A 61-year-old man presented to the emergency department with a sudden onset of atraumatic pain and swelling in the left knee that had lasted for 3 hours. His height was 175 cm, his weight was 74 kg, and he worked as a postman. He had undergone unicompartmental knee arthroplasty (UKA) 5 years previously and had been symptom-free and functioning well. A radiograph performed in the emergency department was interpreted as normal (Fig. 1). The patient was advised to return if he had persistent symptoms.
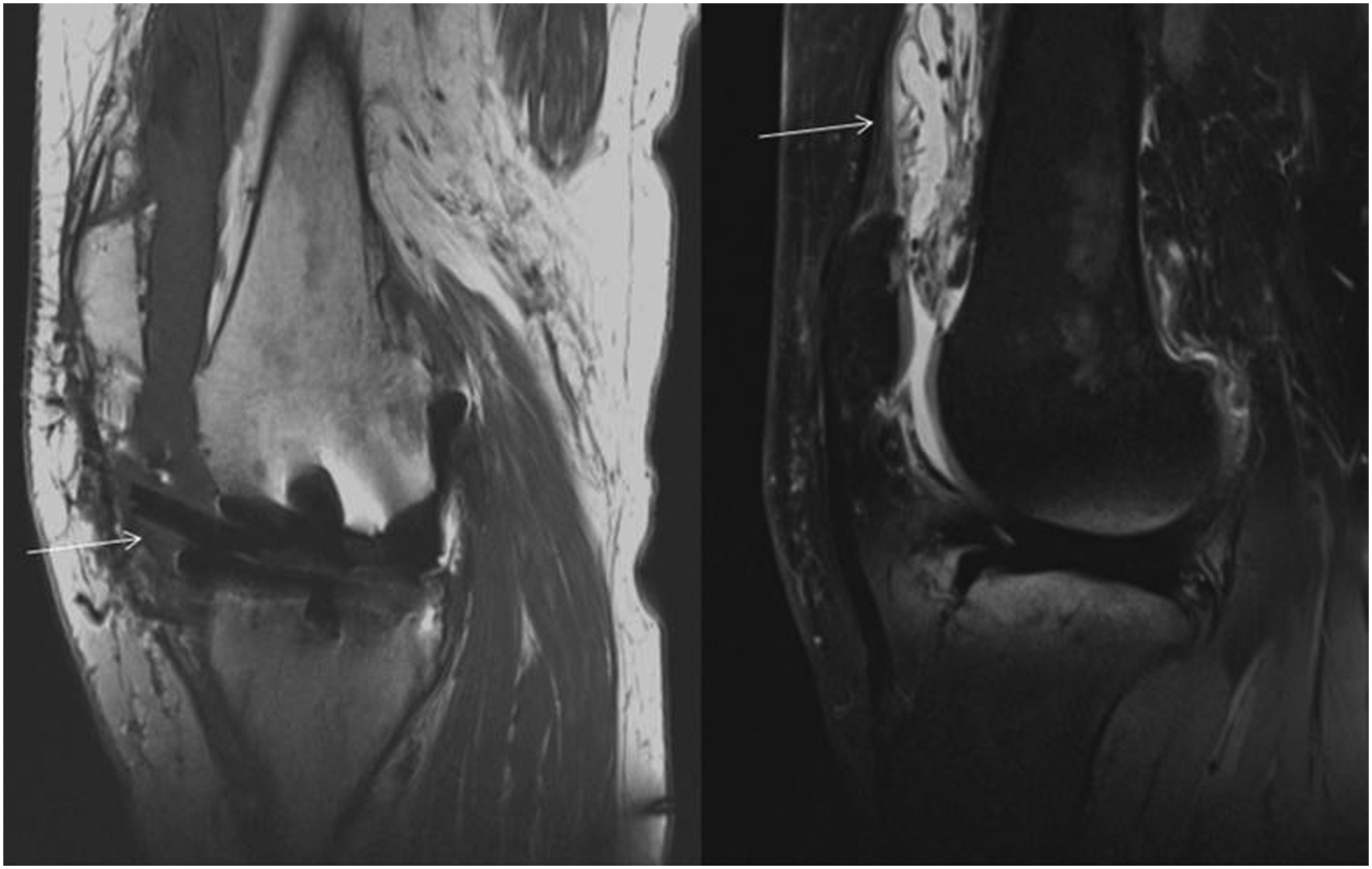
The patient returned to the clinic after 4 weeks with continued pain, swelling, and difficulty in bearing weight. A previous joint fluid aspiration was found to be aseptic. The initial radiograph was reviewed, and a dislocated polyethylene liner of the unicompartmental prosthesis was identified. Repeat radiographs showed a metal arthrogram with new curvilinear densities outlining the knee capsule and the Baker cyst (Fig. 2). These radiographs also delineated the dislocated fixed bearing. The immediate postoperative radiograph from his previous hospital was reviewed, and there was no evidence of malalignment. A magnetic resonance imaging (MRI) scan showed an effusion and thickened synovium with a diffusely low signal consistent with metallosis (Fig. 3). There was no osteolysis. The anterior cruciate ligament (ACL) was intact.
