal avulsion fracture. In the native knee, isolated popliteal avulsion fractures represent a rare entity limited to case reports and case series and typically present in skeletally immature populations. To the best of our knowledge, no description of this injury pattern and method of treatment has been detailed in a patient who had undergone arthroplasty. The popliteus is occasionally viewed as a structure that may be released to improve gap balancing on occasion during knee arthroplasty. However, dysfunction of the popliteal tendon (i.e., subluxation) may represent a source of discomfort after arthroplasty, while routine sectioning of this tendon during knee balancing may adversely affect postoperative functional scores. This case report and prior literature indicate that disruption of the popliteal tendon, whether iatrogenic or traumatic, may negatively affect an individual’s postoperative function and patient satisfaction.
This case also illustrates the nuanced approach necessary to diagnose discomfort after arthroplasties. Although patients undergoing UKA demonstrate greater levels of postoperative satisfaction than patients undergoing total knee arthroplasty, 10% of patients are not satisfied with the function of the operatively treated knee. Patients undergoing UKA face a significantly higher rate of revision surgery than patients undergoing total knee arthroplasty, which may be partially attributed to a real or perceived contribution of the native patellofemoral and contralateral compartment to the continued discomfort that a patient is experiencing. Efforts to better identify sources of discomfort after UKA may prevent a revision surgical procedure and allow an individual to maintain the improved activity level and satisfaction associated with a successful UKA. For a patient with laterally based discomfort, popliteal tendon pathology should be considered in addition to more common etiologies: lateral meniscal tear, progressive articular cartilage degeneration, iliotibial-band dysfunction, and fibular collateral ligament sprain. In this case, a diagnostic anesthetic injection was essential to establishing the popliteal avulsion fracture as the likely source of discomfort. In this patient’s case, the timing of the discomfort and unremarkable postoperative radiographs made an intraoperative injury unlikely; therefore, this injury likely occurred secondary to a coincidental injury during the postoperative course.
The popliteal muscle originates from the posterolateral aspect of the tibia and inserts on a 0.59-cm2 footprint on the posterolateral femoral condyle. When this condition is addressed surgically, anatomic repair is required for the successful treatment of this condition. An appreciation of the relationship between the individual structures comprising the posterolateral corner is essential to an anatomic reconstruction. In this case, reattachment of the popliteal tendon was guided by the uninjured femoral attachment of the fibular collateral ligament, which originates 18.5 mm proximal and posterior to the popliteal tendon. Given that the fibular collateral ligament is intact in the case of an isolated popliteal injury, this relationship easily guides restoration of the patient’s native anatomy. In cases in which the fibular collateral ligament is not identified or is not intact, the anterior one-fifth of the popliteal sulcus can also be used to locate the native footprint of the tendon. Repairing the tendon back to its anatomic femoral insertion, rather than excise the ossific fragment, may prevent symptomatic laxity to external tibial rotation seen with traumatic injury to the popliteus.
In addition to 3-dimensional (3D) imaging to identify the fragment, diagnostic injection was able to confirm that this avulsed fragment was the cause of an individual’s residual discomfort. This case demonstrates the diligence necessary to successfully diagnose and treat the specific cause of discomfort after an uncomplicated UKA. In this patient, excision of an avulsed bone fragment and anatomic repair of the popliteal tendon resulted in complete pain relief and satisfactory physical function.
Reference: Inclan PM, Barrack RL, Matava MJ. Popliteus avulsion fracture after unicompartmental arthroplasty: a case report. JBJS Case Connect. 2023 Jan 6;13(1).e22.00477.
What is the diagnosis?