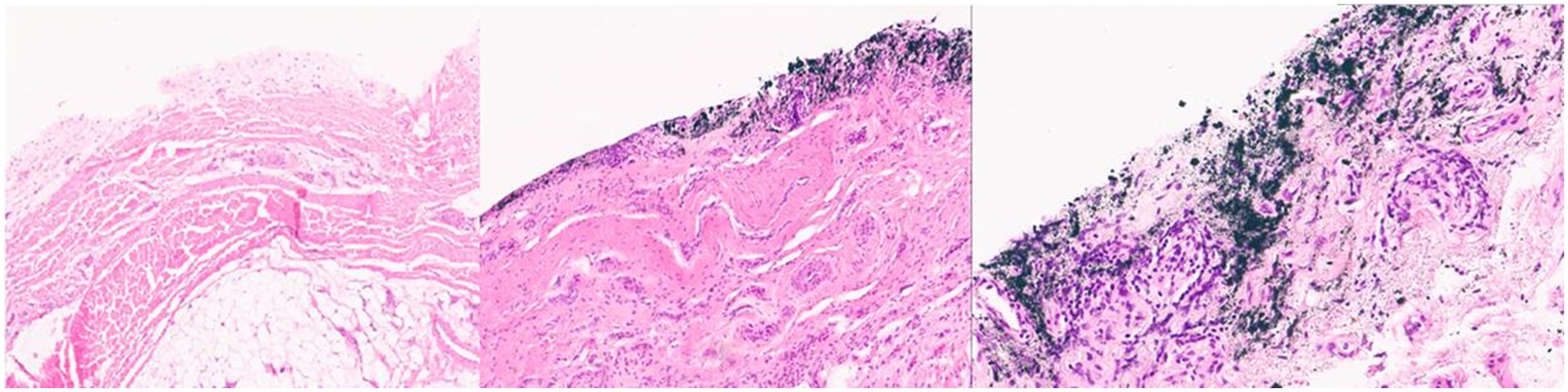
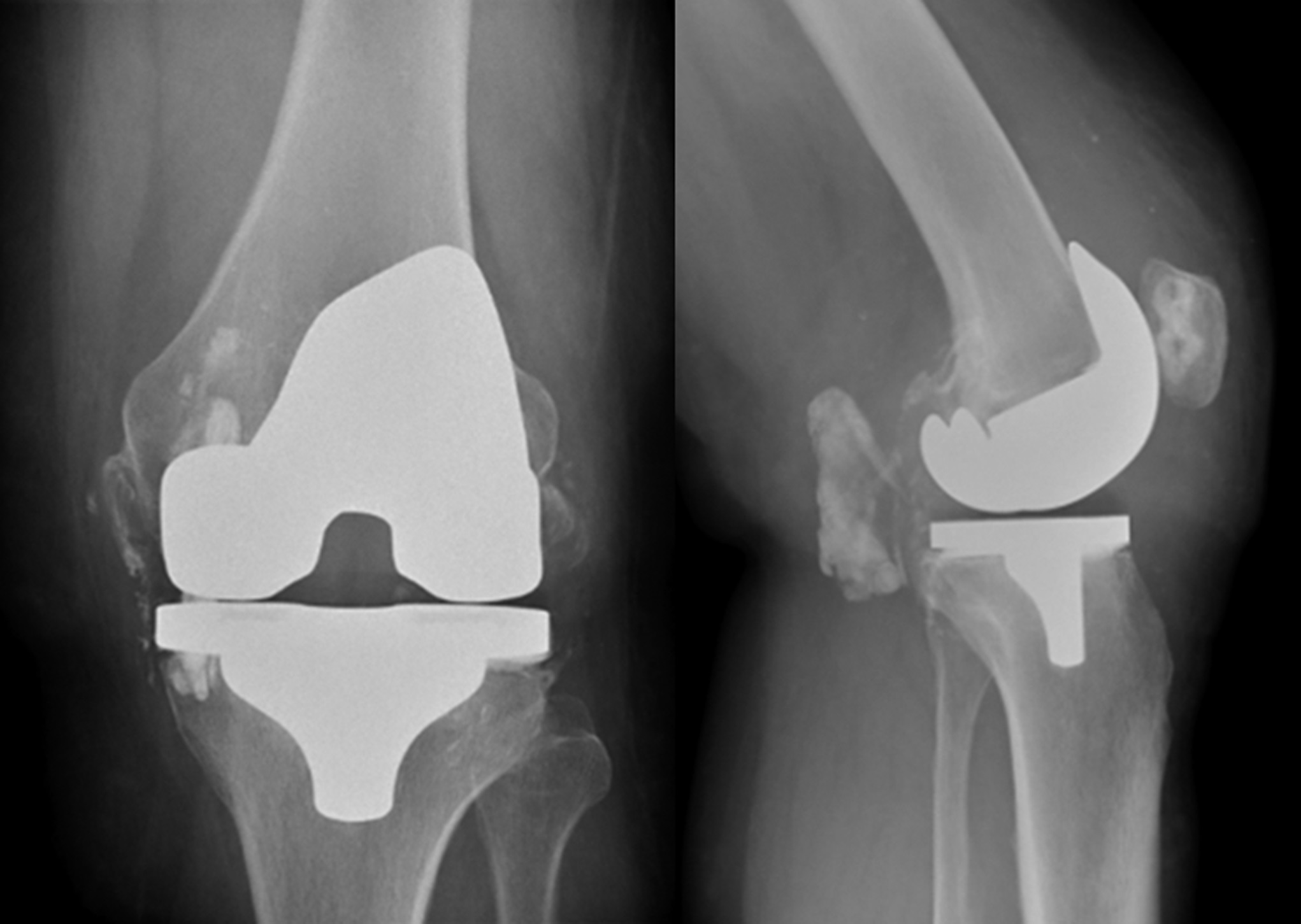
Intraoperatively, substantial synovial metallosis was seen, and the ACL was found to be intact (Fig. 4). Thorough debridement was performed. The tissue samples were sent for culture and histopathology. The culture report showed no evidence of infection. Histopathology showed evidence of infiltration of metal debris over the synovium. The difference between normal synovium and metallosis in low and high magnification (×20) using a hematoxylin and eosin stain is shown in Figure 5. Substantial wear of the posterior aspect of the fixed bearing, damage to the locking mechanism, and wear of the femoral and tibial implants were noted (Fig. 6). The knee underwent revision to a Triathlon (Stryker) cruciate-retaining total knee replacement (Fig. 7). The patient was reviewed at 1 year and was functioning well at that time with a modified Oxford Knee Score of 39 of 48.
Proceed to Discussion >>Reference: Kiran M, Kho J, Hepburn E, Chakraverty J, Davies H. Chronic wear-induced bearing dislocation in a fixed-bearing unicompartmental knee arthroplasty: a case report. JBJS Case Connect. 2021 Sep;11(3).e21.00364.
There has been a substantial increase in the use of fixed-bearing medial UKAs, increasing from 30% in 2010 to 49% in 2018 in the United Kingdom. This increase may have been due to the reduced risk of bearing dislocation, improved wear characteristics of modern polyethylene bearings, and the perceived technical ease of the surgical procedure. However, polyethylene wear is a common cause of failure in fixed-bearing designs. The mean penetrative wear rate in fixed-bearing UKAs is 0.15 mm/yr compared with 0.04 mm/yr in mobile-bearing UKAs. This wear may offset the potential benefit of bearing stability in fixed-bearing designs and also cause bearing dislocation as described earlier. The wear in fixed-bearing UKA occurs because of higher surface deformation and delamination. Malpositioned components, polyethylene thickness of <6 mm, old manufacturing and sterilization methods, and reduced conformity of design are associated with increased polyethylene wear. The implant in this patient was made of ceramicized titanium nitride, which has low wear when in contact with the polyethylene bearing but can wear rapidly if contact occurs between the metallic components, as evidenced by the rapid onset of metallosis. Therefore, wear in fixed-bearing UKAs may be related to the failure of material properties of the components or technical failure with malalignment of components.
There are 3 types of locking mechanisms in fixed-bearing designs, namely, linear, peripheral, and central. The peripheral locking mechanism is commonly used in fixed-bearing UKAs. Dislocation due to incorrect bearing insertion, repetitive micromotion between base plate and bearing due to the failure of liner locking mechanism, and posterior cruciate ligament tightness causing damage to the posterior locking mechanism and anterior liftoff have been described in fixed-bearing total knee arthroplasties (TKAs). This may cause backside wear, liner dissociation and articulation of metal components, patellar tendon damage, extensor lag, substantial metallosis, and fracture of the tibial base plate in fixed-bearing TKAs. However, liner dislocation is uncommon in fixed-bearing UKAs. Mobile-bearing liners have radiological markers that clearly demonstrate dislocation. By contrast, the absence of a radiological marker in fixed-bearing liners and the rarity of dislocation in fixed-bearing UKAs may have contributed to missing the diagnosis in the initial radiograph. The diagnosis requires careful examination of the lateral radiograph for signs of bearing displacement, which is made difficult because of the radiolucent nature of the insert. Narrowing or asymmetry of the joint space in comparison with previous imaging, if available, and contact between the femoral and tibial components are also potential indicators of bearing dislocation in fixed-bearing UKAs.
A metal arthrogram indicates major component damage and consequent metallosis within the soft tissue. Weissman et al. described the metal-line sign as “a thin curvilinear white line outlining the knee capsule” in patients with metallosis after TKA. Metallosis is often described in the literature as a consequence of liner wear over a long time. Sanchis-Alfonso described severe metallosis and polyethylene debris-induced osteolysis in a fixed-bearing UKA, with substantial liner wear and contact between the tibial and femoral components over a period of 4 years, without liner dislocation. Similar to our patient, he noted that the complete removal of metallosis from the soft tissues surrounding the knee was not possible. He suggested that progressive liner wear resulted in ACL insufficiency and instability, which further perpetuated the liner wear. By contrast, in our patient, the ACL was found to be intact on MRI and intraoperatively, suggesting that contact between tibial and femoral components due to the bearing dislocation resulted in metallosis over a short period of time. This is further evidenced by the lack of metallosis in the initial radiograph. Therefore, early recognition of liner wear and dislocation may avert the occurrence of metallosis and may result in a simple bearing revision or revision to UKA compared with a radical debridement and revision to TKA, as performed for our patient.
To the best of our knowledge, this was the first case of rapid-onset severe metallosis due to liner wear, failure of locking mechanism, and liner dislocation in a fixed-bearing UKA. Early recognition of dislocation on radiographs may prevent the occurrence of severe metallosis and soft-tissue damage.
Reference: Kiran M, Kho J, Hepburn E, Chakraverty J, Davies H. Chronic wear-induced bearing dislocation in a fixed-bearing unicompartmental knee arthroplasty: a case report. JBJS Case Connect. 2021 Sep;11(3).e21.00364.
What is the diagnosis?