Osteochondritis dissecans of the distal femur
Heterotopic ossification
Avulsion fracture of the popliteal tendon
Dissociated, displaced polyethylene insert from the UKA
Osteocartilaginous loose body





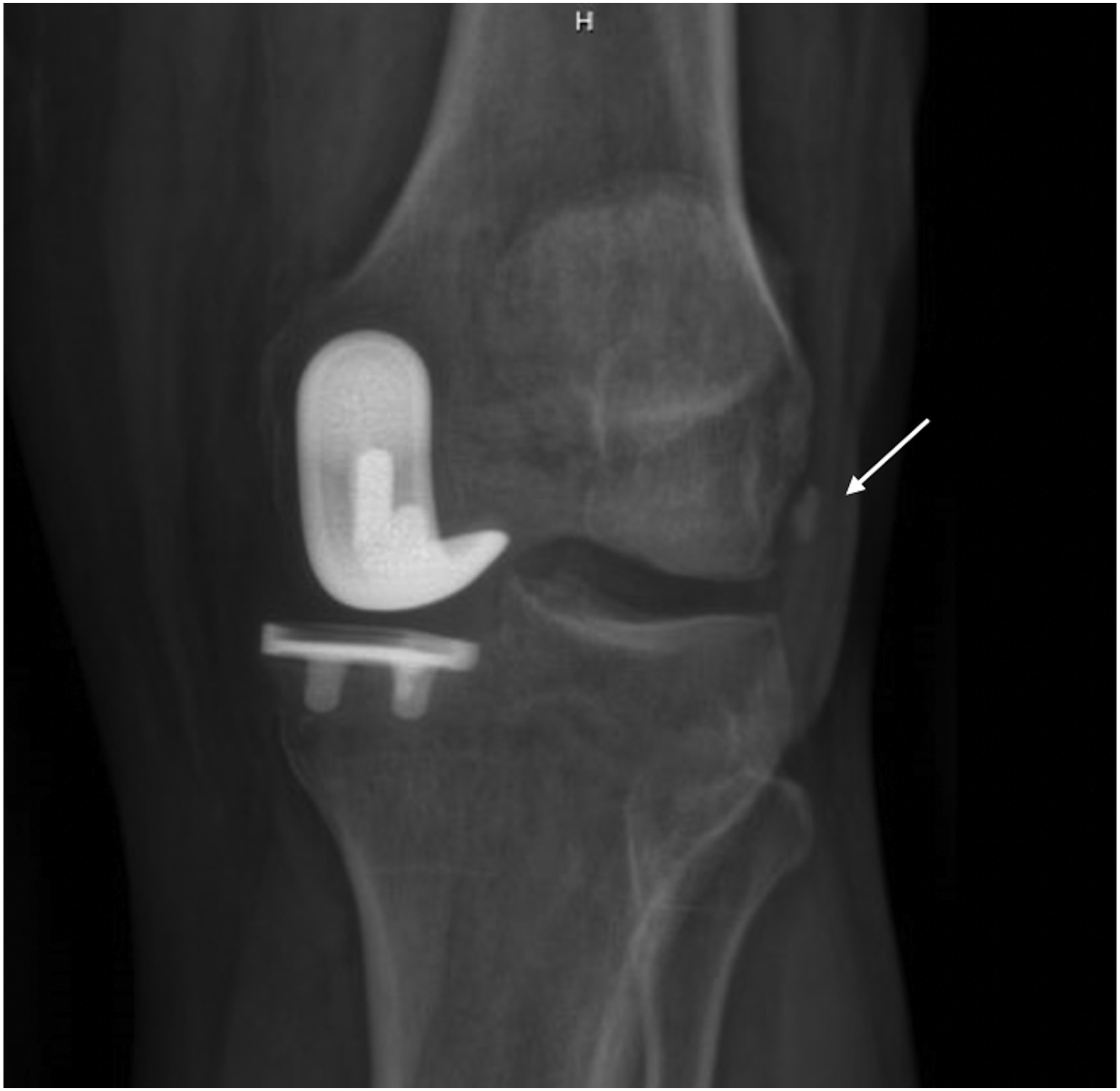
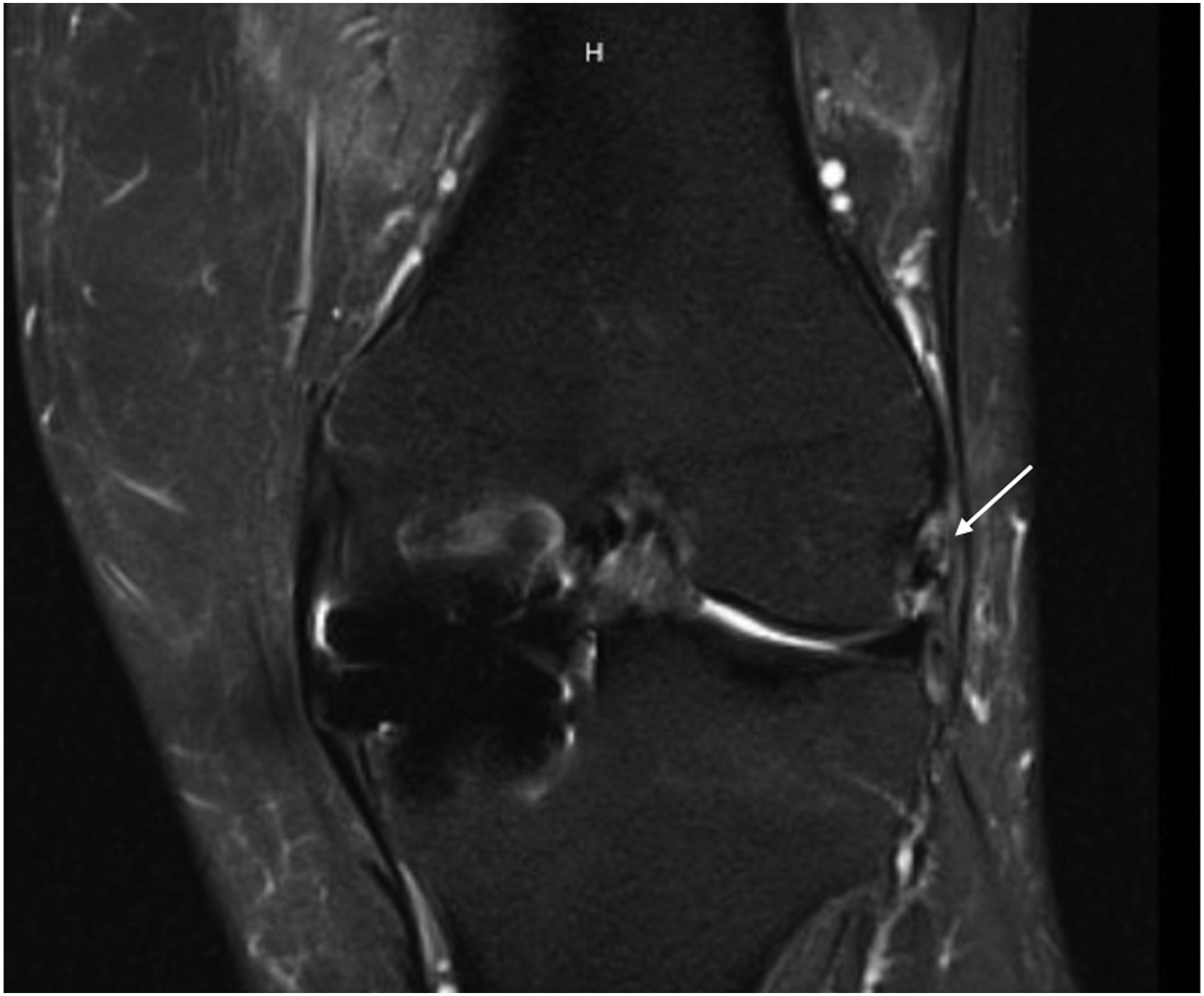
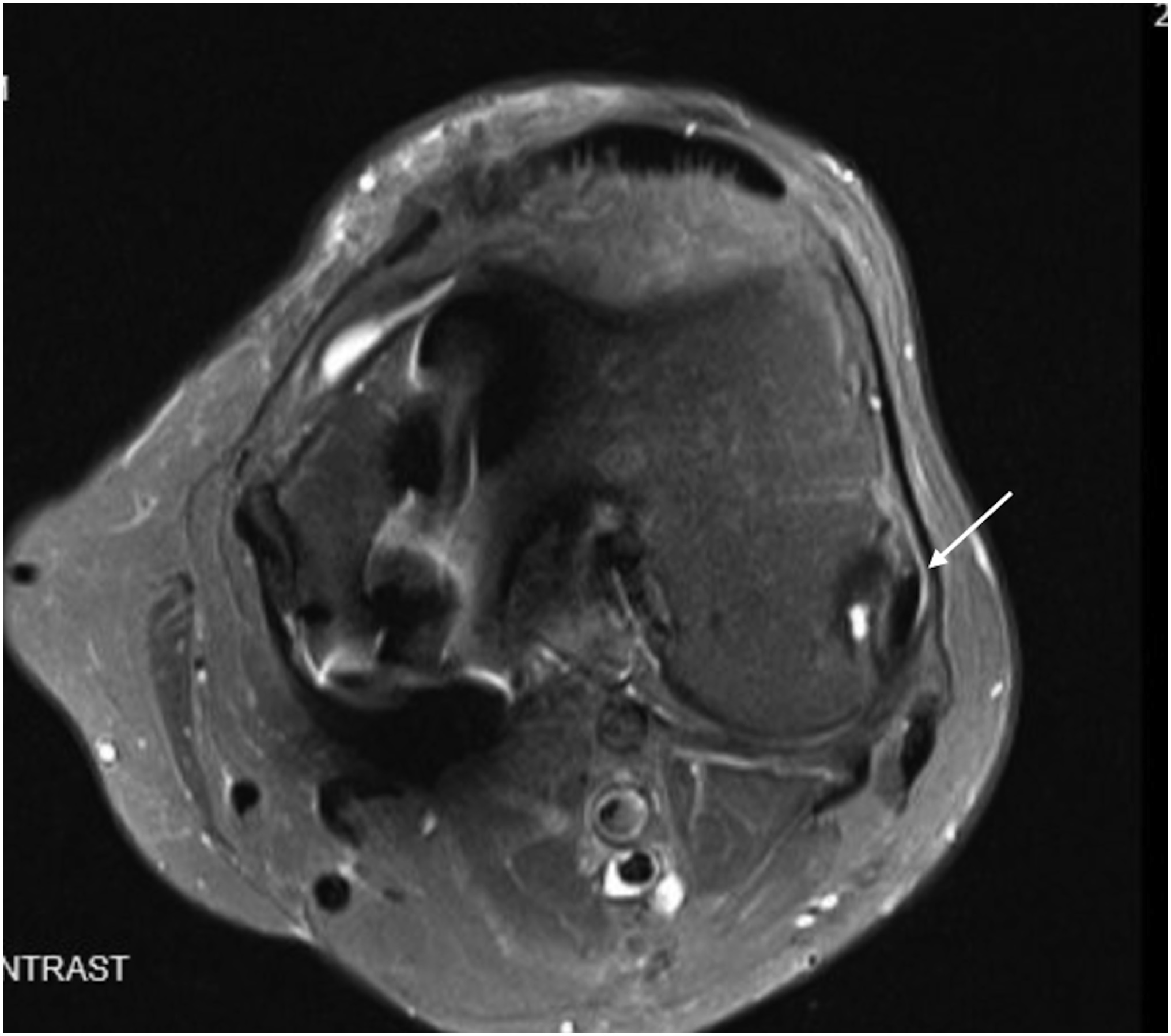
 Fig. 1-A
Fig. 1-A Fig. 1-B
Fig. 1-B Fig. 2-A
Fig. 2-A Fig. 2-B
Fig. 2-B Fig. 3-A
Fig. 3-A Fig. 3-B
Fig. 3-B Fig. 3-C
Fig. 3-C Fig. 4-A
Fig. 4-A Fig. 4-B
Fig. 4-B Fig. 4-C
Fig. 4-C Fig. 4-D
Fig. 4-D Fig. 4-E
Fig. 4-E