Aseptic loosening
Transmural wear of tibial polyethylene
Clostridium periprosthetic infection
Ruptured patella tendon
Dislocated polyethylene liner

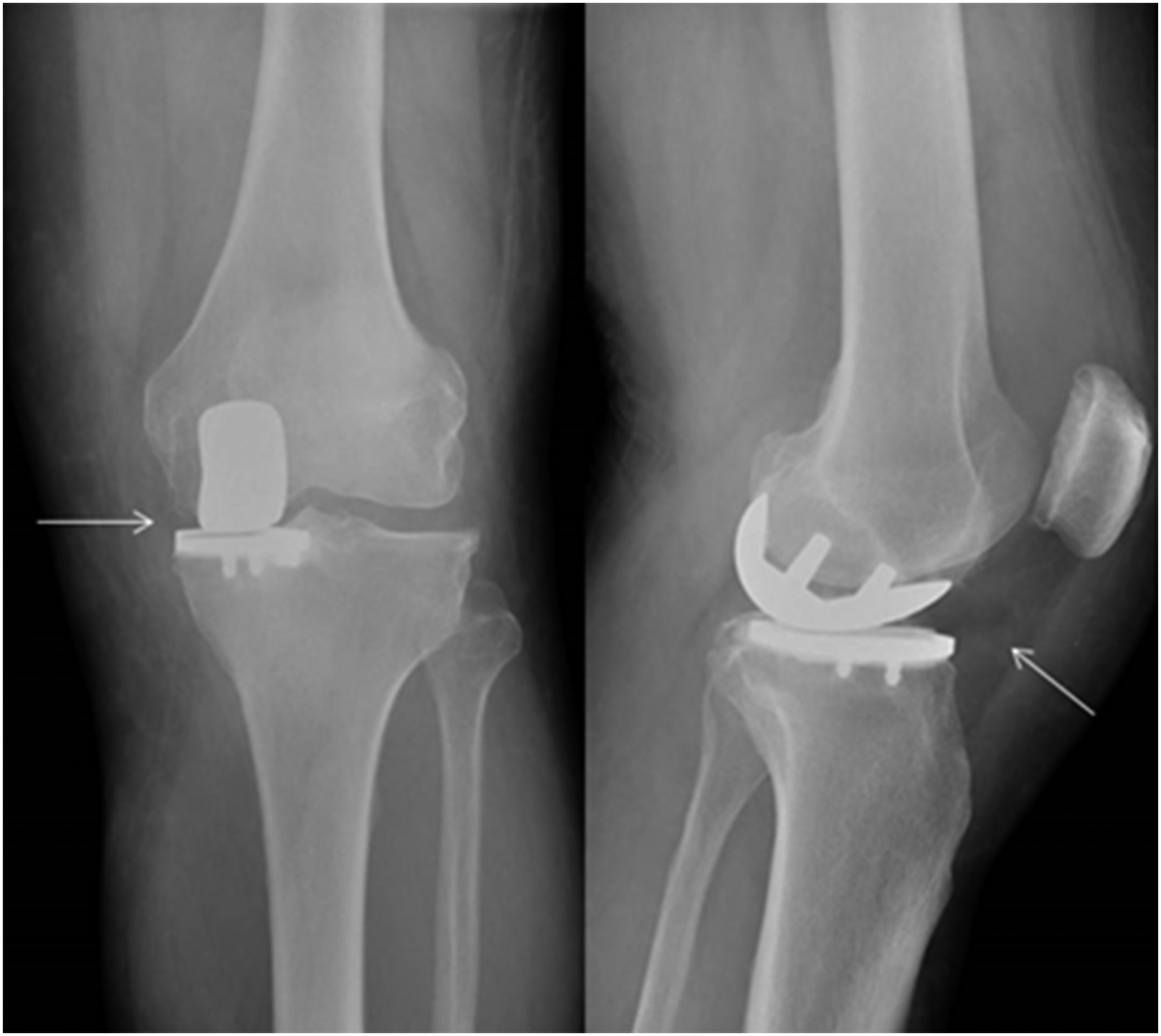
 Fig. 1
Fig. 1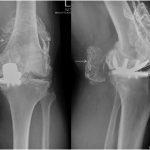 Fig. 2
Fig. 2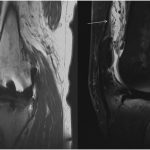 Fig. 3
Fig. 3 Fig. 4
Fig. 4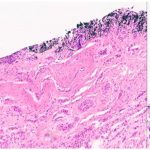 Fig. 5
Fig. 5 Fig. 6
Fig. 6 Fig. 7
Fig. 7